Pulmonary arterial hypertension: Difference between revisions
CSV import |
CSV import |
||
| Line 1: | Line 1: | ||
{{SI}} | |||
{{Infobox medical condition | |||
| name = Pulmonary arterial hypertension | |||
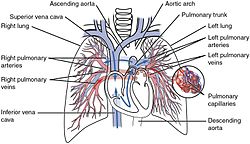
| image = [[File:2119_Pulmonary_Circuit.jpg|250px]] | |||
| caption = Diagram of the pulmonary circuit | |||
| field = [[Cardiology]] | |||
| synonyms = PAH | |||
| symptoms = [[Shortness of breath]], [[fatigue (medical)|fatigue]], [[chest pain]], [[syncope]] | |||
| complications = [[Right-sided heart failure]], [[arrhythmia]], [[blood clots]] | |||
| onset = Any age, but commonly diagnosed in adults | |||
| duration = Long-term | |||
| causes = Idiopathic, [[genetic disorder|genetic]], [[connective tissue disease]], [[congenital heart disease]], [[HIV/AIDS]], [[portal hypertension]], [[drugs]] | |||
| risks = Family history, [[obesity]], [[gender]], [[altitude]] | |||
| diagnosis = [[Echocardiogram]], [[right heart catheterization]], [[chest X-ray]], [[pulmonary function test]] | |||
| differential = [[Chronic thromboembolic pulmonary hypertension]], [[left heart disease]], [[lung disease]] | |||
| treatment = [[Endothelin receptor antagonists]], [[phosphodiesterase-5 inhibitors]], [[prostacyclin analogs]], [[oxygen therapy]], [[lung transplantation]] | |||
| medication = [[Bosentan]], [[sildenafil]], [[epoprostenol]] | |||
| prognosis = Variable, depends on response to treatment | |||
| frequency = Rare | |||
| deaths = Varies, but can be life-threatening | |||
}} | |||
'''Other Names: ''' | '''Other Names: ''' | ||
Primary pulmonary hypertension; PPH; PAH; Idiopathic pulmonary arterial hypertension; Idiopathic pulmonary hypertension; Heritable pulmonary arterial hypertension; Hereditary pulmonary arterial hypertension; Familial pulmonary arterial hypertension; FPAH | Primary pulmonary hypertension; PPH; PAH; Idiopathic pulmonary arterial hypertension; Idiopathic pulmonary hypertension; Heritable pulmonary arterial hypertension; Hereditary pulmonary arterial hypertension; Familial pulmonary arterial hypertension; FPAH | ||
Pulmonary arterial hypertension (PAH) is a progressive condition that affects the heart and lungs. It is characterized by abnormally high blood pressure ([[hypertension]]) in the pulmonary artery, the blood vessel that carries blood from the heart to the lungs. | Pulmonary arterial hypertension (PAH) is a progressive condition that affects the heart and lungs. It is characterized by abnormally high blood pressure ([[hypertension]]) in the pulmonary artery, the blood vessel that carries blood from the heart to the lungs. | ||
Pulmonary arterial hypertension is one form of a broader condition known as [[pulmonary hypertension]]. Pulmonary hypertension occurs when most of the very small arteries throughout the lungs narrow in diameter, which increases the resistance to blood flow through the lungs. To overcome the increased resistance, blood pressure increases in the [[pulmonary artery]] and in the right ventricle of the heart, which is the chamber that pumps blood into the pulmonary artery. Ultimately, the increased blood pressure can damage the right ventricle of the heart. | Pulmonary arterial hypertension is one form of a broader condition known as [[pulmonary hypertension]]. Pulmonary hypertension occurs when most of the very small arteries throughout the lungs narrow in diameter, which increases the resistance to blood flow through the lungs. To overcome the increased resistance, blood pressure increases in the [[pulmonary artery]] and in the right ventricle of the heart, which is the chamber that pumps blood into the pulmonary artery. Ultimately, the increased blood pressure can damage the right ventricle of the heart. | ||
<youtube> | <youtube> | ||
title='''{{PAGENAME}}''' | title='''{{PAGENAME}}''' | ||
| Line 15: | Line 34: | ||
height=600 | height=600 | ||
</youtube> | </youtube> | ||
== '''Cause''' == | == '''Cause''' == | ||
