Methylprednisolone: Difference between revisions
No edit summary |
en>Kupirijo →Available forms: Methylprednisolone aceponate |
||
| Line 1: | Line 1: | ||
{{ | {{Short description|Corticosteroid medication}} | ||
{{Use dmy dates|date=March 2022}} | |||
{{cs1 config |name-list-style=vanc |display-authors=6}} | |||
{{Infobox drug | |||
| verifiedrevid = 4771699945 | |||
| image = Methylprednisolone.svg | |||
| image_class = skin-invert-image | |||
| width = 250 | |||
| alt = | |||
| caption = | |||
| image2 = Methylprednisolone.png | |||
| image_class2 = bg-transparent | |||
| width2 = 215 | |||
| alt2 = | |||
== | <!-- Clinical data --> | ||
| pronounce = | |||
| tradename = Medrol, others | |||
| Drugs.com = {{drugs.com|monograph|methylprednisolone}} | |||
| MedlinePlus = a682795 | |||
| DailyMedID = Methylprednisolone | |||
| pregnancy_AU = A | |||
| pregnancy_AU_comment = <ref name="Drugs.com pregnancy">{{cite web | title=Methylprednisolone Use During Pregnancy | website=Drugs.com | date=20 August 2019 | url=https://www.drugs.com/pregnancy/methylprednisolone.html | access-date=20 February 2020}}</ref> | |||
| pregnancy_category = | |||
| routes_of_administration = [[Oral administration|By mouth]], [[intramuscular]], [[intra-articular]], [[intravenous]] | |||
| class = | |||
| ATC_prefix = D07 | |||
| ATC_suffix = AA01 | |||
| ATC_supplemental = {{ATC|D07|AC14}}, {{ATC|D10|AA02}}, {{ATC|H02|AB04}}, {{ATC|D07|CA02}}, {{ATC|S01|CA08}}, {{ATC|H02|BX01}}, {{ATC|S03|CA07}} | |||
<!-- Legal status --> | |||
| legal_AU = <!-- S2, S3, S4, S5, S6, S7, S8, S9 or Unscheduled --> | |||
| legal_AU_comment = | |||
| legal_BR = <!-- OTC, A1, A2, A3, B1, B2, C1, C2, C3, C4, C5, D1, D2, E, F --> | |||
| legal_BR_comment = | |||
| legal_CA = Rx-only | |||
| legal_CA_comment = <ref>{{cite web | title=Product monograph brand safety updates | website=[[Health Canada]] | date=7 July 2016 | url=https://www.canada.ca/en/health-canada/services/drugs-health-products/drug-products/drug-product-database/label-safety-assessment-update/product-monograph-brand-safety-updates.html | access-date=3 April 2024}}</ref> | |||
| legal_DE = <!-- Anlage I, II, III or Unscheduled --> | |||
| legal_DE_comment = | |||
| legal_NZ = <!-- Class A, B, C --> | |||
| legal_NZ_comment = | |||
| legal_UK = POM | |||
| legal_UK_comment = | |||
| legal_US = Rx-only | |||
| legal_US_comment = | |||
| legal_EU = Rx-only | |||
| legal_EU_comment = <ref>{{cite web|url=https://www.ema.europa.eu/documents/psusa/methylprednisolone-list-nationally-authorised-medicinal-products-psusa/00002026/202011_en.pdf|title=List of nationally authorised medicinal products: Active substance: methylprednisolone: Procedure no. PSUSA/00002026/202011|website=[[European Medicines Agency]] (EMA)|access-date=12 March 2022}}</ref> | |||
| legal_UN = <!-- N I, II, III, IV / P I, II, III, IV --> | |||
| legal_UN_comment = | |||
| legal_status = <!-- For countries not listed above --> | |||
== | <!-- Pharmacokinetic data --> | ||
| bioavailability = | |||
| protein_bound = 78% | |||
| metabolism = [[Liver]] primarily, [[kidney]], [[tissue (biology)|tissue]]s; [[CYP3A4]] | |||
| metabolites = | |||
| onset = | |||
| elimination_half-life = 1.8–2.6 hours | |||
| duration_of_action = | |||
| excretion = [[Urine]] | |||
Methylprednisolone | <!-- Identifiers --> | ||
| CAS_number_Ref = {{cascite|correct|??}} | |||
| CAS_number = 83-43-2 | |||
| CAS_supplemental = | |||
| PubChem = 6741 | |||
| IUPHAR_ligand = 7088 | |||
| DrugBank_Ref = {{drugbankcite|correct|drugbank}} | |||
| DrugBank = DB00959 | |||
| ChemSpiderID_Ref = {{chemspidercite|correct|chemspider}} | |||
| ChemSpiderID = 6485 | |||
| UNII_Ref = {{fdacite|correct|FDA}} | |||
| UNII = X4W7ZR7023 | |||
| KEGG_Ref = {{keggcite|correct|kegg}} | |||
| KEGG = D00407 | |||
| ChEBI_Ref = {{ebicite|correct|EBI}} | |||
| ChEBI = 6888 | |||
| ChEMBL_Ref = {{ebicite|correct|EBI}} | |||
| ChEMBL = 650 | |||
| NIAID_ChemDB = | |||
| PDB_ligand = | |||
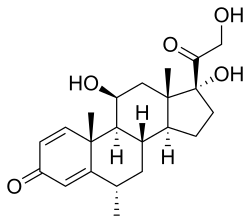
| synonyms = 6α-Methylprednisolone; 11β,17,21-trihydroxy-6α-methyl-δ<sup>1</sup>-progesterone; 11β,17,21-Trihydroxy-6α-methylpregna-1,4-diene-3,20-dione | |||
<!-- Chemical and physical data --> | |||
| IUPAC_name = (1''S'',2''R'',8''S'',10''S'',11''S'',14''R'',15''S'',17''S'')-14,17-dihydroxy-14-(2-hydroxyacetyl)-2,8,15-trimethyltetracyclo[8.7.0.0<sup>2,7</sup>.0<sup>11,15</sup>]heptadeca-3,6-dien-5-one | |||
| C = 22 | |||
| H = 30 | |||
| O = 5 | |||
| SMILES = O=C\1\C=C/[C@]4(/C(=C/1)[C@@H](C)C[C@@H]2[C@@H]4[C@@H](O)C[C@@]3([C@@](O)(C(=O)CO)CC[C@@H]23)C)C | |||
| StdInChI_Ref = {{stdinchicite|correct|chemspider}} | |||
| StdInChI = 1S/C22H30O5/c1-12-8-14-15-5-7-22(27,18(26)11-23)21(15,3)10-17(25)19(14)20(2)6-4-13(24)9-16(12)20/h4,6,9,12,14-15,17,19,23,25,27H,5,7-8,10-11H2,1-3H3/t12-,14-,15-,17-,19+,20-,21-,22-/m0/s1 | |||
| StdInChI_comment = | |||
| StdInChIKey_Ref = {{stdinchicite|correct|chemspider}} | |||
| StdInChIKey = VHRSUDSXCMQTMA-PJHHCJLFSA-N | |||
| density = | |||
| density_notes = | |||
| melting_point = 228 | |||
| melting_high = 237 | |||
| melting_notes = | |||
| boiling_point = | |||
| boiling_notes = | |||
| solubility = 1.20x10+2 | |||
| sol_units = | |||
| specific_rotation = | |||
}} | |||
== | <!-- Definition, medical uses, and side effects --> | ||
'''Methylprednisolone''' (Depo-Medrol, Medrol, Solu-Medrol) is a synthetic [[glucocorticoid]], primarily prescribed for its anti-inflammatory and immunosuppressive effects.<ref name="Katzung_2012">{{cite book|url=https://www.worldcat.org/oclc/761378641|title=Basic & clinical pharmacology|date=2012|publisher=McGraw-Hill Medical| vauthors = Katzung BG, Masters SB, Trevor AJ |isbn=978-0-07-176401-8|edition=12th|location=New York|oclc=761378641}}</ref><ref name="Timmermans_2019">{{cite journal | vauthors = Timmermans S, Souffriau J, Libert C | title = A General Introduction to Glucocorticoid Biology | language = English | journal = Frontiers in Immunology | volume = 10 | pages = 1545 | date = 2019 | pmid = 31333672 | pmc = 6621919 | doi = 10.3389/fimmu.2019.01545 | doi-access = free }}</ref><ref name="Xavier_2016">{{cite journal | vauthors = Xavier AM, Anunciato AK, Rosenstock TR, Glezer I | title = Gene Expression Control by Glucocorticoid Receptors during Innate Immune Responses | language = English | journal = Frontiers in Endocrinology | volume = 7 | pages = 31 | date = 2016 | pmid = 27148162 | pmc = 4835445 | doi = 10.3389/fendo.2016.00031 | doi-access = free }}</ref> It is either used at low doses for chronic illnesses or used concomitantly at high doses during acute flares. Methylprednisolone and its derivatives can be administered orally or parenterally.<ref>{{cite book | vauthors = Ocejo A, Correa R | chapter = Methylprednisolone |date=2020 |url=http://www.ncbi.nlm.nih.gov/books/NBK544340/ | title = StatPearls |place=Treasure Island (FL)|publisher=StatPearls Publishing|pmid=31335060|access-date=10 November 2020 }}</ref> | |||
Regardless of the route of administration, methylprednisolone integrates systemically as exhibited by its effectiveness to quickly reduce inflammation during acute flares.<ref>{{cite journal | vauthors = Habib GS | title = Systemic effects of intra-articular corticosteroids | journal = Clinical Rheumatology | volume = 28 | issue = 7 | pages = 749–56 | date = July 2009 | pmid = 19252817 | doi = 10.1007/s10067-009-1135-x | s2cid = 5645348 }}</ref> It is associated with many adverse reactions that require [[Tapering (medicine)|tapering off]] the drug as soon as the disease is under control.<ref name="Paragliola_2017">{{cite journal | vauthors = Paragliola RM, Papi G, Pontecorvi A, Corsello SM | title = Treatment with Synthetic Glucocorticoids and the Hypothalamus-Pituitary-Adrenal Axis | journal = International Journal of Molecular Sciences | volume = 18 | issue = 10 | pages = 2201 | date = October 2017 | pmid = 29053578 | pmc = 5666882 | doi = 10.3390/ijms18102201 | doi-access = free }}</ref> Serious side effects include iatrogenic [[Cushing's syndrome]], hypertension, osteoporosis, diabetes, infection, and skin atrophy.<ref name="Paragliola_2017"/> | |||
<!-- Chemistry and MOA --> | |||
Chemically, methylprednisolone is a synthetic [[pregnane]] [[steroid hormone]] derived from [[hydrocortisone]] and [[prednisolone]]. It belongs to a class of synthetic glucocorticoids and more generally, [[corticosteroid]]s. It acts as a mineralocorticoid and glucocorticoid receptor agonist. In comparison to other exogenous glucocorticoids, methylprednisolone has a higher affinity to glucocorticoid receptors than to mineralocorticoid receptors. | |||
Glucocorticoid's name was derived after the discovery of their involvement in regulating carbohydrate metabolism.<ref name="Paragliola_2017"/> The cellular functions of glucocorticoids, such as methylprednisolone, are now understood to regulate homeostasis, metabolism, development, cognition, and inflammation.<ref name="Paragliola_2017"/> They play a critical role in adapting and responding to environmental, physical and emotional stress.<ref name="Paragliola_2017"/> | |||
<!-- History, society and culture --> | |||
Methylprednisolone was first synthesized and manufactured by [[Upjohn|The Upjohn Company]] (now [[Viatris]]) and [[Food and Drug Administration|FDA]] approved in the United States in October 1957.<ref name="U.S. Food and Drug Administration (FDA)">{{cite web|title=Drugs@FDA: FDA-Approved Drugs|url=https://www.accessdata.fda.gov/scripts/cder/daf/index.cfm?event=overview.process&ApplNo=011153|access-date=5 December 2020|website=U.S. [[Food and Drug Administration]] (FDA)}}</ref> In 2022, it was the 153rd most commonly prescribed medication in the United States, with more than 3{{nbsp}}million prescriptions.<ref name="The Top 300 of 2022">{{cite web | title=The Top 300 of 2022 | url=https://clincalc.com/DrugStats/Top300Drugs.aspx | website=ClinCalc | access-date=30 August 2024 | archive-date=30 August 2024 | archive-url=https://web.archive.org/web/20240830202410/https://clincalc.com/DrugStats/Top300Drugs.aspx | url-status=live }}</ref><ref name="ClinCalc Methylprednisolone">{{cite web | title = Methylprednisolone Drug Usage Statistics, United States, 2013 - 2022 | website = ClinCalc | url = https://clincalc.com/DrugStats/Drugs/Methylprednisolone | access-date = 30 August 2024 }}</ref> It is on the [[WHO Model List of Essential Medicines|World Health Organization's List of Essential Medicines]].<ref name="WHO23rd">{{cite book | vauthors = ((World Health Organization)) | title = The selection and use of essential medicines 2023: web annex A: World Health Organization model list of essential medicines: 23rd list (2023) | year = 2023 | hdl = 10665/371090 | author-link = World Health Organization | publisher = World Health Organization | location = Geneva | id = WHO/MHP/HPS/EML/2023.02 | hdl-access=free }}</ref> | |||
==Medical uses== | |||
The primary use of methylprednisolone is to suppress inflammatory and immune responses. Methylprednisolone achieves this primarily by regulating the number and function of leukocytes, cytokines, and chemokines.<ref name="Katzung_2012"/> Its widespread inflammatory control is conducive in use across multiple disorders regardless of pathology.<ref name="Katzung_2012"/> Methylprednisolone is commonly prescribed as short-term therapy for acute flares, as seen with acute gouty arthritis. It can be prescribed during on-going therapy in lower doses contingent upon monitorization of adverse effects.<ref name="Timmermans_2019"/> Dosage strength and formulation are optimized per medical use.<ref name="Xavier_2016"/> | |||
=== Asthma === | |||
