Opioid: Difference between revisions
CSV import |
No edit summary |
||
| Line 1: | Line 1: | ||
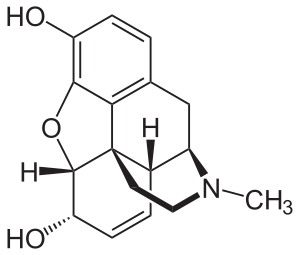
[[File:Morphin - Morphine.svg|thumb|right|Chemical structure of morphine, the prototypical natural opioid]] | |||
[[File:Opioid dependence.webm|thumb|left|Animation explaining opioid dependence]] | |||
[[File:Opiates v opioids.png|thumb|right|Diagram distinguishing between opiates (naturally derived) and opioids (including synthetic and semi-synthetic)]] | |||
[[File:Morphine structure.svg|thumb|left|Detailed molecular structure of morphine]] | |||
[[File:INTA.svg|thumb|right|INTERNATIONAL NARCOTICS CONTROL BOARD emblem related to opioid regulation]] | |||
[[File:Raw opium.jpg|thumb|left|Photograph of raw opium, the natural source of opiate alkaloids]] | |||
[[File:US timeline. Prescription opioid pain reliever deaths.jpg|thumb|right|Timeline of prescription opioid painkiller-related deaths in the U.S.]] | |||
[[File:Adrenorphin slim.svg|thumb|left|Structure of adrenorphin, an endogenous opioid peptide]] | |||
[[File:Amidorphin.svg|thumb|right|Chemical structure of amidorphin, a naturally occurring opioid]] | |||
[[File:Bovine β-casomorphin 7.svg|thumb|left|Structure of bovine β-casomorphin-7, a food-derived opioid peptide]] | |||
[[File:2-D-Alanine-5-D-leucine-enkephalin.png|thumb|right|Chemical structure of synthetic enkephalin analogue: D-Ala2-D-Leu5 enkephalin]] | |||
[[File:DAMGO.svg|thumb|left|DAMGO, a selective μ-opioid receptor agonist used in research]] | |||
'''Opioids''' are a class of drugs that bind to [[opioid receptors]] in the [[central nervous system]], [[peripheral nervous system]], and [[gastrointestinal tract]] to produce a range of effects including analgesia (pain relief), euphoria, sedation, and respiratory depression. | |||
== | == Terminology == | ||
While often used interchangeably, the term '''[[opiate]]''' technically refers only to the naturally occurring alkaloids derived from [[opium]] (e.g., [[morphine]], [[codeine]]), whereas '''opioid''' includes all compounds—natural, semi-synthetic (e.g., [[heroin]], [[oxycodone]]), and fully synthetic (e.g., [[fentanyl]], [[methadone]])—that act on opioid receptors. | |||
'' | == Classification == | ||
Opioids are categorized into: | |||
* '''Endogenous peptides''': Naturally produced in the body (e.g., [[endorphin]]s, [[enkephalin]]s) | |||
* '''Natural opiates''': Derived directly from the opium poppy (e.g., morphine, codeine) | |||
* '''Semi-synthetic opioids''': Chemically modified natural opiates (e.g., oxycodone, heroin) | |||
* '''Synthetic opioids''': Fully synthetic compounds (e.g., fentanyl, methadone) | |||
== Pharmacology == | |||
'''Main article: [[Opioid receptor]]''' | |||
'' | |||
Opioids exert their effects by binding to [[G-protein coupled receptor]]s: | |||
* '''μ (mu) receptor''': Analgesia, euphoria, respiratory depression, physical dependence | |||
* '''κ (kappa) receptor''': Spinal analgesia, sedation, dysphoria | |||
* '''δ (delta) receptor''': Analgesia and mood modulation | |||
* '''NOP receptor''': Binds [[nociceptin]], not reversed by naloxone | |||
== Clinical Use == | |||
Opioids are widely prescribed for: | |||
* Acute pain (post-operative, trauma) | |||
* Chronic pain (cancer, palliative care) | |||
* Cough suppression (codeine) | |||
* Diarrhea treatment (loperamide, diphenoxylate) | |||
* Opioid dependence treatment (methadone, buprenorphine) | |||
* Anesthesia adjuncts (fentanyl) | |||
* [[ | == Adverse Effects == | ||
* [[ | * Common: [[Constipation]], nausea, drowsiness, pruritus, [[miosis]], respiratory depression | ||
* Serious: [[Overdose]], [[addiction]], [[immunosuppression]], [[endocrine disruption]] | |||
== Tolerance, Dependence, and Addiction == | |||
* '''Tolerance''': Reduced effect over time, requiring dose escalation | |||
* '''Dependence''': Withdrawal symptoms upon cessation | |||
* '''Addiction''': Compulsive use despite harm | |||
[ | == Overdose Management == | ||
* Reversed by opioid antagonists such as: | |||
** [[Naloxone]] (Narcan) | |||
** [[Naltrexone]] | |||
These agents outcompete opioids at receptors without activating them. | |||
[ | == Endogenous Opioids == | ||
Produced by the body, they modulate pain, stress, and emotions. | |||
* [[Endorphins]] | |||
* [[Enkephalins]] | |||
* [[Dynorphins]] | |||
* [[Endomorphins]] | |||
* [[Nociceptin]] | |||
== Opioid Epidemic == | |||
The U.S. and several countries face an ongoing public health crisis due to overprescription and illicit use. Factors include: | |||
* Increased prescribing in the 1990s–2000s | |||
* Rise of synthetic opioids (fentanyl) | |||
* Socioeconomic and mental health components | |||
== Recreational Use == | |||
Non-medical use of opioids can cause intense euphoria, making them highly addictive. Long-term abuse leads to: | |||