Mutations in the '''BMPR2 gene''' are the most common genetic cause of pulmonary arterial hypertension. This gene plays a role in regulating the number of cells in certain tissues. Researchers suggest that a mutation in this gene promotes cell division or prevents cell death, resulting in an overgrowth of cells in small arteries throughout the lungs. As a result, these arteries narrow in diameter, which increases the resistance to blood flow. Blood pressure in the pulmonary artery and the right ventricle of the heart increases to overcome the increased resistance to blood flow. | Mutations in the '''BMPR2 gene''' are the most common genetic cause of pulmonary arterial hypertension. This gene plays a role in regulating the number of cells in certain tissues. Researchers suggest that a mutation in this gene promotes cell division or prevents cell death, resulting in an overgrowth of cells in small arteries throughout the lungs. As a result, these arteries narrow in diameter, which increases the resistance to blood flow. Blood pressure in the pulmonary artery and the right ventricle of the heart increases to overcome the increased resistance to blood flow. | ||
Mutations in several additional genes have also been found to cause pulmonary arterial hypertension, but they are much less common causes of the disorder than are '''BMPR2 gene''' mutations. Variations in other genes may increase the risk of developing pulmonary arterial hypertension or modify the course of the disease (usually making it more severe). Changes in as-yet-unidentified genes may also be associated with this condition. | Mutations in several additional genes have also been found to cause pulmonary arterial hypertension, but they are much less common causes of the disorder than are '''BMPR2 gene''' mutations. Variations in other genes may increase the risk of developing pulmonary arterial hypertension or modify the course of the disease (usually making it more severe). Changes in as-yet-unidentified genes may also be associated with this condition. | ||
== '''Risk factors''' == | == '''Risk factors''' == | ||
Researchers have also identified nongenetic factors that increase the risk of developing pulmonary arterial hypertension. These include certain drugs used as appetite suppressants and several illegal drugs, such as [[cocaine]] and [[methamphetamine]]. Pulmonary arterial hypertension is also a rare complication of certain infectious diseases, including [[HIV]] and [[schistosomiasis]]. | Researchers have also identified nongenetic factors that increase the risk of developing pulmonary arterial hypertension. These include certain drugs used as appetite suppressants and several illegal drugs, such as [[cocaine]] and [[methamphetamine]]. Pulmonary arterial hypertension is also a rare complication of certain infectious diseases, including [[HIV]] and [[schistosomiasis]]. | ||
== '''Inheritance''' == | == '''Inheritance''' == | ||
Pulmonary arterial hypertension is usually [[sporadic]], which means it occurs in individuals with no known family history of the disorder. These non-familial cases are described as idiopathic pulmonary arterial hypertension. About 20 percent of these cases are caused by mutations in one of the genes known to be associated with the disease, but most of the time a causative gene mutation has not been identified. | Pulmonary arterial hypertension is usually [[sporadic]], which means it occurs in individuals with no known family history of the disorder. These non-familial cases are described as idiopathic pulmonary arterial hypertension. About 20 percent of these cases are caused by mutations in one of the genes known to be associated with the disease, but most of the time a causative gene mutation has not been identified. | ||
Inherited cases of this disorder are known as '''familial pulmonary arterial hypertension'''. When the condition is inherited, it most often has an [[autosomal dominant]] pattern of inheritance, which means one copy of an altered gene in each cell is sufficient to cause the disorder. However, many people with an altered gene never develop pulmonary arterial hypertension; this phenomenon is called reduced penetrance. | Inherited cases of this disorder are known as '''familial pulmonary arterial hypertension'''. When the condition is inherited, it most often has an [[autosomal dominant]] pattern of inheritance, which means one copy of an altered gene in each cell is sufficient to cause the disorder. However, many people with an altered gene never develop pulmonary arterial hypertension; this phenomenon is called reduced penetrance. | ||