In 2001–2002, 11.4% of patients diagnosed with asthma and seen at an outpatient visit were prescribed oral corticosteroids as a long-term control therapy.<ref>National Center for Health Statistics. Health, United States, 2004 With Chartbook on Trends in the Health of Americans. Hyattsville, Maryland: 2004 https://www.cdc.gov/nchs/data/hus/hus04.pdf</ref> The National Asthma Education and Prevention Program (NAEPP) indicates systemic methylprednisolone in both short and long-term therapies to quickly control and to suppress persistent asthma, respectively.<ref name="NAEPP_2007">{{cite journal | author = National Asthma Education and Prevention Program | title = Expert Panel Report 3 (EPR-3): Guidelines for the Diagnosis and Management of Asthma-Summary Report 2007 | journal = The Journal of Allergy and Clinical Immunology | volume = 120 | issue = 5 Suppl | pages = S94–138 | date = November 2007 | pmid = 17983880 | doi = 10.1016/j.jaci.2007.09.043 | url = https://www.nhlbi.nih.gov/sites/default/files/media/docs/EPR-3_Asthma_Full_Report_2007.pdf }}</ref> For exacerbations that result in a visit to the Emergency Department (ED), oral methylprednisolone is preferred over intravenous administration, unless there are issues with adherence or vomiting.<ref name="NAEPP_2007" /><ref name="Alangari_2010">{{cite journal | vauthors = Alangari AA | title = Genomic and non-genomic actions of glucocorticoids in asthma | journal = Annals of Thoracic Medicine | volume = 5 | issue = 3 | pages = 133–9 | date = July 2010 | pmid = 20835306 | pmc = 2930650 | doi = 10.4103/1817-1737.65040 | doi-access = free }}</ref> Oral methylprednisolone is less invasive and studies have shown that equivalent efficacy compared to intravenous methylprednisolone.<ref name="NAEPP_2007" /><ref name="Alangari_2010" /> Dosage above 60–80 mg/day or 2 mg/kg/day is not recommended as it has not been shown to alter pulmonary function, rate of admission, or length of stay in the hospital compared to lower doses.<ref name="Alangari_2010" /> Following ED discharge, it is advised to prescribe a five-day course of methylprednisolone to decrease the probability of relapse or withdrawal symptoms.<ref name="NAEPP_2007" /><ref name="Alangari_2010" /> | |||
=== Rheumatic diseases === | |||
Methylprednisolone is used to treat several rheumatic diseases, such as Systemic Lupus Erythematosus (SLE) and Rheumatoid Arthritis (RA). Methylprednisolone dosage and administration for these diseases is highly variable due to varied pathophysiology between the diseases and within patients diagnosed with a given disease.<ref name="Kaul_2016">{{cite journal | vauthors = Kaul A, Gordon C, Crow M, Touma Z, Urowitz MB, van Vollenhoven R, Ruiz-Irastorza G, Hughes G | title = Systemic lupus erythematosus. | journal = Nat Rev Dis Primers | volume = 2 | page = 16039 | date = 2016 | doi = 10.1038/nrdp.2016.39 | pmid = 27306639 | s2cid = 2628865 }}</ref><ref name="Chan_2015">{{cite journal | vauthors = Chan TM | title = Treatment of severe lupus nephritis: the new horizon | journal = Nature Reviews. Nephrology | volume = 11 | issue = 1 | pages = 46–61 | date = January 2015 | pmid = 25421826 | doi = 10.1038/nrneph.2014.215 | s2cid = 19814440 }}</ref> In Lupus Nephritis, a common manifestation of SLE, patients are often prescribed methylprednisolone concomitantly with immunosuppressants. Severe manifestations are often treated with [[Cyclophosphamide]] or [[Rituximab]] and three doses of methylprednisolone IV-pulse treatment (as recommended by ACR guidelines) before switching to oral prednisolone and azathioprine for maintenance.<ref name="Kaul_2016" /><ref name="Chan_2015" /> | |||
Intra-articular corticosteroid injections (IACI) are a second-line therapy to relieve joint pain resulting from rheumatoid arthritis.<ref name="Habib">Habib, G.S. Systemic effects of intra-articular corticosteroids. Clin. Rheumatol. 2009, 28, 749–756.</ref> It is most commonly injected into the joints of the knees and shoulders.<ref name="Habib" /> Although the injection is local, studies have shown systemic absorption as evidenced by beneficial effects on distant joints.<ref name="Habib" /> In an attempt to minimize HPA suppression, FDA guidelines have restricted IACIs to three per year, with a minimum of 30 days in between injections.<ref name="pmid25182149">{{cite journal | vauthors = Johnston PC, Lansang MC, Chatterjee S, Kennedy L | title = Intra-articular glucocorticoid injections and their effect on hypothalamic-pituitary-adrenal (HPA)-axis function | journal = Endocrine | volume = 48 | issue = 2 | pages = 410–6 | date = March 2015 | pmid = 25182149 | doi = 10.1007/s12020-014-0409-5 | s2cid = 207363039 }}</ref> | |||
=== Primary or secondary adrenocortical insufficiency === | |||
Methylprednisolone is not typically recommended for primary or secondary adrenocortical insufficiency compared to other corticosteroids which have a higher affinity for mineralocorticoid receptors and salt-retaining properties.<ref name="Katzung_2012"/> | |||
=== Labeled indications === | |||
The labeled indications below are categorized by route of administration and then by medical discipline. | |||
==== Oral methylprednisolone ==== | |||
* Allergy and immunology: [[Angioedema|angioneurotic edema]],<ref name="NAEPP_2007" /> [[asthma]], [[Hives|urticaria]], seasonal or perennial allergic rhinitis, drug hypersensitivity reactions, and [[serum sickness]].<ref name="Pfizer and Upjohn Company LLC_2019"/> | |||
* Dermatology: toxic epidermal necrolysis,<ref name="NAEPP_2007" /> [[atopic dermatitis]], [[contact dermatitis]], [[pemphigus]], [[erythema multiforme]], [[Stevens–Johnson syndrome|Steven-Johnson syndrome]], bullous dermatitis herpetiformis, severe [[Seborrhoeic dermatitis|seborrheic dermatitis]], exfoliative dermatitis, [[mycosis fungoides]], and severe [[psoriasis]].<ref name="Pfizer and Upjohn Company LLC_2019"/> | |||
* Endocrinology: [[congenital adrenal hyperplasia]], [[Hypercalcaemia|hypercalcemia associated with cancer]], nonsuppurative thyroiditis, and [[Adrenal insufficiency|primary or secondary adrenocortical insufficiency]].<ref name="Pfizer and Upjohn Company LLC_2019"/> | |||
* Gastroenterology: [[inflammatory bowel disease]] and [[ulcerative colitis]].<ref name="Pfizer and Upjohn Company LLC_2019"/> | |||
* Hematology: [[Autoimmune hemolytic anemia|acquired (autoimmune) hemolytic anemia]], [[Immune thrombocytopenic purpura|idiopathic thrombocytopenic purpura]], secondary thrombocytopenia, erythroblastopenia, [[leukemia]], [[lymphoma]] and congenital (erythroid) hypoplastic anemia.<ref name="Pfizer and Upjohn Company LLC_2019"/> | |||
* Pulmonary: [[Aspiration pneumonia|aspiration pneumonitis]], [[Berylliosis|chronic beryllium disease]], [[eosinophilic pneumonia]], symptomatic [[sarcoidosis]], and [[Tuberculosis|pulmonary tuberculosis]] in conjunction with antituberculosis chemotherapy.<ref name="Pfizer and Upjohn Company LLC_2019"/> | |||
* Nephrology: [[nephrotic syndrome]], idiopathic type or secondary to [[lupus nephritis]].<ref name="Pfizer and Upjohn Company LLC_2019"/> | |||
* Neurology: [[multiple sclerosis]].<ref name="Pfizer and Upjohn Company LLC_2019"/> | |||
* Ophthalmology: [[scleritis]], [[retinal vasculitis]],<ref name="NAEPP_2007" /> [[uveitis]], choroiditis, iritis, iridocyclitis, [[keratitis]], [[optic neuritis]], [[allergic conjunctivitis]], allergic corneal marginal ulcers, [[herpes zoster ophthalmicus]], [[sympathetic ophthalmia]], and chorioretinitis.<ref name="Pfizer and Upjohn Company LLC_2019"/> | |||
* Rheumatology: [[rheumatoid arthritis]], [[Rheumatic fever|rheumatic carditis]], [[Gout|acute gouty arthritis]], [[ankylosing spondylitis]], [[dermatomyositis]] and [[polymyositis]], [[psoriatic arthritis]], [[Lupus|systemic lupus erythematosus]], acute and subacute [[bursitis]], synovitis of osteoarthritis, post-traumatic osteoarthritis, and [[epicondylitis]].<ref name="Pfizer and Upjohn Company LLC_2019"/> | |||
* Miscellaneous: trichinosis with neurologic or myocardial involvement.<ref name="Pfizer and Upjohn Company LLC_2019"/> | |||
==== Parenteral methylprednisolone ==== | |||
* Intra-articular or soft tissue injections: acute gouty arthritis, acute and subacute bursitis, acute tenosynovitis, epicondylitis, and synovitis of osteoarthritis.<ref name="Chan_2015" /> | |||
* Intralesional injections: [[alopecia areata]], [[discoid lupus erythematosus]], [[keloid]]s, [[granuloma annulare]], [[lichen planus]], [[lichen simplex chronicus]], psoriatic plaques, [[Necrobiosis lipoidica|necrobiosis lipoidica diabeticorum]].<ref name="Chan_2015" /> | |||
* Intramuscular injections are prescribed to treat many of the same conditions indicated for oral administration. Intramuscular injections are administered as an alternative to oral therapy.<ref name="Chan_2015" /> | |||
=== Off-label indications === | |||
Some of the off-label indications of methylprednisolone include acute [[spinal cord injury]], [[acute respiratory distress syndrome]], [[alcoholic hepatitis]], hormonal resuscitation in cadaveric organ recovery, and [[chronic obstructive pulmonary disease]].<ref name="NAEPP_2007" /> | |||
=== Available forms === | |||
{{See also|Methylprednisolone acetate|Methylprednisolone succinate|Methylprednisolone aceponate}} | |||
{| class="wikitable" | |||
|+Available Forms of methylprednisolone<ref name="Pfizer and Upjohn Company LLC_2019"/><ref name="Chan_2015" /><ref name="Pfizer_2020"/> | |||
!Active Ingredient | |||
!Brand Name | |||
!ROA | |||
!Form | |||
!Strength<sup>1</sup> | |||
!Inactive Ingredients | |||
|- | |||
|methylprednisolone | |||
|Medrol | |||
|Oral | |||
|tablet | |||
|2, 4, 8, 16, 32 mg | |||
|calcium stearate, cornstarch, lactose, mineral oil, sorbic acid, sucrose, and erythrosine sodium (2 mg only), FD&C yellow No. 6 (8 and 32 mg only) | |||
|- | |||
|methylprednisolone | |||
|Medrol | |||
|Oral | |||
|tablet | |||
|4 mg; 21 pills (dose-pack) | |||
|calcium stearate, cornstarch, lactose, sucrose | |||
|- | |||
|methylprednisolone acetate | |||
|Depo-Medrol | |||
|Parenteral: | |||
intra-articular or soft tissue, intralesional or intramuscular | |||
|suspension | |||
|20, 40, 80 mg/ml | |||
|Polyethylene glycol 3350, Polysorbate 80, Monobasic sodium phosphate, Dibasic sodium phosphate USP, Benzyl alcohol<sup>2</sup> added as a preservative | |||
|- | |||
|methylprednisolone acetate<sup>3</sup> | |||
|Depo-Medrol | |||
|Parenteral: | |||
intra-articular or soft tissue, intralesional or intramuscular | |||
|suspension | |||
|40 or 80 mg/ml (single dose vial) | |||
|Polyethylene glycol 3350 | |||
Myristyl-gamma-picolinium chloride | |||
|- | |||
|methylprednisolone succinate | |||
|Solu-Medrol | |||
|Parenteral: | |||
intravenous or intramuscular | |||
|solution, reconstituted | |||
|500, 1000, 2000 mg/vial, 2000 mg with diluent (multi-dose vial) | |||
|monobasic sodium phosphate anhydrous, dibasic sodium phosphate dried, and lactose hydrous. Bacteriostatic water added as diluent with Benzyl alcohol<sup>2</sup> added as a preservative | |||
|- | |||
|methylprednisolone succinate<sup>3</sup> | |||
|Solu-Medrol | |||
|Parenteral: | |||
intravenous or intramuscular | |||
|solution, reconstituted | |||
|40, 125, 500, 1000 mg/vial (single dose vial) | |||
|monobasic sodium phosphate anhydrous, dibasic sodium phosphate dried, and lactose hydrous. | |||
|} | |||
Footnotes: | |||
<sup>1</sup>Signifies varying strengths of available forms. Is not indicative of frequency nor daily cumulative dose; varies per patient and condition. | |||
<sup>2</sup>Benzyl alcohol should not be used on neonates | |||
<sup>3</sup>Preservative free formulation | |||
== Contraindications == | |||
Methylprednisolone should not be taken orally by people who have systemic fungal infections, except for Depo-Medrol when administered as an intra-articular injection for localized joint conditions.<ref name="DEPO-MEDROL_label" /> Methylprednisolone is contraindicated in those with known hypersensitivity to methylprednisolone or its components<ref name="Pfizer and Upjohn Company LLC_2019"/> Steroids should be used with caution in patients with ulcerative colitis, heart disease or hypertension, peptic ulcer, renal insufficiency, osteoporosis, myasthenia gravis, glaucoma, and diabetes.<ref name="Katzung_2012"/><ref name="Pfizer and Upjohn Company LLC_2019"/> Psychic manifestations may appear while taking methylprednisolone, ranging from euphoria, insomnia, personality changes to depression. Caution is required for patients with predisposed psychoses, as psychotic tendencies may be exacerbated while taking corticosteroids.<ref name="Pfizer and Upjohn Company LLC_2019"/> | |||
Solu-Medrol 40 mg dosage contains lactose monohydrate produced from cow's milk; It should not be taken by anyone with known hypersensitivity to dairy products or its components.<ref name="Pfizer_2020"/> Severe medical events have been associated with epidural administration of Solu-Medrol and Depo-Medrol, including spinal cord infarction, paraplegia, quadriplegia, cortical blindness and stroke. Intramuscular injections should not be administered to those with idiopathic thrombocytopenic purpura. Formulations of Solu-Medrol and Depo-Medrol containing benzyl alcohol are contraindicated for use in premature infants.<ref name="Pfizer_2020"/> Exposure of neural tissue to excessive amounts of benzyl alcohol has been associated with toxicity and in rare events has resulted in death.<ref name="DEPO-MEDROL_label" /> | |||
== Adverse effects == | |||
[[File:Overview of glucocorticoid-associated side effects.png|left|thumb|641x641px|Overview of Methylprednisolone-associated side effects.]] | |||
