Cephaloridine: Difference between revisions
No edit summary Tag: Manual revert |
|
| (One intermediate revision by the same user not shown) | |
(No difference)
| |
Latest revision as of 14:51, 1 April 2025
Chemical compound
| Cephaloridine | |
|---|---|
| |
| INN | |
| Drug class | |
| Routes of administration | |
| Pregnancy category | |
| Bioavailability | |
| Metabolism | |
| Elimination half-life | |
| Excretion | Renal |
| Legal status | |
| CAS Number | 50-59-9 |
| PubChem | 5773 |
| DrugBank | DB09008 |
| ChemSpider | 5569 |
| KEGG | D01075 |
Cephaloridine is a first-generation Cephalosporin antibiotic, introduced in the 1960s. It is a beta-lactam antibiotic similar in structure and mechanism of action to penicillins. Cephaloridine was developed for the treatment of bacterial infections due to its effectiveness against a broad range of Gram-positive bacteria and some Gram-negative bacteria. However, its use has declined over the years due to the development of newer antibiotics with fewer side effects and broader antimicrobial activities.
Chemical Structure and Mechanism of Action[edit]
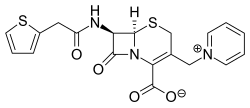
Cephaloridine's chemical structure is characterized by a beta-lactam ring, which is essential for its antibacterial activity. The mechanism of action of cephaloridine involves the inhibition of bacterial cell wall synthesis. It binds to specific penicillin-binding proteins (PBPs) located inside the bacterial cell wall, leading to the disruption of cell wall synthesis and ultimately causing cell lysis and death.
Pharmacokinetics[edit]
The pharmacokinetics of cephaloridine involve its absorption, distribution, metabolism, and excretion. After administration, cephaloridine is not well absorbed from the gastrointestinal tract and is therefore usually administered via intramuscular or intravenous injection. It is distributed throughout the body, including in the kidneys, liver, and lungs. Cephaloridine is excreted primarily by the kidneys through glomerular filtration.
Clinical Uses[edit]
Cephaloridine was primarily used to treat infections caused by susceptible bacteria, including respiratory tract infections, skin and soft tissue infections, urinary tract infections, and bone and joint infections. Its use has been largely superseded by newer cephalosporins and other antibiotics that have a broader spectrum of activity and are less nephrotoxic.
Side Effects and Toxicity[edit]
The most significant adverse effect associated with cephaloridine is nephrotoxicity, which can lead to kidney damage, particularly at high doses or in patients with pre-existing kidney impairment. Other side effects may include allergic reactions, ranging from rash to anaphylaxis, as well as gastrointestinal disturbances such as nausea, vomiting, and diarrhea.
Current Status[edit]
Due to its nephrotoxic effects and the availability of safer, more effective antibiotics, the use of cephaloridine has decreased significantly and it is no longer widely used in clinical practice. Research into cephalosporins has continued, leading to the development of several generations of these antibiotics, each with improved spectra of activity and safety profiles.
| Xenobiotic-sensing receptor modulators | ||||
|---|---|---|---|---|
;See also
|
| This article is a stub. You can help WikiMD by registering to expand it. |
| Types of antibacterials | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|