== '''Signs and symptoms''' == | == '''Signs and symptoms''' == | ||
Signs and symptoms of pulmonary arterial hypertension occur when increased blood pressure cannot fully overcome the elevated resistance. As a result, the flow of oxygenated blood from the lungs to the rest of the body is insufficient. Shortness of breath (dyspnea) during exertion and fainting spells are the most common symptoms of pulmonary arterial hypertension. People with this disorder may experience additional symptoms, particularly as the condition worsens. Other symptoms include dizziness, swelling (edema) of the ankles or legs, chest pain, and a rapid heart rate. | Signs and symptoms of pulmonary arterial hypertension occur when increased blood pressure cannot fully overcome the elevated resistance. As a result, the flow of oxygenated blood from the lungs to the rest of the body is insufficient. Shortness of breath (dyspnea) during exertion and fainting spells are the most common symptoms of pulmonary arterial hypertension. People with this disorder may experience additional symptoms, particularly as the condition worsens. Other symptoms include dizziness, swelling (edema) of the ankles or legs, chest pain, and a rapid heart rate. | ||
| Line 39: | Line 52: | ||
* Right ventricular failure | * Right ventricular failure | ||
* Right ventricular [[hypertrophy]] | * Right ventricular [[hypertrophy]] | ||
30%-79% of people have these symptoms | 30%-79% of people have these symptoms | ||
* Abnormal thrombosis(Abnormal blood clot) | * Abnormal thrombosis(Abnormal blood clot) | ||
| Line 50: | Line 62: | ||
* Pulmonary aterial intimal [[fibrosis]] | * Pulmonary aterial intimal [[fibrosis]] | ||
* Vertigo(Dizzy spell) | * Vertigo(Dizzy spell) | ||
5%-29% of people have these symptoms | 5%-29% of people have these symptoms | ||
* Abnormal tricuspid valve morphology | * Abnormal tricuspid valve morphology | ||
| Line 60: | Line 71: | ||
* Recurrent respiratory infections(Frequent respiratory infections) | * Recurrent respiratory infections(Frequent respiratory infections) | ||
* Sudden cardiac death(Premature sudden cardiac death) | * Sudden cardiac death(Premature sudden cardiac death) | ||
1%-4% of people have these symptoms | 1%-4% of people have these symptoms | ||
* Pulmonary arterial hypertension(Increased blood pressure in blood vessels of lungs) | * Pulmonary arterial hypertension(Increased blood pressure in blood vessels of lungs) | ||
== '''Diagnosis''' == | == '''Diagnosis''' == | ||
The diagnosis of PAH can be established clinically by confirming the presence of pulmonary arterial hypertension (i.e., mean [[pulmonary artery pressure]] >25 mmHg at rest or >30 mmHg during exercise) and excluding other known causes of pulmonary hypertension (PH). The diagnosis of HPAH is confirmed by the presence of two or more family members with PAH or the identification of a pathogenic variant in a simplex case (i.e., a single occurrence in a family). | The diagnosis of PAH can be established clinically by confirming the presence of pulmonary arterial hypertension (i.e., mean [[pulmonary artery pressure]] >25 mmHg at rest or >30 mmHg during exercise) and excluding other known causes of pulmonary hypertension (PH). The diagnosis of HPAH is confirmed by the presence of two or more family members with PAH or the identification of a pathogenic variant in a simplex case (i.e., a single occurrence in a family). | ||
== '''Treatment''' == | == '''Treatment''' == | ||
People with pulmonary arterial hypertension (PAH) benefit from receiving treatment at specialized centers. The Pulmonary Hypertension Association offers a Find a Doctor tool which may aid you in locating your nearest center. | People with pulmonary arterial hypertension (PAH) benefit from receiving treatment at specialized centers. The Pulmonary Hypertension Association offers a Find a Doctor tool which may aid you in locating your nearest center. | ||