Adverse reactions may overshadow the therapeutic effects of methylprednisolone.<ref name="Paragliola_2017"/> | |||
=== Central nervous system === | |||
There is minimal clinical diagnostic criteria to define the psychic adverse effects (PAE) associated with methylprednisolone use in patients with systemic lupus erythematosus (SLE).<ref name="Fietta_2009">{{cite journal | vauthors = Fietta P, Fietta P, Delsante G | title = Central nervous system effects of natural and synthetic glucocorticoids | journal = Psychiatry and Clinical Neurosciences | volume = 63 | issue = 5 | pages = 613–22 | date = October 2009 | pmid = 19788629 | doi = 10.1111/j.1440-1819.2009.02005.x | s2cid = 28778979 | doi-access = free }}</ref> The prevalence varies from 1.3 to 62% of adult treated patients.<ref name="Fietta_2009" /> The type and severity of neuropsychiatric symptoms also varies significantly between patients, with 33% of patients reporting mild to moderate PAE and 5-10% reporting severe PAE.<ref name="Fietta_2009" /> Methylprednisolone dose and duration have been implicated in PAE development. 20 mg/day of prednisone (16 mg/day of methylprednisolone) is the threshold dosage for PAE development agreed upon by many studies.<ref name="Fietta_2009" /> Short-term pulse IV therapy at high doses is associated with rapid onset of manic and hypomanic symptoms, whereas long-term therapy gives rise to depressive symptoms (suicide attempts infrequent).<ref name="Fietta_2009" /> PAE are reversible with treatment reduction or discontinuation.<ref name="Fietta_2009" /> | |||
=== Metabolic and endocrine === | |||
Iatrogenic Cushing's Syndrome is a direct complication of glucocorticoid therapy, and the most common cause of exogenous Cushing's Syndrome.<ref name="Hopkins_2005">{{cite journal | vauthors = Hopkins RL, Leinung MC | title = Exogenous Cushing's syndrome and glucocorticoid withdrawal | journal = Endocrinology and Metabolism Clinics of North America | volume = 34 | issue = 2 | pages = 371–84, ix | date = June 2005 | pmid = 15850848 | doi = 10.1016/j.ecl.2005.01.013 }}</ref> Clinical features of Cushing's Syndrome are inclusive of many adverse effects in glucocorticoid therapy.<ref name="Hopkins_2005" /> Traditional symptoms include weight gain, myopathy, osteoporosis, increased risk of infection, hypertension, and psychological effects. Fat deposition is centralized on the trunk, in between shoulders ("buffalo hump"), and on the face ("moon face").<ref name="Hopkins_2005" /> Patient education and provider monitoring is the first step in recognizing and diagnosing Iatrogenic Cushing's Syndrome. Exogenous glucocorticoids suppress [[adrenocorticotropic hormone]] (ATCH) production, which can be verified by AM biochemical analysis.<ref name="Hopkins_2005" /> The onset of side effects varies; neuropsychiatric symptoms can arise within a few hours, while osteoporosis takes months to develop.<ref name="Hopkins_2005" /> | |||
The metabolic effects of taking methylprednisolone involve the continuous breakdown of proteins for gluconeogenesis increasing the necessity for insulin. This results in hyperlipidemia, weight gain, and myopathy that may prompt a patient to cease treatment.<ref name="Katzung_2012"/> | |||
=== Infections === | |||
{{see|Glucocorticoid#Immunodeficiency}} | |||
The Immunodeficiency section tabulates known pathogens of concern in glucocorticoid-induced immunodeficiency. | |||
=== Musculoskeletal === | |||
Osteoporosis is a type of bone disease characterized by a loss of bone density, mass, and architecture that leaves a patient susceptible to fractures.<ref>{{cite web|title=Osteoporosis Overview {{!}} NIH Osteoporosis and Related Bone Diseases National Resource Center|url=https://www.bones.nih.gov/health-info/bone/osteoporosis/overview|access-date=7 December 2020|website=www.bones.nih.gov}}</ref> The World Health Organization (WHO) defines osteoporosis in caucasian postmenopausal women as a bone mineral density (BMD) and a T-score of -2.5 or less.<ref name="Phang_2018"/><ref>{{cite journal | vauthors = Jeremiah MP, Unwin BK, Greenawald MH, Casiano VE | title = Diagnosis and Management of Osteoporosis | journal = American Family Physician | volume = 92 | issue = 4 | pages = 261–8 | date = August 2015 | pmid = 26280231 | url = https://www.aafp.org/afp/2015/0815/p261.html }}</ref> The prevalence of osteoporosis in patients with SLE varies geographically and some attribute it to BMD and T-score diagnostic appropriateness.<ref name="Phang_2018"/> British 10.3%, Chinese 21.7%The Canadian Clinical Practice Guidelines and The American College of Rheumatology have switched to using a Z-score as a diagnostic marker for osteoporosis but have failed to find a clinical diagnostic threshold.<ref name="Phang_2018"/> Additionally, a UK-based study showed that BMD may underrepresent a patient with SLE, as their risk for fractures is 22% higher than the healthy individual.<ref name="Phang_2018"/> | |||
Exogenous corticosteroids induce osteoporosis by increasing bone resorption and reducing bone formation.<ref name="Phang_2018"/> Bone loss can be pronounced within the first few months of initiating methylprednisolone with a steady decrease with chronic use. Trabecular bone loss in the lumbar spine precedes cortical bone loss in the femoral neck.<ref name="Phang_2018"/> | |||
=== Exhaustive list === | |||
Allergic: allergic or hypersensitivity reactions, anaphylactoid reaction, anaphylaxis, and urticaria.<ref name="Pfizer and Upjohn Company LLC_2019"/> | |||
Cardiovascular: hypertension, congestive heart failure in susceptible patients,<ref name="Pfizer and Upjohn Company LLC_2019"/> premature atherosclerotic disease, arrhythmias, and possible hyperlipidemia.<ref name="Hopkins_2005" /> | |||
Dermatologic: impaired wound healing, petechiae, and ecchymoses, thinning of the skin, facial erythema, and increased sweating.<ref name="Pfizer and Upjohn Company LLC_2019"/> | |||
Endocrine: Cushingoid features, growth suppression in children, secondary adrenocortical and pituitary unresponsiveness, menstrual irregularities, decreased carbohydrate intolerance, and latent diabetes mellitus. In patients with diabetes, increased requirements of insulin or oral hypoglycemic agents.<ref name="Pfizer and Upjohn Company LLC_2019"/> | |||
Fluid and electrolyte disturbances: sodium retention, fluid retention, potassium loss, hypokalemic alkalosis, or congestive heart failure in susceptible patients.<ref name="Pfizer and Upjohn Company LLC_2019"/> | |||
Gastrointestinal: peptic ulcer, pancreatitis, abdominal distention, and ulcerative esophagitis.<ref name="Pfizer and Upjohn Company LLC_2019"/> | |||
Metabolic: protein catabolism which causes negative nitrogen balance.<ref name="Pfizer and Upjohn Company LLC_2019"/> | |||
Musculoskeletal: muscle weakness, loss of muscle mass, steroid myopathy, osteoporosis, tendon rupture (especially Achilles), vertebral compression fractures, aseptic necrosis of femoral and humeral heads, and pathologic fracture of long bones.<ref name="Pfizer and Upjohn Company LLC_2019"/> | |||
Neurological: increased intracranial pressure with papilledema, convulsions, vertigo, and headache.<ref name="Pfizer and Upjohn Company LLC_2019"/> | |||
Ophthalmic: posterior subcapsular cataracts, increased intraocular pressure, glaucoma, and exophthalmos.<ref name="Pfizer and Upjohn Company LLC_2019"/> | |||
=== Withdrawal === | |||
Feedback of the exogenous glucocorticoids at the hypothalamic–pituitary–adrenal (HPA) axis inhibits the secretion of the [[corticotropin-releasing hormone]] (CRH) and the [[adrenocorticotropic hormone]] (ATCH) at the hypothalamus and pituitary glands, respectively.<ref name="Iliopoulou_2013">{{cite journal | vauthors = Iliopoulou A, Abbas A, Murray R | title = How to manage withdrawal of glucocorticoid therapy. | journal = Prescriber | date = May 2013 | volume = 24 | issue = 10 | pages = 23–9 | doi = 10.1002/psb.1060 | s2cid = 72082017 }}</ref> Prolonged suppression leads to inadequate responses to physical and emotional stresses, such as illness and trauma.<ref name="Iliopoulou_2013" /> Suppression of ATCH may result in adrenal hypoplasia or secondary adrenal gland atrophy within 6 weeks of methylprednisolone therapy, leaving a patient at risk for developing a life-threatening adrenal insufficiency crisis.<ref name="Paragliola_2017"/><ref name="Iliopoulou_2013" /> Factors that contribute to the extent of HPA axis suppression include steroid hormone potency (type of compound and route of administration), cumulative dose, duration of treatment and concomitant drug use.<ref name="Paragliola_2017" /> Any individual who has taken steroid hormones for 2+ weeks is at risk for developing HPA axis suppression.<ref name="Iliopoulou_2013" /> Systemic methylprednisolone risk has been marked as moderate within the class of synthetic glucocorticoids.<ref name="Iliopoulou_2013" /> | |||
Consult with your physician before discontinuing methylprednisolone for any reason.<ref name="MedlinePlus Drug Information_2017">{{cite web | publisher = US National Library of Medicine | date = September 2017 | title = Methylprednisolone | work = MedlinePlus Drug Information | url = https://medlineplus.gov/druginfo/meds/a682795.html }}</ref> Abrupt termination of the drug commonly causes transient non-specific symptoms such as loss of appetite, upset stomach, vomiting, drowsiness, confusion, headache, fever, joint and muscle pain, peeling skin, and weight loss.<ref name="Iliopoulou_2013" /><ref name="MedlinePlus Drug Information_2017" /> These symptoms can be attributed to steroid withdrawal syndrome, adrenal insufficiency, or disease relapse.<ref name="Iliopoulou_2013" /> Those who have been taking methylprednisolone as a long-term treatment may be gradually tapered off to minimize withdrawal symptoms and the potential for relapse.<ref name="MedlinePlus Drug Information_2017" /><ref name="Iliopoulou_2013" /> If symptoms are exacerbated, temporarily increasing methylprednisolone dosage has shown clinical relevancy.<ref name="Iliopoulou_2013" /> Studies retesting patients upon methylprednisolone withdrawal showed persistent adrenal insufficiency, with one study showing 15% after 3 years.<ref name="Paragliola_2017" /><ref name="Joseph_2016">{{cite journal | vauthors = Joseph RM, Hunter AL, Ray DW, Dixon WG | title = Systemic glucocorticoid therapy and adrenal insufficiency in adults: A systematic review | journal = Seminars in Arthritis and Rheumatism | volume = 46 | issue = 1 | pages = 133–41 | date = August 2016 | pmid = 27105755 | pmc = 4987145 | doi = 10.1016/j.semarthrit.2016.03.001 }}</ref> However, there was a wide range of prevalence and lack of uniformity in the follow-up timeline.<ref name="Joseph_2016" /> | |||
== Drug interactions == | |||
Caution is advised when taking methylprednisolone concurrently with the medications described below. | |||
===Enzyme inducers=== | |||
All drugs that fall within the class of enzyme inducers increase the clearance and decrease the half-life of methylprednisolone when co-administered.<ref name="Czock_2005" /> [[Phenobarbital]], [[phenytoin]], [[Rifampicin|rifampin]], carbamazepine and barbiturates, increase hepatic enzymes and rate of elimination, thus reducing the immunosuppressive effect of methylprednisolone.<ref name="Czock_2005" /> Increased dosages may be required to achieve desired effect of methylprednisolone.<ref name="Czock_2005" /> | |||
===Cytochrome P450 (CYP) 3A4 inhibitors=== | |||
[[Troleandomycin]], [[ketoconazole]], and Clarithromycin inhibit metabolism; and may decrease the rate of elimination and increase the half-life of methylprednisolone.<ref name="Pfizer and Upjohn Company LLC_2019"/><ref name="Czock_2005" /> Dosages should be decreased accordingly to avoid side effects. Another CYP 3A4 inhibitor, grapefruit juice, prolongs the half-life of oral methylprednisolone.<ref name="Czock_2005" /> | |||
===Oral contraceptives=== | |||
Oral contraceptives inhibit oxidative processes, as highlighted by their ability to decrease methylprednisolone clearance.<ref name="Czock_2005" /> | |||
===P-glycoprotein inhibitors=== | |||
Methylprednisolone is shown to be a substrate of P-glycoprotein; its inhibition is thought to increase methylprednisone absorption and distribution. No clinical relevance has been linked.<ref name="Czock_2005" /> | |||
===Ciclosporin, tacrolimus, sirolimus (Rapamycin)=== | |||
Methylprednisolone and [[Cyclosporins|cyclosporin]] inhibit metabolism and therefore increase the likelihood of experiencing side effects associated with either of the individual drugs. In addition to known individual side effects, convulsions have been reported.<ref name="Pfizer and Upjohn Company LLC_2019" /> | |||