* Tolerance | |||
* Physical and psychological dependence | |||
* Risk of fatal overdose | |||
== History == | |||
Opioids have been used since ancient times. The 20th century saw regulatory acts (e.g., Harrison Narcotics Act 1914), followed by the rise of synthetic opioids and ongoing debates over pain management vs. addiction risk. | |||
== Examples == | |||
=== Natural Alkaloids === | |||
* [[Morphine]] | * [[Morphine]] | ||
* [[Codeine]] | * [[Codeine]] | ||
* [[Thebaine]] | * [[Thebaine]] | ||
=== Semi-Synthetic === | |||
* [[Heroin]] | |||
=== | |||
* [[ | |||
* [[Oxycodone]] | * [[Oxycodone]] | ||
* [[Hydromorphone]] | * [[Hydromorphone]] | ||
=== Synthetic === | |||
* [[Fentanyl]] | |||
* [[Methadone]] | * [[Methadone]] | ||
* [[Tramadol]] | * [[Tramadol]] | ||
* [[Loperamide]] | * [[Loperamide]] | ||
=== Antagonists === | |||
* [[Naloxone]] | * [[Naloxone]] | ||
* [[Naltrexone]] | * [[Naltrexone]] | ||
== | == See Also == | ||
* [[Opioid receptor]] | |||
* [[Opioid epidemic]] | |||
* [[Analgesic]] | |||
* [[Substance use disorder]] | |||
* [[Endorphins]] | |||
* [[Naloxone]] | |||
* [[Chronic pain]] | |||
{{Antiaddictives}} | {{Antiaddictives}} | ||
{{Analgesics}} | {{Analgesics}} | ||
{{Drug use}} | {{Drug use}} | ||
{{Euphoriants}} | {{Euphoriants}} | ||
{{Opioidergics}} | {{Opioidergics}} | ||
}} | {{stub}} | ||
[[Category:Opioids | |||
[[Category:Opioids]] | |||
[[Category:Pain management]] | |||
[[Category:Morphine]] | [[Category:Morphine]] | ||
[[Category: | [[Category:Analgesics]] | ||
[[Category:Substance-related disorders]] | |||
[[Category:Neurological disorders]] | |||
Latest revision as of 02:57, 22 March 2025










Opioids are a class of drugs that bind to opioid receptors in the central nervous system, peripheral nervous system, and gastrointestinal tract to produce a range of effects including analgesia (pain relief), euphoria, sedation, and respiratory depression.
Terminology[edit]
While often used interchangeably, the term opiate technically refers only to the naturally occurring alkaloids derived from opium (e.g., morphine, codeine), whereas opioid includes all compounds—natural, semi-synthetic (e.g., heroin, oxycodone), and fully synthetic (e.g., fentanyl, methadone)—that act on opioid receptors.
Classification[edit]
Opioids are categorized into:
- Endogenous peptides: Naturally produced in the body (e.g., endorphins, enkephalins)
- Natural opiates: Derived directly from the opium poppy (e.g., morphine, codeine)
- Semi-synthetic opioids: Chemically modified natural opiates (e.g., oxycodone, heroin)
- Synthetic opioids: Fully synthetic compounds (e.g., fentanyl, methadone)
Pharmacology[edit]
Main article: Opioid receptor
Opioids exert their effects by binding to G-protein coupled receptors:
- μ (mu) receptor: Analgesia, euphoria, respiratory depression, physical dependence
- κ (kappa) receptor: Spinal analgesia, sedation, dysphoria
- δ (delta) receptor: Analgesia and mood modulation
- NOP receptor: Binds nociceptin, not reversed by naloxone
Clinical Use[edit]
Opioids are widely prescribed for:
- Acute pain (post-operative, trauma)
- Chronic pain (cancer, palliative care)
- Cough suppression (codeine)
- Diarrhea treatment (loperamide, diphenoxylate)
- Opioid dependence treatment (methadone, buprenorphine)
- Anesthesia adjuncts (fentanyl)
Adverse Effects[edit]
- Common: Constipation, nausea, drowsiness, pruritus, miosis, respiratory depression
- Serious: Overdose, addiction, immunosuppression, endocrine disruption
Tolerance, Dependence, and Addiction[edit]
- Tolerance: Reduced effect over time, requiring dose escalation
- Dependence: Withdrawal symptoms upon cessation
- Addiction: Compulsive use despite harm
Overdose Management[edit]
- Reversed by opioid antagonists such as:
- Naloxone (Narcan)
- Naltrexone
These agents outcompete opioids at receptors without activating them.
Endogenous Opioids[edit]
Produced by the body, they modulate pain, stress, and emotions.
Opioid Epidemic[edit]
The U.S. and several countries face an ongoing public health crisis due to overprescription and illicit use. Factors include:
- Increased prescribing in the 1990s–2000s
- Rise of synthetic opioids (fentanyl)
- Socioeconomic and mental health components
Recreational Use[edit]
Non-medical use of opioids can cause intense euphoria, making them highly addictive. Long-term abuse leads to:
- Tolerance
- Physical and psychological dependence
- Risk of fatal overdose
History[edit]
Opioids have been used since ancient times. The 20th century saw regulatory acts (e.g., Harrison Narcotics Act 1914), followed by the rise of synthetic opioids and ongoing debates over pain management vs. addiction risk.
Examples[edit]
Natural Alkaloids[edit]
Semi-Synthetic[edit]
Synthetic[edit]
Antagonists[edit]
See Also[edit]