Treatment of serious or life threatening PAH may involve continuous IV [[epoprostenol]]. Other treatment options, include [[treprostinil]], [[iloprost]], [[bosentan]], [[ambrisentan]], [[sildenafil]], and [[tadalafil]]. Many of these treatments can be administered in various forms, such as by shot, IV, or inhalation. A small number of people with PAH respond well to long term oral calcium channel blockers. Blood thinners, diuretics, and supplemental oxygen may be prescribed as needed. | Treatment of serious or life threatening PAH may involve continuous IV [[epoprostenol]]. Other treatment options, include [[treprostinil]], [[iloprost]], [[bosentan]], [[ambrisentan]], [[sildenafil]], and [[tadalafil]]. Many of these treatments can be administered in various forms, such as by shot, IV, or inhalation. A small number of people with PAH respond well to long term oral calcium channel blockers. Blood thinners, diuretics, and supplemental oxygen may be prescribed as needed. | ||
Many drugs can be harmful to people with PAH. The following should be avoided: appetite suppressants, cocaine, amphetamines (and related compounds), low oxygen environments (such as high altitudes), and possibly estrogen compounds (oral contraceptives and hormone replacement therapy). | Many drugs can be harmful to people with PAH. The following should be avoided: appetite suppressants, cocaine, amphetamines (and related compounds), low oxygen environments (such as high altitudes), and possibly estrogen compounds (oral contraceptives and hormone replacement therapy). | ||
The medication(s) listed below have been approved by the Food and Drug Administration (FDA) as orphan products for treatment of this condition. | The medication(s) listed below have been approved by the Food and Drug Administration (FDA) as orphan products for treatment of this condition. | ||
* '''[[Riociguat]]''' (Brand name: Adempas) Treatment of adults with pulmonary arterial hypertension (PAH) WHO Group 1, to improve exercise capacity, WHO functional class and to delay clinical worsening. | * '''[[Riociguat]]''' (Brand name: Adempas) Treatment of adults with pulmonary arterial hypertension (PAH) WHO Group 1, to improve exercise capacity, WHO functional class and to delay clinical worsening. | ||
* '''[[Epoprostenol]]''' (Brand name: | * '''[[Epoprostenol]]''' (Brand name: Flolan®) Long-term intravenous treatment of primary pulmonary hypertension in NYHA Class III and Class IV patients. | ||
* '''[[Ambrisentan]] '''(Brand name: | * '''[[Ambrisentan]] '''(Brand name: Letairis®) Treatment of pulmonary arterial hypertension (WHO group I) in patients with WHO class II or III symptoms to improve exercise capacity and delay clinical worsening | ||
* '''[[macitentan]] '''(Brand name: Opsumit) Treatment of pulmonary arterial hypertension (PAH, WHO Group 1) to delay disease progression. Disease progression included: death, initiation of intravenous (IV) or subcutaneous prostanoids, or clinical worsening of PAH (decreased 6-minute walk distance, worsened PAH symptoms and need for additional PAH treatment). Opsumit also reduced hospitalization for PAH. | * '''[[macitentan]] '''(Brand name: Opsumit) Treatment of pulmonary arterial hypertension (PAH, WHO Group 1) to delay disease progression. Disease progression included: death, initiation of intravenous (IV) or subcutaneous prostanoids, or clinical worsening of PAH (decreased 6-minute walk distance, worsened PAH symptoms and need for additional PAH treatment). Opsumit also reduced hospitalization for PAH. | ||
* '''[[Treprostinil]]''' (Brand name: | * '''[[Treprostinil]]''' (Brand name: Remodulin®) Treatment of pulmonary arterial hypertension. | ||
* '''[[Bosentan]]''' (Brand name: Tracleer) Treatment of pulmonary arterial hypertension. | * '''[[Bosentan]]''' (Brand name: Tracleer) Treatment of pulmonary arterial hypertension. | ||