===Cox1 inhibitors=== | |||
Methylprednisolone may increase the rate of elimination with chronic high doses of [[aspirin]]. Patients are susceptible to increased salicylate serum levels or salicylate toxicity upon termination of methylprednisolone. Excessive caution should be taken when prescribing methylprednisolone and aspirin to patients with [[hypoprothrombinemia]].<ref name="Pfizer and Upjohn Company LLC_2019" /> | |||
===Anticoagulants=== | |||
[[Anticoagulant]]s exhibit variable interactions; monitoring coagulation indices is recommended to achieve the desired effect.<ref name="Pfizer and Upjohn Company LLC_2019" />[[File:Sandoz.Methylprednisolone.4mg.jpg|thumb|Some 4-mg methylprednisolone tablets by [[Sandoz]]]] | |||
== Pharmacology == | |||
Methylprednisolone is a synthetic glucocorticoid (GCs) that exhibits pleiotropic effects on a variety of physiological mechanisms.<ref name="Timmermans_2019"/> However, they have been prescribed extensively for their effects on inflammation and immunity.<ref name="Xavier_2016"/> The effects of synthetic glucocorticoids, such as methylprednisolone, are dependent on its association with intracellular glucocorticoid receptors (GRs), and to a lesser extent, mineralocorticoid receptors (MRs). GRs are widely distributed in contrast to MRs that show a restricted tissue distribution.<ref name="Paragliola_2017"/> By this mechanism, the ligand-bound receptor translocates to the nucleus and modulates gene expression.<ref name="Xavier_2016"/> | |||
[[File:Signal Transduction Image.jpg|thumb|center|334x334px|The signal transduction pathway of glucocorticoids (methylprednisolone): Genomic and non-genomic effects.]] | |||
=== Signal transduction === | |||
In the absence of endogenous or synthetic GCs, monomeric GRs are located in the cytoplasm and form multiprotein complexes with [[heat shock protein]]s (HSPs), [[immunophilins]], and other chaperones such as src, and p23.<ref name="Katzung_2012"/> The GR acts in a ligand-dependent manner, with the complex holding the GR in an inactive form with high specificity for the ligand.<ref name="Xavier_2016"/> When methylprednisolone from the plasma or interstitial fluid diffuses passively across the cell membrane, it binds to the GR inducing a conformational change and GC-GR dimerization. It was previously thought that this conformational change was necessary to dissociate the multiprotein complex to allow the ligand-bound receptor to translocate to the nucleus.<ref name="Katzung_2012"/><ref name="Timmermans_2019"/> However, recent studies have indicated that chaperones play a role in nuclear import.<ref name="Cain_2017">{{cite journal | vauthors = Cain DW, Cidlowski JA | title = Immune regulation by glucocorticoids | journal = Nature Reviews. Immunology | volume = 17 | issue = 4 | pages = 233–247 | date = April 2017 | pmid = 28192415 | doi = 10.1038/nri.2017.1 | pmc = 9761406 | s2cid = 47176122 }}</ref> The now active methylprednisolone-GR complex can either transduce non-genomic changes in the cytoplasm or translocate to the nucleus and regulate the transcriptional activity of target genes by direct, tethering or composite mechanisms.<ref name="Timmermans_2019"/> | |||
=== Genomic signaling === | |||
Genomic mechanisms, regardless of which type, elicit responses with a slow onset and a slow dissipation.<ref name="Czock_2005" /> This is attributed to the duration of mRNA transcription and translation.<ref name="Czock_2005" /> Glucocorticoids can regulate roughly 100 to 1000 genes with specificity to cell type.<ref name="Czock_2005" /> | |||
Three major mechanisms have described how the MP-GR complex alters gene expression by either binding to DNA or transcription modulators.<ref name="Timmermans_2019"/> One mechanism of genomic signaling occurs when the MP-GR complex directly binds to DNA sequences called [[glucocorticoid response elements]] (GREs).<ref name="Timmermans_2019"/> GREs are located in regulatory regions of target genes and mediate their transactivation or transrepression.<ref name="Xavier_2016"/> For example, the activation of [[Annexin A1|lipocortin 1]] (ANAX1) negatively interferes with the production of [[prostaglandin]]s and [[leukotriene]]s, known pro-inflammatory signals. Likewise, negative GREs (nGREs) are responsible for repressing genes involved in immune cell activation.<ref name="Timmermans_2019"/> | |||
=== Post-transcriptional modifications === | |||
Post-translational modifications (PTMs) also contribute to methylprednisolone signaling and can produce genomic and non-genomic effects.<ref name="Cain_2017"/> The GR contains several sites for phosphorylation, sumoylation, ubiquitination, and acetylation that primarily occurs after intracellular methylprednisolone binding to the GR.<ref name="Xavier_2016"/><ref name="Kino_2011">{{cite journal | vauthors = Kino T, Chrousos GP | title = Acetylation-mediated epigenetic regulation of glucocorticoid receptor activity: circadian rhythm-associated alterations of glucocorticoid actions in target tissues | journal = Molecular and Cellular Endocrinology | volume = 336 | issue = 1–2 | pages = 23–30 | date = April 2011 | pmid = 21146585 | pmc = 3057275 | doi = 10.1016/j.mce.2010.12.001 }}</ref> PTMs modulate many functions including nuclear translocation, strength and duration of receptor signaling and cofactor interaction.<ref name="Cain_2017"/> A specific example is the deacetylation by histone deacetylase 2 (HDACe) was necessary for transrepression of NF-κB.<ref name="Xavier_2016"/><ref name="Kino_2011" /> | |||
=== Non-genomic signaling === | |||
The mechanisms of non-genomic signaling are distinct from genomic signaling, yet mediate similar pathways and provide therapeutic relevance.<ref name="Song_2006">{{cite journal | vauthors = Song IH, Buttgereit F | title = Non-genomic glucocorticoid effects to provide the basis for new drug developments | journal = Molecular and Cellular Endocrinology | volume = 246 | issue = 1–2 | pages = 142–6 | date = February 2006 | pmid = 16388891 | doi = 10.1016/j.mce.2005.11.012 | s2cid = 40239838 }}</ref><ref>{{cite journal | vauthors = Panettieri RA, Schaafsma D, Amrani Y, Koziol-White C, Ostrom R, Tliba O | title = Non-genomic Effects of Glucocorticoids: An Updated View | journal = Trends in Pharmacological Sciences | volume = 40 | issue = 1 | pages = 38–49 | date = January 2019 | pmid = 30497693 | pmc = 7106476 | doi = 10.1016/j.tips.2018.11.002 }}</ref> These mechanisms are characterized as having a rapid onset (less than 15 minutes) because they do not rely on time-consuming transcription or translation and are not modified by inhibitors of transcription.<ref name="Czock_2005">{{cite journal | vauthors = Czock D, Keller F, Rasche FM, Häussler U | title = Pharmacokinetics and pharmacodynamics of systemically administered glucocorticoids | journal = Clinical Pharmacokinetics | volume = 44 | issue = 1 | pages = 61–98 | date = 2005 | pmid = 15634032 | doi = 10.2165/00003088-200544010-00003 | s2cid = 24458998 }}</ref> | |||
Methylprednisolone-induced non-genomic signaling is classified by three mechanisms: (1) cytoplasmic glucocorticoid receptor (cGR)-mediated non-genomic effects, (2) membrane-bound glucocorticoid receptor (mGR) non-genomic effects, and (3) physiochemical interactions with cellular membranes (non-specific non-genomic effects).<ref name="Czock_2005" /><ref name="Song_2006" /> | |||
Proteins that dissociate from the activated GC-cGR complex, initiate intracellular transcription-independent mechanisms.<ref name="Stahn_2008">{{cite journal | vauthors = Stahn C, Buttgereit F | title = Genomic and nongenomic effects of glucocorticoids | journal = Nature Clinical Practice. Rheumatology | volume = 4 | issue = 10 | pages = 525–33 | date = October 2008 | pmid = 18762788 | doi = 10.1038/ncprheum0898 | s2cid = 22686260 }}</ref><ref name="Phang_2018">{{cite journal| vauthors = Phang KF, Cho J, Lee W, Mak A |date=2018 |title=Glucocorticoid-induced osteoporosis in systemic lupus erythematosus |journal=Rheumatology Practice and Research|language=en|volume=3 |pages=205990211880251 |doi=10.1177/2059902118802510 |doi-access=free }}</ref> It is evidence that dissociated SRC is responsible for inhibiting the release of arachidonic acid (AA) from cell membrane phospholipids.<ref name="Song_2006" /> AA is required for the synthesis of inflammatory mediators (prostaglandins and leukotrienes) and thus AA inhibition mediates several important pathways such as cellular growth, metabolism and inflammation.<ref name="Stahn_2008" /><ref name="Phang_2018" /> | |||
Previous studies identified mGRs in lymphoma cells, but it wasn't until 2004 that mGRs were identified in human peripheral mononuclear cells.<ref name="Song_2006" /> The prevalence of mGRs ranges per cell type, with the highest concentration in B lymphocytes at up to 12.3%, up to 9.2% in monocytes, and absent from T lymphocytes.<ref name="Song_2006" /> Studies have shown a positive correlation between the mGR-positive cells and disease-related activity.<ref name="Song_2006" /> There are no proven signaling pathways associated with mGR at this time. Some researchers hypothesize that high disease activity activates mGR expression and upon administering methylprednisolone, creates a negative feedback loop by inducing apoptosis.<ref name="Song_2006" /> | |||
High concentrations of methylprednisolone intercalate in plasma and mitochondrial cellular membranes. This association changes the physiochemical properties of the membrane; activating membrane proteins, altering cellular functions and ultimately influencing cation transport through the plasma membrane and stimulating the proton leak across the inner mitochondrial membrane.<ref name="Czock_2005" /><ref name="Song_2006" /> Hindered oxidative phosphorylation compromises ATP production, a major energy source for cellular energy metabolism and immune function. In vivo, studies of Con-A stimulated thymocytes (in rats) and human immune cells that were administered high doses of methylprednisolone have been shown to inhibit respiration in a dose-dependent manner, inhibit plasma calcium and sodium uptake, and increase cytoplasmic calcium concentration.<ref name="Song_2006" /> The summative process is as follows: Methylprednisolone intercalates in the plasma membrane, causes physiochemical changes, and activates membrane proteins that inhibit plasma calcium and sodium uptake (mimicking an energy deficit state). ATP consumption drops (resembled by inhibited respiration), resulting in protein permeability at the inner mitochondrial membrane and uncoupling of oxidative phosphorylation. Of notable importance, DNA/RNA synthesis was not hindered.<ref name="Song_2006" /> The dependency of housekeeping cells and immune cells on ATP, results in immunosuppression during ATP deficit. Specific immune functions affected by this process are cytokinesis, migration, phagocytosis, antigen processing and presenting, antibody synthesis, cytotoxicity, and regulation.<ref name="Song_2006" /> | |||
=== The HPA === | |||
[[File:Methylprednisolone inhibits the HPA axis.png|center|thumb|445x445px|Regulation of the HPA axis]] | |||
The activation of the hypothalamic-pituitary axis (HPA) stimulates the production of endogenous glucocorticoids within the adrenal cortex.<ref name="Cain_2017"/> The HPA interprets stimuli (stress, inflammation, and circadian cues) and transduces a corresponding physiochemical response.<ref name="Xavier_2016"/> Glucocorticoids released in the blood, serve as a messenger by binding to glucocorticoid receptors in a wide distribution across the body, including the HPA itself.<ref name="Cain_2017" /> Thus, the physiological range of GCs is monitored by the negative feedback loop GCs exert on any portion of the HPA.<ref name="Xavier_2016"/> | |||
=== Pharmacokinetics === | |||
{{see also|Glucocorticoid#Pharmacology}} | |||
[[File:Methylprednisolone, methylprednisolone acetate, and melthyprednisolone succinate.svg|class=skin-invert-image|center|thumb|623x623px|Methylprednisolone (Medrol), methylprednisolone acetate (Depo-Medrol), and methylprednisolone succinate (Solu-Medrol), respectively.]] | |||
Methylprednisolone is approved for oral and parenteral administration. Methylprednisolone (Medrol) for oral administration is available in a tablet formulation in 2 mg, 4 mg, 8 mg, 16 mg or 32 mg strengths.<ref name="Pfizer and Upjohn Company LLC_2019">{{cite web | date=1 February 2019|title=Medrol U.S. Physician Prescribing Information|url=http://labeling.pfizer.com/ShowLabeling.aspx?id=601|archive-url=|archive-date=|access-date=10 November 2020|website=Pfizer and Upjohn Company LLC}}</ref> Both methylprednisolone acetate (Depo-Medrol) and methylprednisolone succinate (Solu-Medrol) are approved for intramuscular injection.<ref name="DEPO-MEDROL_label">{{cite web | publisher = Pfizer | date = July 2018 | title = DEPO-MEDROL Multidose vial U.S. Physician Prescribing Information | url = http://labeling.pfizer.com/ShowLabeling.aspx?id=551 }}</ref><ref name="Pfizer_2020">{{cite web | publisher = Pfizer | date = September 2020 | title = SOLU-MEDROL Multidose vial U.S. Physician Prescribing Information | url = http://labeling.pfizer.com/ShowLabeling.aspx?id=648 }}</ref> Depo-Medrol is additionally approved for intralesional, intra-articular, and soft tissue injections. Depo-Medrol is available as sterile aqueous solution in 20 mg/mL, 40 mg/mL, or 80 mg/mL strengths.<ref name="DEPO-MEDROL_label" /> Solu-Medrol is the only derivative of methylprednisolone that is approved for intravenous infusion, as the sterile powder is soluble in water and can be mixed with a diluent. Strengths vary from 40 mg to 2 g.<ref name="Pfizer_2020"/> | |||
Synthetic glucocorticoids are similar to endogenous steroids in metabolism but differ in affinity for glucocorticoid and mineralocorticoid receptors, affinity for protein-binding, rate of elimination, and metabolic products.<ref name="Katzung_2012"/> | |||
Oral methylprednisolone is readily absorbed from the gastrointestinal tract with a bioavailability of 89.9%.<ref name="Garg_1979">{{cite journal | vauthors = Garg DC, Wagner JG, Sakmar E, Weidler DJ, Albert KS | title = Rectal and oral absorption of methylprednisolone acetate | journal = Clinical Pharmacology and Therapeutics | volume = 26 | issue = 2 | pages = 232–9 | date = August 1979 | pmid = 455892 | doi = 10.1002/cpt1979262232 | hdl = 2027.42/117227 | s2cid = 28001411 | hdl-access = free }}</ref> In contrast to endogenous GCs, methylprednisolone does not bind to the glycoprotein transcortin (corticosteroid-binding globulin, CBG) but does have moderate protein binding to albumin.<ref name="Czock_2005" /> Thus, the pharmacokinetics of methylprednisolone are linear and show no dose dependency.<ref name="Czock_2005" /> Patients exhibiting low albumin concentrations are at risk for adverse effects during glucocorticoid therapy.<ref name="Czock_2005" /> Oral methylprednisolone has a moderate distribution into tissue at 1.38L/kg.<ref name="Szefler_1986">{{cite journal | vauthors = Szefler SJ, Ebling WF, Georgitis JW, Jusko WJ | title = Methylprednisolone versus prednisolone pharmacokinetics in relation to dose in adults | journal = European Journal of Clinical Pharmacology | volume = 30 | issue = 3 | pages = 323–9 | date = 1986 | pmid = 3732369 | doi = 10.1007/BF00541537 | s2cid = 21550959 }}</ref> | |||
Methylprednisolone is primarily eliminated by hepatic metabolism and renal excretion of metabolites; with renal excretion of unchanged methylprednisolone at only 1.3–9.2%.<ref name="Szefler_1986" /> Methylprednisolone can be interconverted with methylprednisone.<ref name="Czock_2005" /> Hepatic metabolism is mediated by 11 beta-hydroxysteroid dehydrogenases (11[beta]-HSD) and 20-ketosteroid reductases.<ref name="Szefler_1986" /> Methylprednisolone undergoes renal excretion of hydrophilic inactive metabolites, including 20-carboxymelthylprednisolone and 6[beta]-hydroxy-20[alpha]-hydroxymethylprednisolone.<ref name="Czock_2005" /> | |||
== Physical properties == | |||
Oral methylprednisolone (Medrol) and its derivatives are a white, odorless crystalline powder. Its solubility ranges from practically insoluble in water, very slightly soluble in ether, slightly soluble in acetone and chloroform to sparingly soluble in alcohol, dioxane, and methanol.<ref>{{cite web| work = PubChem|title=Methylprednisolone| url=https://pubchem.ncbi.nlm.nih.gov/compound/6741|access-date=16 November 2020|publisher = U.S. National Library of Medicine |language=en}}</ref> Methylprednisolone acetate suspension (Depo-Medrol) is a 6-methyl derivative of prednisolone that melts at 215 degrees Celsius with some decomposition.<ref name="DEPO-MEDROL_label" /> Methylprednisolone sodium succinate (Solu-Medrol) is the sodium succinate ester of methylprednisolone. Contrary to the solubilities above, methylprednisolone sodium succinate is soluble in water and alcohol, slightly soluble in acetone and insoluble in chloroform<ref name="Pfizer_2020"/>[[File:Depo-Medrol (Methylprednisolone Acetate injectable suspension, USP).jpg|thumb|upright|Depo-Medrol (methylprednisolone acetate) injectable suspension]] | |||
== Chemistry == | |||
Methylprednisolone, or 6α-methylprednisolone, also known as 11β,17,21-trihydroxy-6α-methylpregna-1,4-diene-3,20-dione, is a [[synthetic compound|synthetic]] [[pregnane]] [[steroid]] and a [[chemical derivative|derivative]] of [[hydrocortisone]] (11β,17α,21-trihydroxypregn-4-ene-3,20-dione) and [[prednisolone]] (11β,17α,21-trihydroxypregn-1,4-diene-3,20-dione).<ref name="Elks2014">{{cite book|url=https://books.google.com/books?id=0vXTBwAAQBAJ&pg=PA811|title=The Dictionary of Drugs: Chemical Data: Chemical Data, Structures and Bibliographies|vauthors=Elks J|date=14 November 2014|publisher=Springer|isbn=978-1-4757-2085-3|pages=811–}}</ref><ref name="IndexNominum2000">{{cite book|url=https://books.google.com/books?id=5GpcTQD_L2oC&pg=PA675|title=Index Nominum 2000: International Drug Directory|publisher=Taylor & Francis|year=2000|isbn=978-3-88763-075-1|pages=675–}}</ref> A variety of [[methylprednisolone ester]]s with differing characteristics exist and have been marketed for medical use.<ref name="Elks2014" /><ref name="IndexNominum2000" /> They include [[methylprednisolone aceponate]] (Advantan), [[methylprednisolone acetate]] (Depo-Medrol), [[methylprednisolone succinate]] (Solu-Medrol), and [[methylprednisolone suleptanate]] (Medrosol, Promedrol).<ref name="Elks2014" /><ref name="IndexNominum2000" /> | |||
=== Synthesis === | |||
Synthetic steroids are synthesized from cholic acid and sapogenins obtained from cattle and plants, respectively.<ref name="Katzung_2012"/> | |||
[[File:Methylprednisolone synthesis.svg|class=skin-invert-image|center|thumb|399x399px|Synthesis of Methylprednisolone]] | |||
== History == | |||
Methylprednisolone was first synthesized and manufactured by [[Upjohn|The Upjohn Company]] (now Pfizer) and [[Food and Drug Administration]] (FDA) approved in the United States in October 1957.<ref name="U.S. Food and Drug Administration (FDA)"/> The patent has expired, and generics are available. In 2022, it was the 153rd most commonly prescribed medication in the United States, with more than 3{{nbsp}}million prescriptions.<ref name="The Top 300 of 2022" /><ref name="ClinCalc Methylprednisolone" /> | |||
== Research == | |||
Methylprednisolone has been a prescribed therapy amidst the [[COVID-19 pandemic]], but there is no evidence it is either safe or effective for this purpose.<ref>{{cite journal | vauthors = Kosaka M, Yamazaki Y, Maruno T, Sakaguchi K, Sawaki S | title = Corticosteroids as adjunctive therapy in the treatment of coronavirus disease 2019: A report of two cases and literature review | journal = Journal of Infection and Chemotherapy | volume = 27 | issue = 1 | pages = 94–98 | date = January 2021 | pmid = 32988730 | doi = 10.1016/j.jiac.2020.09.007 | pmc = 7480527 }}</ref><ref>{{cite journal | vauthors = Yousefifard M, Mohamed Ali K, Aghaei A, Zali A, Madani Neishaboori A, Zarghi A, Safari S, Hashemi B, Forouzanfar MM, Hosseini M | title = Corticosteroids on the Management of Coronavirus Disease 2019 (COVID-19): A Systemic Review and Meta-Analysis | journal = Iranian Journal of Public Health | volume = 49 | issue = 8 | pages = 1411–1421 | date = August 2020 | pmid = 33083317 | doi = 10.18502/ijph.v49i8.3863 | pmc = 7554375 }}</ref> | |||
== References == | == References == | ||
{{Reflist}} | |||
{{ | {{Glucocorticoids and antiglucocorticoids}} | ||
{{Glucocorticoid receptor modulators}} | |||
{{Xenobiotic-sensing receptor modulators}} | |||
{{Portal bar | Medicine}} | |||
{{Authority control}} | |||
[[Category: | [[Category:Chemical substances for emergency medicine]] | ||
[[Category: | [[Category:CYP3A4 inducers]] | ||
[[Category:Drugs]] | [[Category:Diketones]] | ||
[[Category:Drugs developed by Pfizer]] | |||
[[Category:Glucocorticoids]] | [[Category:Glucocorticoids]] | ||
[[Category:Pregnanes]] | |||
[[Category:Primary alcohols]] | |||
[[Category:Secondary alcohols]] | |||
[[Category:Tertiary alcohols]] | |||
[[Category:Triols]] | |||
[[Category:Wikipedia medicine articles ready to translate]] | |||
[[Category:World Health Organization essential medicines]] | |||
Revision as of 11:17, 13 January 2025
Corticosteroid medication
| Methylprednisolone | |
|---|---|
| |
| INN | |
| Drug class | |
| Routes of administration | By mouth, intramuscular, intra-articular, intravenous |
| Pregnancy category | |
| Bioavailability | |
| Metabolism | Liver primarily, kidney, tissues; CYP3A4 |
| Elimination half-life | 1.8–2.6 hours |
| Excretion | Urine |
| Legal status | |
| CAS Number | 83-43-2 |
| PubChem | 6741 |
| DrugBank | DB00959 |
| ChemSpider | 6485 |
| KEGG | D00407 |
Methylprednisolone (Depo-Medrol, Medrol, Solu-Medrol) is a synthetic glucocorticoid, primarily prescribed for its anti-inflammatory and immunosuppressive effects.<ref name="Katzung_2012">,
Basic & clinical pharmacology. online version, 12th edition, New York:McGraw-Hill Medical, ISBN 978-0-07-176401-8,</ref><ref name="Timmermans_2019">, A General Introduction to Glucocorticoid Biology, Frontiers in Immunology, Vol. 10, pp. 1545, DOI: 10.3389/fimmu.2019.01545, PMID: 31333672, PMC: 6621919,</ref><ref name="Xavier_2016">, Gene Expression Control by Glucocorticoid Receptors during Innate Immune Responses, Frontiers in Endocrinology, Vol. 7, pp. 31, DOI: 10.3389/fendo.2016.00031, PMID: 27148162, PMC: 4835445,</ref> It is either used at low doses for chronic illnesses or used concomitantly at high doses during acute flares. Methylprednisolone and its derivatives can be administered orally or parenterally.<ref>, StatPearls. online version, StatPearls Publishing, Accessed: 10 November 2020.</ref>
Regardless of the route of administration, methylprednisolone integrates systemically as exhibited by its effectiveness to quickly reduce inflammation during acute flares.<ref>,
Systemic effects of intra-articular corticosteroids, Clinical Rheumatology, Vol. 28(Issue: 7), pp. 749–56, DOI: 10.1007/s10067-009-1135-x, PMID: 19252817,</ref> It is associated with many adverse reactions that require tapering off the drug as soon as the disease is under control.<ref name="Paragliola_2017">, Treatment with Synthetic Glucocorticoids and the Hypothalamus-Pituitary-Adrenal Axis, International Journal of Molecular Sciences, Vol. 18(Issue: 10), pp. 2201, DOI: 10.3390/ijms18102201, PMID: 29053578, PMC: 5666882,</ref> Serious side effects include iatrogenic Cushing's syndrome, hypertension, osteoporosis, diabetes, infection, and skin atrophy.<ref name="Paragliola_2017"/>
Chemically, methylprednisolone is a synthetic pregnane steroid hormone derived from hydrocortisone and prednisolone. It belongs to a class of synthetic glucocorticoids and more generally, corticosteroids. It acts as a mineralocorticoid and glucocorticoid receptor agonist. In comparison to other exogenous glucocorticoids, methylprednisolone has a higher affinity to glucocorticoid receptors than to mineralocorticoid receptors.
Glucocorticoid's name was derived after the discovery of their involvement in regulating carbohydrate metabolism.<ref name="Paragliola_2017"/> The cellular functions of glucocorticoids, such as methylprednisolone, are now understood to regulate homeostasis, metabolism, development, cognition, and inflammation.<ref name="Paragliola_2017"/> They play a critical role in adapting and responding to environmental, physical and emotional stress.<ref name="Paragliola_2017"/>
Methylprednisolone was first synthesized and manufactured by The Upjohn Company (now Viatris) and FDA approved in the United States in October 1957.<ref name="U.S. Food and Drug Administration (FDA)">
Drugs@FDA: FDA-Approved Drugs(link). U.S. Food and Drug Administration (FDA).
Accessed 5 December 2020.
</ref> In 2022, it was the 153rd most commonly prescribed medication in the United States, with more than 3 million prescriptions.<ref name="The Top 300 of 2022">
The Top 300 of 2022(link). ClinCalc.
Accessed 30 August 2024.
</ref><ref name="ClinCalc Methylprednisolone">
Methylprednisolone Drug Usage Statistics, United States, 2013 - 2022(link). ClinCalc.
Accessed 30 August 2024.