* '''[[Selexipag]] '''(Brand name: Uptravi)For use of Uptravi (Selexipag) Tablets, 200, 400, 600, 800, 1000, 1200, 1400, and 1600 mcg for treatment of pulmonary arterial hypertension (PAH, WHO Group I) to reduce the risks of disease progression and hospitalization for PAH. | * '''[[Selexipag]] '''(Brand name: Uptravi)For use of Uptravi (Selexipag) Tablets, 200, 400, 600, 800, 1000, 1200, 1400, and 1600 mcg for treatment of pulmonary arterial hypertension (PAH, WHO Group I) to reduce the risks of disease progression and hospitalization for PAH. | ||
* '''[[Iloprost]]''' (Brand name: Ventavis)Treatment of pulmonary arterial hypertension (WHO Group I) in patients with NYHA Class III or IV symptoms. | * '''[[Iloprost]]''' (Brand name: Ventavis)Treatment of pulmonary arterial hypertension (WHO Group I) in patients with NYHA Class III or IV symptoms. | ||
== '''Prognosis''' == | == '''Prognosis''' == | ||
The average survival of a person with pulmonary arterial hypertension (PAH) after diagnosis is estimated to be around 2.8 years, however individual prognosis may be better or worse depending on a variety of factors including age and severity of PAH. Studies have demonstrated survivals ranging from less than 1 year to over 7 years. Current treatments are helpful in controlling/managing symptoms experienced by people with PAH, but unfortunately no treatment has significantly improved survival. | The average survival of a person with pulmonary arterial hypertension (PAH) after diagnosis is estimated to be around 2.8 years, however individual prognosis may be better or worse depending on a variety of factors including age and severity of PAH. Studies have demonstrated survivals ranging from less than 1 year to over 7 years. Current treatments are helpful in controlling/managing symptoms experienced by people with PAH, but unfortunately no treatment has significantly improved survival. | ||
| Line 90: | Line 94: | ||
{{Medicine}} | {{Medicine}} | ||
{{Authority control}} | {{Authority control}} | ||
[[Category:Pulmonary heart disease and diseases of pulmonary circulation]] | [[Category:Pulmonary heart disease and diseases of pulmonary circulation]] | ||
[[Category:Hypertension]] | [[Category:Hypertension]] | ||
| Line 97: | Line 100: | ||
{{rarediseases}} | {{rarediseases}} | ||
{{stub}} | {{stub}} | ||
Latest revision as of 22:07, 6 April 2025

Editor-In-Chief: Prab R Tumpati, MD
Obesity, Sleep & Internal medicine
Founder, WikiMD Wellnesspedia &
W8MD medical weight loss NYC and sleep center NYC
| Pulmonary arterial hypertension | |
|---|---|
| |
| Synonyms | PAH |
| Pronounce | N/A |
| Specialty | N/A |
| Symptoms | Shortness of breath, fatigue, chest pain, syncope |
| Complications | Right-sided heart failure, arrhythmia, blood clots |
| Onset | Any age, but commonly diagnosed in adults |
| Duration | Long-term |
| Types | N/A |
| Causes | Idiopathic, genetic, connective tissue disease, congenital heart disease, HIV/AIDS, portal hypertension, drugs |
| Risks | Family history, obesity, gender, altitude |
| Diagnosis | Echocardiogram, right heart catheterization, chest X-ray, pulmonary function test |
| Differential diagnosis | Chronic thromboembolic pulmonary hypertension, left heart disease, lung disease |
| Prevention | N/A |
| Treatment | Endothelin receptor antagonists, phosphodiesterase-5 inhibitors, prostacyclin analogs, oxygen therapy, lung transplantation |
| Medication | Bosentan, sildenafil, epoprostenol |
| Prognosis | Variable, depends on response to treatment |
| Frequency | Rare |
| Deaths | Varies, but can be life-threatening |
Other Names:
Primary pulmonary hypertension; PPH; PAH; Idiopathic pulmonary arterial hypertension; Idiopathic pulmonary hypertension; Heritable pulmonary arterial hypertension; Hereditary pulmonary arterial hypertension; Familial pulmonary arterial hypertension; FPAH
Pulmonary arterial hypertension (PAH) is a progressive condition that affects the heart and lungs. It is characterized by abnormally high blood pressure (hypertension) in the pulmonary artery, the blood vessel that carries blood from the heart to the lungs.