</ref> It is on the World Health Organization's List of Essential Medicines.<ref name="WHO23rd">,
The selection and use of essential medicines 2023: web annex A: World Health Organization model list of essential medicines: 23rd list (2023), Geneva:World Health Organization, 2023, ID: WHO/MHP/HPS/EML/2023.02,</ref>
Medical uses
The primary use of methylprednisolone is to suppress inflammatory and immune responses. Methylprednisolone achieves this primarily by regulating the number and function of leukocytes, cytokines, and chemokines.<ref name="Katzung_2012"/> Its widespread inflammatory control is conducive in use across multiple disorders regardless of pathology.<ref name="Katzung_2012"/> Methylprednisolone is commonly prescribed as short-term therapy for acute flares, as seen with acute gouty arthritis. It can be prescribed during on-going therapy in lower doses contingent upon monitorization of adverse effects.<ref name="Timmermans_2019"/> Dosage strength and formulation are optimized per medical use.<ref name="Xavier_2016"/>
Asthma
In 2001–2002, 11.4% of patients diagnosed with asthma and seen at an outpatient visit were prescribed oral corticosteroids as a long-term control therapy.<ref>National Center for Health Statistics. Health, United States, 2004 With Chartbook on Trends in the Health of Americans. Hyattsville, Maryland: 2004 https://www.cdc.gov/nchs/data/hus/hus04.pdf</ref> The National Asthma Education and Prevention Program (NAEPP) indicates systemic methylprednisolone in both short and long-term therapies to quickly control and to suppress persistent asthma, respectively.<ref name="NAEPP_2007">National Asthma Education and Prevention Program,
Expert Panel Report 3 (EPR-3): Guidelines for the Diagnosis and Management of Asthma-Summary Report 2007, The Journal of Allergy and Clinical Immunology, Vol. 120(Issue: 5 Suppl), pp. S94–138, DOI: 10.1016/j.jaci.2007.09.043, PMID: 17983880, Full text,</ref> For exacerbations that result in a visit to the Emergency Department (ED), oral methylprednisolone is preferred over intravenous administration, unless there are issues with adherence or vomiting.<ref name="NAEPP_2007" /><ref name="Alangari_2010">, Genomic and non-genomic actions of glucocorticoids in asthma, Annals of Thoracic Medicine, Vol. 5(Issue: 3), pp. 133–9, DOI: 10.4103/1817-1737.65040, PMID: 20835306, PMC: 2930650,</ref> Oral methylprednisolone is less invasive and studies have shown that equivalent efficacy compared to intravenous methylprednisolone.<ref name="NAEPP_2007" /><ref name="Alangari_2010" /> Dosage above 60–80 mg/day or 2 mg/kg/day is not recommended as it has not been shown to alter pulmonary function, rate of admission, or length of stay in the hospital compared to lower doses.<ref name="Alangari_2010" /> Following ED discharge, it is advised to prescribe a five-day course of methylprednisolone to decrease the probability of relapse or withdrawal symptoms.<ref name="NAEPP_2007" /><ref name="Alangari_2010" />
Rheumatic diseases
Methylprednisolone is used to treat several rheumatic diseases, such as Systemic Lupus Erythematosus (SLE) and Rheumatoid Arthritis (RA). Methylprednisolone dosage and administration for these diseases is highly variable due to varied pathophysiology between the diseases and within patients diagnosed with a given disease.<ref name="Kaul_2016">,
Systemic lupus erythematosus., Nat Rev Dis Primers, Vol. 2, DOI: 10.1038/nrdp.2016.39, PMID: 27306639,</ref><ref name="Chan_2015">, Treatment of severe lupus nephritis: the new horizon, Nature Reviews. Nephrology, Vol. 11(Issue: 1), pp. 46–61, DOI: 10.1038/nrneph.2014.215, PMID: 25421826,</ref> In Lupus Nephritis, a common manifestation of SLE, patients are often prescribed methylprednisolone concomitantly with immunosuppressants. Severe manifestations are often treated with Cyclophosphamide or Rituximab and three doses of methylprednisolone IV-pulse treatment (as recommended by ACR guidelines) before switching to oral prednisolone and azathioprine for maintenance.<ref name="Kaul_2016" /><ref name="Chan_2015" />
Intra-articular corticosteroid injections (IACI) are a second-line therapy to relieve joint pain resulting from rheumatoid arthritis.<ref name="Habib">Habib, G.S. Systemic effects of intra-articular corticosteroids. Clin. Rheumatol. 2009, 28, 749–756.</ref> It is most commonly injected into the joints of the knees and shoulders.<ref name="Habib" /> Although the injection is local, studies have shown systemic absorption as evidenced by beneficial effects on distant joints.<ref name="Habib" /> In an attempt to minimize HPA suppression, FDA guidelines have restricted IACIs to three per year, with a minimum of 30 days in between injections.<ref name="pmid25182149">,
Intra-articular glucocorticoid injections and their effect on hypothalamic-pituitary-adrenal (HPA)-axis function, Endocrine, Vol. 48(Issue: 2), pp. 410–6, DOI: 10.1007/s12020-014-0409-5, PMID: 25182149,</ref>
Primary or secondary adrenocortical insufficiency
Methylprednisolone is not typically recommended for primary or secondary adrenocortical insufficiency compared to other corticosteroids which have a higher affinity for mineralocorticoid receptors and salt-retaining properties.<ref name="Katzung_2012"/>
Labeled indications
The labeled indications below are categorized by route of administration and then by medical discipline.
Oral methylprednisolone
- Allergy and immunology: angioneurotic edema,<ref name="NAEPP_2007" /> asthma, urticaria, seasonal or perennial allergic rhinitis, drug hypersensitivity reactions, and serum sickness.<ref name="Pfizer and Upjohn Company LLC_2019"/>
- Dermatology: toxic epidermal necrolysis,<ref name="NAEPP_2007" /> atopic dermatitis, contact dermatitis, pemphigus, erythema multiforme, Steven-Johnson syndrome, bullous dermatitis herpetiformis, severe seborrheic dermatitis, exfoliative dermatitis, mycosis fungoides, and severe psoriasis.<ref name="Pfizer and Upjohn Company LLC_2019"/>
- Endocrinology: congenital adrenal hyperplasia, hypercalcemia associated with cancer, nonsuppurative thyroiditis, and primary or secondary adrenocortical insufficiency.<ref name="Pfizer and Upjohn Company LLC_2019"/>
- Gastroenterology: inflammatory bowel disease and ulcerative colitis.<ref name="Pfizer and Upjohn Company LLC_2019"/>
- Hematology: acquired (autoimmune) hemolytic anemia, idiopathic thrombocytopenic purpura, secondary thrombocytopenia, erythroblastopenia, leukemia, lymphoma and congenital (erythroid) hypoplastic anemia.<ref name="Pfizer and Upjohn Company LLC_2019"/>
- Pulmonary: aspiration pneumonitis, chronic beryllium disease, eosinophilic pneumonia, symptomatic sarcoidosis, and pulmonary tuberculosis in conjunction with antituberculosis chemotherapy.<ref name="Pfizer and Upjohn Company LLC_2019"/>
- Nephrology: nephrotic syndrome, idiopathic type or secondary to lupus nephritis.<ref name="Pfizer and Upjohn Company LLC_2019"/>
- Neurology: multiple sclerosis.<ref name="Pfizer and Upjohn Company LLC_2019"/>
- Ophthalmology: scleritis, retinal vasculitis,<ref name="NAEPP_2007" /> uveitis, choroiditis, iritis, iridocyclitis, keratitis, optic neuritis, allergic conjunctivitis, allergic corneal marginal ulcers, herpes zoster ophthalmicus, sympathetic ophthalmia, and chorioretinitis.<ref name="Pfizer and Upjohn Company LLC_2019"/>
- Rheumatology: rheumatoid arthritis, rheumatic carditis, acute gouty arthritis, ankylosing spondylitis, dermatomyositis and polymyositis, psoriatic arthritis, systemic lupus erythematosus, acute and subacute bursitis, synovitis of osteoarthritis, post-traumatic osteoarthritis, and epicondylitis.<ref name="Pfizer and Upjohn Company LLC_2019"/>
- Miscellaneous: trichinosis with neurologic or myocardial involvement.<ref name="Pfizer and Upjohn Company LLC_2019"/>
Parenteral methylprednisolone
- Intra-articular or soft tissue injections: acute gouty arthritis, acute and subacute bursitis, acute tenosynovitis, epicondylitis, and synovitis of osteoarthritis.<ref name="Chan_2015" />
- Intralesional injections: alopecia areata, discoid lupus erythematosus, keloids, granuloma annulare, lichen planus, lichen simplex chronicus, psoriatic plaques, necrobiosis lipoidica diabeticorum.<ref name="Chan_2015" />
- Intramuscular injections are prescribed to treat many of the same conditions indicated for oral administration. Intramuscular injections are administered as an alternative to oral therapy.<ref name="Chan_2015" />
Off-label indications
Some of the off-label indications of methylprednisolone include acute spinal cord injury, acute respiratory distress syndrome, alcoholic hepatitis, hormonal resuscitation in cadaveric organ recovery, and chronic obstructive pulmonary disease.<ref name="NAEPP_2007" />
Available forms
| Active Ingredient | Brand Name | ROA | Form | Strength1 | Inactive Ingredients |
|---|---|---|---|---|---|
| methylprednisolone | Medrol | Oral | tablet | 2, 4, 8, 16, 32 mg | calcium stearate, cornstarch, lactose, mineral oil, sorbic acid, sucrose, and erythrosine sodium (2 mg only), FD&C yellow No. 6 (8 and 32 mg only) |
| methylprednisolone | Medrol | Oral | tablet | 4 mg; 21 pills (dose-pack) | calcium stearate, cornstarch, lactose, sucrose |
| methylprednisolone acetate | Depo-Medrol | Parenteral:
intra-articular or soft tissue, intralesional or intramuscular |
suspension | 20, 40, 80 mg/ml | Polyethylene glycol 3350, Polysorbate 80, Monobasic sodium phosphate, Dibasic sodium phosphate USP, Benzyl alcohol2 added as a preservative |
| methylprednisolone acetate3 | Depo-Medrol | Parenteral:
intra-articular or soft tissue, intralesional or intramuscular |
suspension | 40 or 80 mg/ml (single dose vial) | Polyethylene glycol 3350
Myristyl-gamma-picolinium chloride |
| methylprednisolone succinate | Solu-Medrol | Parenteral:
intravenous or intramuscular |
solution, reconstituted | 500, 1000, 2000 mg/vial, 2000 mg with diluent (multi-dose vial) | monobasic sodium phosphate anhydrous, dibasic sodium phosphate dried, and lactose hydrous. Bacteriostatic water added as diluent with Benzyl alcohol2 added as a preservative |
| methylprednisolone succinate3 | Solu-Medrol | Parenteral:
intravenous or intramuscular |
solution, reconstituted | 40, 125, 500, 1000 mg/vial (single dose vial) | monobasic sodium phosphate anhydrous, dibasic sodium phosphate dried, and lactose hydrous. |
Footnotes:
1Signifies varying strengths of available forms. Is not indicative of frequency nor daily cumulative dose; varies per patient and condition.
2Benzyl alcohol should not be used on neonates
3Preservative free formulation
Contraindications
Methylprednisolone should not be taken orally by people who have systemic fungal infections, except for Depo-Medrol when administered as an intra-articular injection for localized joint conditions.<ref name="DEPO-MEDROL_label" /> Methylprednisolone is contraindicated in those with known hypersensitivity to methylprednisolone or its components<ref name="Pfizer and Upjohn Company LLC_2019"/> Steroids should be used with caution in patients with ulcerative colitis, heart disease or hypertension, peptic ulcer, renal insufficiency, osteoporosis, myasthenia gravis, glaucoma, and diabetes.<ref name="Katzung_2012"/><ref name="Pfizer and Upjohn Company LLC_2019"/> Psychic manifestations may appear while taking methylprednisolone, ranging from euphoria, insomnia, personality changes to depression. Caution is required for patients with predisposed psychoses, as psychotic tendencies may be exacerbated while taking corticosteroids.<ref name="Pfizer and Upjohn Company LLC_2019"/>
Solu-Medrol 40 mg dosage contains lactose monohydrate produced from cow's milk; It should not be taken by anyone with known hypersensitivity to dairy products or its components.<ref name="Pfizer_2020"/> Severe medical events have been associated with epidural administration of Solu-Medrol and Depo-Medrol, including spinal cord infarction, paraplegia, quadriplegia, cortical blindness and stroke. Intramuscular injections should not be administered to those with idiopathic thrombocytopenic purpura. Formulations of Solu-Medrol and Depo-Medrol containing benzyl alcohol are contraindicated for use in premature infants.<ref name="Pfizer_2020"/> Exposure of neural tissue to excessive amounts of benzyl alcohol has been associated with toxicity and in rare events has resulted in death.<ref name="DEPO-MEDROL_label" />
Adverse effects

Adverse reactions may overshadow the therapeutic effects of methylprednisolone.<ref name="Paragliola_2017"/>
Central nervous system
There is minimal clinical diagnostic criteria to define the psychic adverse effects (PAE) associated with methylprednisolone use in patients with systemic lupus erythematosus (SLE).<ref name="Fietta_2009">,
Central nervous system effects of natural and synthetic glucocorticoids, Psychiatry and Clinical Neurosciences, Vol. 63(Issue: 5), pp. 613–22, DOI: 10.1111/j.1440-1819.2009.02005.x, PMID: 19788629,</ref> The prevalence varies from 1.3 to 62% of adult treated patients.<ref name="Fietta_2009" /> The type and severity of neuropsychiatric symptoms also varies significantly between patients, with 33% of patients reporting mild to moderate PAE and 5-10% reporting severe PAE.<ref name="Fietta_2009" /> Methylprednisolone dose and duration have been implicated in PAE development. 20 mg/day of prednisone (16 mg/day of methylprednisolone) is the threshold dosage for PAE development agreed upon by many studies.<ref name="Fietta_2009" /> Short-term pulse IV therapy at high doses is associated with rapid onset of manic and hypomanic symptoms, whereas long-term therapy gives rise to depressive symptoms (suicide attempts infrequent).<ref name="Fietta_2009" /> PAE are reversible with treatment reduction or discontinuation.<ref name="Fietta_2009" />
Metabolic and endocrine
Iatrogenic Cushing's Syndrome is a direct complication of glucocorticoid therapy, and the most common cause of exogenous Cushing's Syndrome.<ref name="Hopkins_2005">,
Exogenous Cushing's syndrome and glucocorticoid withdrawal, Endocrinology and Metabolism Clinics of North America, Vol. 34(Issue: 2), pp. 371–84, ix, DOI: 10.1016/j.ecl.2005.01.013, PMID: 15850848,</ref> Clinical features of Cushing's Syndrome are inclusive of many adverse effects in glucocorticoid therapy.<ref name="Hopkins_2005" /> Traditional symptoms include weight gain, myopathy, osteoporosis, increased risk of infection, hypertension, and psychological effects. Fat deposition is centralized on the trunk, in between shoulders ("buffalo hump"), and on the face ("moon face").<ref name="Hopkins_2005" /> Patient education and provider monitoring is the first step in recognizing and diagnosing Iatrogenic Cushing's Syndrome. Exogenous glucocorticoids suppress adrenocorticotropic hormone (ATCH) production, which can be verified by AM biochemical analysis.<ref name="Hopkins_2005" /> The onset of side effects varies; neuropsychiatric symptoms can arise within a few hours, while osteoporosis takes months to develop.<ref name="Hopkins_2005" />
The metabolic effects of taking methylprednisolone involve the continuous breakdown of proteins for gluconeogenesis increasing the necessity for insulin. This results in hyperlipidemia, weight gain, and myopathy that may prompt a patient to cease treatment.<ref name="Katzung_2012"/>
Infections
The Immunodeficiency section tabulates known pathogens of concern in glucocorticoid-induced immunodeficiency.