Pulmonary arterial hypertension is one form of a broader condition known as pulmonary hypertension. Pulmonary hypertension occurs when most of the very small arteries throughout the lungs narrow in diameter, which increases the resistance to blood flow through the lungs. To overcome the increased resistance, blood pressure increases in the pulmonary artery and in the right ventricle of the heart, which is the chamber that pumps blood into the pulmonary artery. Ultimately, the increased blood pressure can damage the right ventricle of the heart.
Cause[edit]
Mutations in the BMPR2 gene are the most common genetic cause of pulmonary arterial hypertension. This gene plays a role in regulating the number of cells in certain tissues. Researchers suggest that a mutation in this gene promotes cell division or prevents cell death, resulting in an overgrowth of cells in small arteries throughout the lungs. As a result, these arteries narrow in diameter, which increases the resistance to blood flow. Blood pressure in the pulmonary artery and the right ventricle of the heart increases to overcome the increased resistance to blood flow. Mutations in several additional genes have also been found to cause pulmonary arterial hypertension, but they are much less common causes of the disorder than are BMPR2 gene mutations. Variations in other genes may increase the risk of developing pulmonary arterial hypertension or modify the course of the disease (usually making it more severe). Changes in as-yet-unidentified genes may also be associated with this condition.
Risk factors[edit]
Researchers have also identified nongenetic factors that increase the risk of developing pulmonary arterial hypertension. These include certain drugs used as appetite suppressants and several illegal drugs, such as cocaine and methamphetamine. Pulmonary arterial hypertension is also a rare complication of certain infectious diseases, including HIV and schistosomiasis.
Inheritance[edit]
Pulmonary arterial hypertension is usually sporadic, which means it occurs in individuals with no known family history of the disorder. These non-familial cases are described as idiopathic pulmonary arterial hypertension. About 20 percent of these cases are caused by mutations in one of the genes known to be associated with the disease, but most of the time a causative gene mutation has not been identified. Inherited cases of this disorder are known as familial pulmonary arterial hypertension. When the condition is inherited, it most often has an autosomal dominant pattern of inheritance, which means one copy of an altered gene in each cell is sufficient to cause the disorder. However, many people with an altered gene never develop pulmonary arterial hypertension; this phenomenon is called reduced penetrance.
Signs and symptoms[edit]
Signs and symptoms of pulmonary arterial hypertension occur when increased blood pressure cannot fully overcome the elevated resistance. As a result, the flow of oxygenated blood from the lungs to the rest of the body is insufficient. Shortness of breath (dyspnea) during exertion and fainting spells are the most common symptoms of pulmonary arterial hypertension. People with this disorder may experience additional symptoms, particularly as the condition worsens. Other symptoms include dizziness, swelling (edema) of the ankles or legs, chest pain, and a rapid heart rate. For most diseases, symptoms will vary from person to person. People with the same disease may not have all the symptoms listed. 80%-99% of people have these symptoms
- Chest pain
- Dyspnea(Trouble breathing)
- Elevated right atrial pressure
- Increased pulmonary vascular resistance
- Right ventricular failure
- Right ventricular hypertrophy
30%-79% of people have these symptoms
- Abnormal thrombosis(Abnormal blood clot)
- Fatigue(Tired)
- Hepatomegaly(Enlarged liver)
- Palpitations(Missed heart beat)
- Pedal edema(Fluid accumulation in lower limbs)
- Pulmonary arterial medial hypertrophy
- Pulmonary artery vasoconstriction
- Pulmonary aterial intimal fibrosis
- Vertigo(Dizzy spell)
5%-29% of people have these symptoms
- Abnormal tricuspid valve morphology
- Acrocyanosis(Persistent blue color of hands, feet, or parts of face)
- Ascites(Accumulation of fluid in the abdomen)
- Capillary hemangioma(Strawberry birthmark)
- Congestive heart failure(Cardiac failure)
- Hemoptysis(Coughing up blood)
- Recurrent respiratory infections(Frequent respiratory infections)
- Sudden cardiac death(Premature sudden cardiac death)
1%-4% of people have these symptoms
- Pulmonary arterial hypertension(Increased blood pressure in blood vessels of lungs)
Diagnosis[edit]
The diagnosis of PAH can be established clinically by confirming the presence of pulmonary arterial hypertension (i.e., mean pulmonary artery pressure >25 mmHg at rest or >30 mmHg during exercise) and excluding other known causes of pulmonary hypertension (PH). The diagnosis of HPAH is confirmed by the presence of two or more family members with PAH or the identification of a pathogenic variant in a simplex case (i.e., a single occurrence in a family).
Treatment[edit]
People with pulmonary arterial hypertension (PAH) benefit from receiving treatment at specialized centers. The Pulmonary Hypertension Association offers a Find a Doctor tool which may aid you in locating your nearest center. Treatment of serious or life threatening PAH may involve continuous IV epoprostenol. Other treatment options, include treprostinil, iloprost, bosentan, ambrisentan, sildenafil, and tadalafil. Many of these treatments can be administered in various forms, such as by shot, IV, or inhalation. A small number of people with PAH respond well to long term oral calcium channel blockers. Blood thinners, diuretics, and supplemental oxygen may be prescribed as needed. Many drugs can be harmful to people with PAH. The following should be avoided: appetite suppressants, cocaine, amphetamines (and related compounds), low oxygen environments (such as high altitudes), and possibly estrogen compounds (oral contraceptives and hormone replacement therapy). The medication(s) listed below have been approved by the Food and Drug Administration (FDA) as orphan products for treatment of this condition.
- Riociguat (Brand name: Adempas) Treatment of adults with pulmonary arterial hypertension (PAH) WHO Group 1, to improve exercise capacity, WHO functional class and to delay clinical worsening.
- Epoprostenol (Brand name: Flolan®) Long-term intravenous treatment of primary pulmonary hypertension in NYHA Class III and Class IV patients.
- Ambrisentan (Brand name: Letairis®) Treatment of pulmonary arterial hypertension (WHO group I) in patients with WHO class II or III symptoms to improve exercise capacity and delay clinical worsening
- macitentan (Brand name: Opsumit) Treatment of pulmonary arterial hypertension (PAH, WHO Group 1) to delay disease progression. Disease progression included: death, initiation of intravenous (IV) or subcutaneous prostanoids, or clinical worsening of PAH (decreased 6-minute walk distance, worsened PAH symptoms and need for additional PAH treatment). Opsumit also reduced hospitalization for PAH.
- Treprostinil (Brand name: Remodulin®) Treatment of pulmonary arterial hypertension.
- Bosentan (Brand name: Tracleer) Treatment of pulmonary arterial hypertension.
- Selexipag (Brand name: Uptravi)For use of Uptravi (Selexipag) Tablets, 200, 400, 600, 800, 1000, 1200, 1400, and 1600 mcg for treatment of pulmonary arterial hypertension (PAH, WHO Group I) to reduce the risks of disease progression and hospitalization for PAH.
- Iloprost (Brand name: Ventavis)Treatment of pulmonary arterial hypertension (WHO Group I) in patients with NYHA Class III or IV symptoms.
Prognosis[edit]
The average survival of a person with pulmonary arterial hypertension (PAH) after diagnosis is estimated to be around 2.8 years, however individual prognosis may be better or worse depending on a variety of factors including age and severity of PAH. Studies have demonstrated survivals ranging from less than 1 year to over 7 years. Current treatments are helpful in controlling/managing symptoms experienced by people with PAH, but unfortunately no treatment has significantly improved survival.
| Cardiovascular disease (vessels) | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| Diseases of the respiratory system | ||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
NIH genetic and rare disease info[edit]
Pulmonary arterial hypertension is a rare disease.
| Rare and genetic diseases | ||||||
|---|---|---|---|---|---|---|
|
Rare diseases - Pulmonary arterial hypertension
|