Musculoskeletal
Osteoporosis is a type of bone disease characterized by a loss of bone density, mass, and architecture that leaves a patient susceptible to fractures.<ref>
Osteoporosis Overview | NIH Osteoporosis and Related Bone Diseases National Resource Center(link). www.bones.nih.gov.
Accessed 7 December 2020.
</ref> The World Health Organization (WHO) defines osteoporosis in caucasian postmenopausal women as a bone mineral density (BMD) and a T-score of -2.5 or less.<ref name="Phang_2018"/><ref>,
Diagnosis and Management of Osteoporosis, American Family Physician, Vol. 92(Issue: 4), pp. 261–8, PMID: 26280231, Full text,</ref> The prevalence of osteoporosis in patients with SLE varies geographically and some attribute it to BMD and T-score diagnostic appropriateness.<ref name="Phang_2018"/> British 10.3%, Chinese 21.7%The Canadian Clinical Practice Guidelines and The American College of Rheumatology have switched to using a Z-score as a diagnostic marker for osteoporosis but have failed to find a clinical diagnostic threshold.<ref name="Phang_2018"/> Additionally, a UK-based study showed that BMD may underrepresent a patient with SLE, as their risk for fractures is 22% higher than the healthy individual.<ref name="Phang_2018"/>
Exogenous corticosteroids induce osteoporosis by increasing bone resorption and reducing bone formation.<ref name="Phang_2018"/> Bone loss can be pronounced within the first few months of initiating methylprednisolone with a steady decrease with chronic use. Trabecular bone loss in the lumbar spine precedes cortical bone loss in the femoral neck.<ref name="Phang_2018"/>
Exhaustive list
Allergic: allergic or hypersensitivity reactions, anaphylactoid reaction, anaphylaxis, and urticaria.<ref name="Pfizer and Upjohn Company LLC_2019"/>
Cardiovascular: hypertension, congestive heart failure in susceptible patients,<ref name="Pfizer and Upjohn Company LLC_2019"/> premature atherosclerotic disease, arrhythmias, and possible hyperlipidemia.<ref name="Hopkins_2005" />
Dermatologic: impaired wound healing, petechiae, and ecchymoses, thinning of the skin, facial erythema, and increased sweating.<ref name="Pfizer and Upjohn Company LLC_2019"/>
Endocrine: Cushingoid features, growth suppression in children, secondary adrenocortical and pituitary unresponsiveness, menstrual irregularities, decreased carbohydrate intolerance, and latent diabetes mellitus. In patients with diabetes, increased requirements of insulin or oral hypoglycemic agents.<ref name="Pfizer and Upjohn Company LLC_2019"/>
Fluid and electrolyte disturbances: sodium retention, fluid retention, potassium loss, hypokalemic alkalosis, or congestive heart failure in susceptible patients.<ref name="Pfizer and Upjohn Company LLC_2019"/>
Gastrointestinal: peptic ulcer, pancreatitis, abdominal distention, and ulcerative esophagitis.<ref name="Pfizer and Upjohn Company LLC_2019"/>
Metabolic: protein catabolism which causes negative nitrogen balance.<ref name="Pfizer and Upjohn Company LLC_2019"/>
Musculoskeletal: muscle weakness, loss of muscle mass, steroid myopathy, osteoporosis, tendon rupture (especially Achilles), vertebral compression fractures, aseptic necrosis of femoral and humeral heads, and pathologic fracture of long bones.<ref name="Pfizer and Upjohn Company LLC_2019"/>
Neurological: increased intracranial pressure with papilledema, convulsions, vertigo, and headache.<ref name="Pfizer and Upjohn Company LLC_2019"/>
Ophthalmic: posterior subcapsular cataracts, increased intraocular pressure, glaucoma, and exophthalmos.<ref name="Pfizer and Upjohn Company LLC_2019"/>
Withdrawal
Feedback of the exogenous glucocorticoids at the hypothalamic–pituitary–adrenal (HPA) axis inhibits the secretion of the corticotropin-releasing hormone (CRH) and the adrenocorticotropic hormone (ATCH) at the hypothalamus and pituitary glands, respectively.<ref name="Iliopoulou_2013">,
How to manage withdrawal of glucocorticoid therapy., Prescriber, Vol. 24(Issue: 10), pp. 23–9, DOI: 10.1002/psb.1060,</ref> Prolonged suppression leads to inadequate responses to physical and emotional stresses, such as illness and trauma.<ref name="Iliopoulou_2013" /> Suppression of ATCH may result in adrenal hypoplasia or secondary adrenal gland atrophy within 6 weeks of methylprednisolone therapy, leaving a patient at risk for developing a life-threatening adrenal insufficiency crisis.<ref name="Paragliola_2017"/><ref name="Iliopoulou_2013" /> Factors that contribute to the extent of HPA axis suppression include steroid hormone potency (type of compound and route of administration), cumulative dose, duration of treatment and concomitant drug use.<ref name="Paragliola_2017" /> Any individual who has taken steroid hormones for 2+ weeks is at risk for developing HPA axis suppression.<ref name="Iliopoulou_2013" /> Systemic methylprednisolone risk has been marked as moderate within the class of synthetic glucocorticoids.<ref name="Iliopoulou_2013" />
Consult with your physician before discontinuing methylprednisolone for any reason.<ref name="MedlinePlus Drug Information_2017">
Methylprednisolone(link). {{{website}}}. US National Library of Medicine. September 2017.
</ref> Abrupt termination of the drug commonly causes transient non-specific symptoms such as loss of appetite, upset stomach, vomiting, drowsiness, confusion, headache, fever, joint and muscle pain, peeling skin, and weight loss.<ref name="Iliopoulou_2013" /><ref name="MedlinePlus Drug Information_2017" /> These symptoms can be attributed to steroid withdrawal syndrome, adrenal insufficiency, or disease relapse.<ref name="Iliopoulou_2013" /> Those who have been taking methylprednisolone as a long-term treatment may be gradually tapered off to minimize withdrawal symptoms and the potential for relapse.<ref name="MedlinePlus Drug Information_2017" /><ref name="Iliopoulou_2013" /> If symptoms are exacerbated, temporarily increasing methylprednisolone dosage has shown clinical relevancy.<ref name="Iliopoulou_2013" /> Studies retesting patients upon methylprednisolone withdrawal showed persistent adrenal insufficiency, with one study showing 15% after 3 years.<ref name="Paragliola_2017" /><ref name="Joseph_2016">,
Systemic glucocorticoid therapy and adrenal insufficiency in adults: A systematic review, Seminars in Arthritis and Rheumatism, Vol. 46(Issue: 1), pp. 133–41, DOI: 10.1016/j.semarthrit.2016.03.001, PMID: 27105755, PMC: 4987145,</ref> However, there was a wide range of prevalence and lack of uniformity in the follow-up timeline.<ref name="Joseph_2016" />
Drug interactions
Caution is advised when taking methylprednisolone concurrently with the medications described below.
Enzyme inducers
All drugs that fall within the class of enzyme inducers increase the clearance and decrease the half-life of methylprednisolone when co-administered.<ref name="Czock_2005" /> Phenobarbital, phenytoin, rifampin, carbamazepine and barbiturates, increase hepatic enzymes and rate of elimination, thus reducing the immunosuppressive effect of methylprednisolone.<ref name="Czock_2005" /> Increased dosages may be required to achieve desired effect of methylprednisolone.<ref name="Czock_2005" />
Cytochrome P450 (CYP) 3A4 inhibitors
Troleandomycin, ketoconazole, and Clarithromycin inhibit metabolism; and may decrease the rate of elimination and increase the half-life of methylprednisolone.<ref name="Pfizer and Upjohn Company LLC_2019"/><ref name="Czock_2005" /> Dosages should be decreased accordingly to avoid side effects. Another CYP 3A4 inhibitor, grapefruit juice, prolongs the half-life of oral methylprednisolone.<ref name="Czock_2005" />
Oral contraceptives
Oral contraceptives inhibit oxidative processes, as highlighted by their ability to decrease methylprednisolone clearance.<ref name="Czock_2005" />
P-glycoprotein inhibitors
Methylprednisolone is shown to be a substrate of P-glycoprotein; its inhibition is thought to increase methylprednisone absorption and distribution. No clinical relevance has been linked.<ref name="Czock_2005" />
Ciclosporin, tacrolimus, sirolimus (Rapamycin)
Methylprednisolone and cyclosporin inhibit metabolism and therefore increase the likelihood of experiencing side effects associated with either of the individual drugs. In addition to known individual side effects, convulsions have been reported.<ref name="Pfizer and Upjohn Company LLC_2019" />
Cox1 inhibitors
Methylprednisolone may increase the rate of elimination with chronic high doses of aspirin. Patients are susceptible to increased salicylate serum levels or salicylate toxicity upon termination of methylprednisolone. Excessive caution should be taken when prescribing methylprednisolone and aspirin to patients with hypoprothrombinemia.<ref name="Pfizer and Upjohn Company LLC_2019" />
Anticoagulants
Anticoagulants exhibit variable interactions; monitoring coagulation indices is recommended to achieve the desired effect.<ref name="Pfizer and Upjohn Company LLC_2019" />

Pharmacology
Methylprednisolone is a synthetic glucocorticoid (GCs) that exhibits pleiotropic effects on a variety of physiological mechanisms.<ref name="Timmermans_2019"/> However, they have been prescribed extensively for their effects on inflammation and immunity.<ref name="Xavier_2016"/> The effects of synthetic glucocorticoids, such as methylprednisolone, are dependent on its association with intracellular glucocorticoid receptors (GRs), and to a lesser extent, mineralocorticoid receptors (MRs). GRs are widely distributed in contrast to MRs that show a restricted tissue distribution.<ref name="Paragliola_2017"/> By this mechanism, the ligand-bound receptor translocates to the nucleus and modulates gene expression.<ref name="Xavier_2016"/>

Signal transduction
In the absence of endogenous or synthetic GCs, monomeric GRs are located in the cytoplasm and form multiprotein complexes with heat shock proteins (HSPs), immunophilins, and other chaperones such as src, and p23.<ref name="Katzung_2012"/> The GR acts in a ligand-dependent manner, with the complex holding the GR in an inactive form with high specificity for the ligand.<ref name="Xavier_2016"/> When methylprednisolone from the plasma or interstitial fluid diffuses passively across the cell membrane, it binds to the GR inducing a conformational change and GC-GR dimerization. It was previously thought that this conformational change was necessary to dissociate the multiprotein complex to allow the ligand-bound receptor to translocate to the nucleus.<ref name="Katzung_2012"/><ref name="Timmermans_2019"/> However, recent studies have indicated that chaperones play a role in nuclear import.<ref name="Cain_2017">,
Immune regulation by glucocorticoids, Nature Reviews. Immunology, Vol. 17(Issue: 4), pp. 233–247, DOI: 10.1038/nri.2017.1, PMID: 28192415, PMC: 9761406,</ref> The now active methylprednisolone-GR complex can either transduce non-genomic changes in the cytoplasm or translocate to the nucleus and regulate the transcriptional activity of target genes by direct, tethering or composite mechanisms.<ref name="Timmermans_2019"/>
Genomic signaling
Genomic mechanisms, regardless of which type, elicit responses with a slow onset and a slow dissipation.<ref name="Czock_2005" /> This is attributed to the duration of mRNA transcription and translation.<ref name="Czock_2005" /> Glucocorticoids can regulate roughly 100 to 1000 genes with specificity to cell type.<ref name="Czock_2005" />
Three major mechanisms have described how the MP-GR complex alters gene expression by either binding to DNA or transcription modulators.<ref name="Timmermans_2019"/> One mechanism of genomic signaling occurs when the MP-GR complex directly binds to DNA sequences called glucocorticoid response elements (GREs).<ref name="Timmermans_2019"/> GREs are located in regulatory regions of target genes and mediate their transactivation or transrepression.<ref name="Xavier_2016"/> For example, the activation of lipocortin 1 (ANAX1) negatively interferes with the production of prostaglandins and leukotrienes, known pro-inflammatory signals. Likewise, negative GREs (nGREs) are responsible for repressing genes involved in immune cell activation.<ref name="Timmermans_2019"/>
Post-transcriptional modifications
Post-translational modifications (PTMs) also contribute to methylprednisolone signaling and can produce genomic and non-genomic effects.<ref name="Cain_2017"/> The GR contains several sites for phosphorylation, sumoylation, ubiquitination, and acetylation that primarily occurs after intracellular methylprednisolone binding to the GR.<ref name="Xavier_2016"/><ref name="Kino_2011">,
Acetylation-mediated epigenetic regulation of glucocorticoid receptor activity: circadian rhythm-associated alterations of glucocorticoid actions in target tissues, Molecular and Cellular Endocrinology, Vol. 336(Issue: 1–2), pp. 23–30, DOI: 10.1016/j.mce.2010.12.001, PMID: 21146585, PMC: 3057275,</ref> PTMs modulate many functions including nuclear translocation, strength and duration of receptor signaling and cofactor interaction.<ref name="Cain_2017"/> A specific example is the deacetylation by histone deacetylase 2 (HDACe) was necessary for transrepression of NF-κB.<ref name="Xavier_2016"/><ref name="Kino_2011" />
Non-genomic signaling
The mechanisms of non-genomic signaling are distinct from genomic signaling, yet mediate similar pathways and provide therapeutic relevance.<ref name="Song_2006">,
Non-genomic glucocorticoid effects to provide the basis for new drug developments, Molecular and Cellular Endocrinology, Vol. 246(Issue: 1–2), pp. 142–6, DOI: 10.1016/j.mce.2005.11.012, PMID: 16388891,</ref><ref>, Non-genomic Effects of Glucocorticoids: An Updated View, Trends in Pharmacological Sciences, Vol. 40(Issue: 1), pp. 38–49, DOI: 10.1016/j.tips.2018.11.002, PMID: 30497693, PMC: 7106476,</ref> These mechanisms are characterized as having a rapid onset (less than 15 minutes) because they do not rely on time-consuming transcription or translation and are not modified by inhibitors of transcription.<ref name="Czock_2005">, Pharmacokinetics and pharmacodynamics of systemically administered glucocorticoids, Clinical Pharmacokinetics, Vol. 44(Issue: 1), pp. 61–98, DOI: 10.2165/00003088-200544010-00003, PMID: 15634032,</ref>
Methylprednisolone-induced non-genomic signaling is classified by three mechanisms: (1) cytoplasmic glucocorticoid receptor (cGR)-mediated non-genomic effects, (2) membrane-bound glucocorticoid receptor (mGR) non-genomic effects, and (3) physiochemical interactions with cellular membranes (non-specific non-genomic effects).<ref name="Czock_2005" /><ref name="Song_2006" />
Proteins that dissociate from the activated GC-cGR complex, initiate intracellular transcription-independent mechanisms.<ref name="Stahn_2008">,
Genomic and nongenomic effects of glucocorticoids, Nature Clinical Practice. Rheumatology, Vol. 4(Issue: 10), pp. 525–33, DOI: 10.1038/ncprheum0898, PMID: 18762788,</ref><ref name="Phang_2018">, Glucocorticoid-induced osteoporosis in systemic lupus erythematosus, Rheumatology Practice and Research, Vol. 3, pp. 205990211880251, DOI: 10.1177/2059902118802510,</ref> It is evidence that dissociated SRC is responsible for inhibiting the release of arachidonic acid (AA) from cell membrane phospholipids.<ref name="Song_2006" /> AA is required for the synthesis of inflammatory mediators (prostaglandins and leukotrienes) and thus AA inhibition mediates several important pathways such as cellular growth, metabolism and inflammation.<ref name="Stahn_2008" /><ref name="Phang_2018" />
Previous studies identified mGRs in lymphoma cells, but it wasn't until 2004 that mGRs were identified in human peripheral mononuclear cells.<ref name="Song_2006" /> The prevalence of mGRs ranges per cell type, with the highest concentration in B lymphocytes at up to 12.3%, up to 9.2% in monocytes, and absent from T lymphocytes.<ref name="Song_2006" /> Studies have shown a positive correlation between the mGR-positive cells and disease-related activity.<ref name="Song_2006" /> There are no proven signaling pathways associated with mGR at this time. Some researchers hypothesize that high disease activity activates mGR expression and upon administering methylprednisolone, creates a negative feedback loop by inducing apoptosis.<ref name="Song_2006" />
High concentrations of methylprednisolone intercalate in plasma and mitochondrial cellular membranes. This association changes the physiochemical properties of the membrane; activating membrane proteins, altering cellular functions and ultimately influencing cation transport through the plasma membrane and stimulating the proton leak across the inner mitochondrial membrane.<ref name="Czock_2005" /><ref name="Song_2006" /> Hindered oxidative phosphorylation compromises ATP production, a major energy source for cellular energy metabolism and immune function. In vivo, studies of Con-A stimulated thymocytes (in rats) and human immune cells that were administered high doses of methylprednisolone have been shown to inhibit respiration in a dose-dependent manner, inhibit plasma calcium and sodium uptake, and increase cytoplasmic calcium concentration.<ref name="Song_2006" /> The summative process is as follows: Methylprednisolone intercalates in the plasma membrane, causes physiochemical changes, and activates membrane proteins that inhibit plasma calcium and sodium uptake (mimicking an energy deficit state). ATP consumption drops (resembled by inhibited respiration), resulting in protein permeability at the inner mitochondrial membrane and uncoupling of oxidative phosphorylation. Of notable importance, DNA/RNA synthesis was not hindered.<ref name="Song_2006" /> The dependency of housekeeping cells and immune cells on ATP, results in immunosuppression during ATP deficit. Specific immune functions affected by this process are cytokinesis, migration, phagocytosis, antigen processing and presenting, antibody synthesis, cytotoxicity, and regulation.<ref name="Song_2006" />
The HPA

The activation of the hypothalamic-pituitary axis (HPA) stimulates the production of endogenous glucocorticoids within the adrenal cortex.<ref name="Cain_2017"/> The HPA interprets stimuli (stress, inflammation, and circadian cues) and transduces a corresponding physiochemical response.<ref name="Xavier_2016"/> Glucocorticoids released in the blood, serve as a messenger by binding to glucocorticoid receptors in a wide distribution across the body, including the HPA itself.<ref name="Cain_2017" /> Thus, the physiological range of GCs is monitored by the negative feedback loop GCs exert on any portion of the HPA.<ref name="Xavier_2016"/>
Pharmacokinetics

Methylprednisolone is approved for oral and parenteral administration. Methylprednisolone (Medrol) for oral administration is available in a tablet formulation in 2 mg, 4 mg, 8 mg, 16 mg or 32 mg strengths.<ref name="Pfizer and Upjohn Company LLC_2019">
Medrol U.S. Physician Prescribing Information(link). Pfizer and Upjohn Company LLC.
1 February 2019.
Accessed 10 November 2020.
</ref> Both methylprednisolone acetate (Depo-Medrol) and methylprednisolone succinate (Solu-Medrol) are approved for intramuscular injection.<ref name="DEPO-MEDROL_label">
DEPO-MEDROL Multidose vial U.S. Physician Prescribing Information(link). {{{website}}}. Pfizer. July 2018.
</ref><ref name="Pfizer_2020">
SOLU-MEDROL Multidose vial U.S. Physician Prescribing Information(link). {{{website}}}. Pfizer. September 2020.
</ref> Depo-Medrol is additionally approved for intralesional, intra-articular, and soft tissue injections. Depo-Medrol is available as sterile aqueous solution in 20 mg/mL, 40 mg/mL, or 80 mg/mL strengths.<ref name="DEPO-MEDROL_label" /> Solu-Medrol is the only derivative of methylprednisolone that is approved for intravenous infusion, as the sterile powder is soluble in water and can be mixed with a diluent. Strengths vary from 40 mg to 2 g.<ref name="Pfizer_2020"/>
Synthetic glucocorticoids are similar to endogenous steroids in metabolism but differ in affinity for glucocorticoid and mineralocorticoid receptors, affinity for protein-binding, rate of elimination, and metabolic products.<ref name="Katzung_2012"/>
Oral methylprednisolone is readily absorbed from the gastrointestinal tract with a bioavailability of 89.9%.<ref name="Garg_1979">,
Rectal and oral absorption of methylprednisolone acetate, Clinical Pharmacology and Therapeutics, Vol. 26(Issue: 2), pp. 232–9, DOI: 10.1002/cpt1979262232, PMID: 455892,</ref> In contrast to endogenous GCs, methylprednisolone does not bind to the glycoprotein transcortin (corticosteroid-binding globulin, CBG) but does have moderate protein binding to albumin.<ref name="Czock_2005" /> Thus, the pharmacokinetics of methylprednisolone are linear and show no dose dependency.<ref name="Czock_2005" /> Patients exhibiting low albumin concentrations are at risk for adverse effects during glucocorticoid therapy.<ref name="Czock_2005" /> Oral methylprednisolone has a moderate distribution into tissue at 1.38L/kg.<ref name="Szefler_1986">, Methylprednisolone versus prednisolone pharmacokinetics in relation to dose in adults, European Journal of Clinical Pharmacology, Vol. 30(Issue: 3), pp. 323–9, DOI: 10.1007/BF00541537, PMID: 3732369,</ref>
Methylprednisolone is primarily eliminated by hepatic metabolism and renal excretion of metabolites; with renal excretion of unchanged methylprednisolone at only 1.3–9.2%.<ref name="Szefler_1986" /> Methylprednisolone can be interconverted with methylprednisone.<ref name="Czock_2005" /> Hepatic metabolism is mediated by 11 beta-hydroxysteroid dehydrogenases (11[beta]-HSD) and 20-ketosteroid reductases.<ref name="Szefler_1986" /> Methylprednisolone undergoes renal excretion of hydrophilic inactive metabolites, including 20-carboxymelthylprednisolone and 6[beta]-hydroxy-20[alpha]-hydroxymethylprednisolone.<ref name="Czock_2005" />
Physical properties
Oral methylprednisolone (Medrol) and its derivatives are a white, odorless crystalline powder. Its solubility ranges from practically insoluble in water, very slightly soluble in ether, slightly soluble in acetone and chloroform to sparingly soluble in alcohol, dioxane, and methanol.<ref>
Methylprednisolone(link). {{{website}}}. U.S. National Library of Medicine.
Accessed 16 November 2020.
</ref> Methylprednisolone acetate suspension (Depo-Medrol) is a 6-methyl derivative of prednisolone that melts at 215 degrees Celsius with some decomposition.<ref name="DEPO-MEDROL_label" /> Methylprednisolone sodium succinate (Solu-Medrol) is the sodium succinate ester of methylprednisolone. Contrary to the solubilities above, methylprednisolone sodium succinate is soluble in water and alcohol, slightly soluble in acetone and insoluble in chloroform<ref name="Pfizer_2020"/>

Chemistry
Methylprednisolone, or 6α-methylprednisolone, also known as 11β,17,21-trihydroxy-6α-methylpregna-1,4-diene-3,20-dione, is a synthetic pregnane steroid and a derivative of hydrocortisone (11β,17α,21-trihydroxypregn-4-ene-3,20-dione) and prednisolone (11β,17α,21-trihydroxypregn-1,4-diene-3,20-dione).<ref name="Elks2014">,
The Dictionary of Drugs: Chemical Data: Chemical Data, Structures and Bibliographies. online version, Springer, ISBN 978-1-4757-2085-3, Pages: 811–,</ref><ref name="IndexNominum2000">, Index Nominum 2000: International Drug Directory. online version, Taylor & Francis, 2000, ISBN 978-3-88763-075-1, Pages: 675–,</ref> A variety of methylprednisolone esters with differing characteristics exist and have been marketed for medical use.<ref name="Elks2014" /><ref name="IndexNominum2000" /> They include methylprednisolone aceponate (Advantan), methylprednisolone acetate (Depo-Medrol), methylprednisolone succinate (Solu-Medrol), and methylprednisolone suleptanate (Medrosol, Promedrol).<ref name="Elks2014" /><ref name="IndexNominum2000" />
Synthesis
Synthetic steroids are synthesized from cholic acid and sapogenins obtained from cattle and plants, respectively.<ref name="Katzung_2012"/>

History
Methylprednisolone was first synthesized and manufactured by The Upjohn Company (now Pfizer) and Food and Drug Administration (FDA) approved in the United States in October 1957.<ref name="U.S. Food and Drug Administration (FDA)"/> The patent has expired, and generics are available. In 2022, it was the 153rd most commonly prescribed medication in the United States, with more than 3 million prescriptions.<ref name="The Top 300 of 2022" /><ref name="ClinCalc Methylprednisolone" />
Research
Methylprednisolone has been a prescribed therapy amidst the COVID-19 pandemic, but there is no evidence it is either safe or effective for this purpose.<ref>,
Corticosteroids as adjunctive therapy in the treatment of coronavirus disease 2019: A report of two cases and literature review, Journal of Infection and Chemotherapy, Vol. 27(Issue: 1), pp. 94–98, DOI: 10.1016/j.jiac.2020.09.007, PMID: 32988730, PMC: 7480527,</ref><ref>, Corticosteroids on the Management of Coronavirus Disease 2019 (COVID-19): A Systemic Review and Meta-Analysis, Iranian Journal of Public Health, Vol. 49(Issue: 8), pp. 1411–1421, DOI: 10.18502/ijph.v49i8.3863, PMID: 33083317, PMC: 7554375,</ref>
References
<references group="" responsive="1"></references>
| Glucocorticoids and antiglucocorticoids (D07, H02) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| Xenobiotic-sensing receptor modulators | ||||
|---|---|---|---|---|
;See also
|