Drug eruption: Difference between revisions
CSV import Tags: mobile edit mobile web edit |
No edit summary |
||
| Line 42: | Line 42: | ||
* [[Hypersensitivity]] | * [[Hypersensitivity]] | ||
* [[Dermatology]] | * [[Dermatology]] | ||
== External links == | |||
{{Medical resources | |||
| DiseasesDB = | |||
| ICD10 = {{ICD10|L|27|0|l|20}}, {{ICD10|L|27|1|l|20}} | |||
| ICD9 = {{ICD9|692.3}}, {{ICD9|782.1}} | |||
| ICDO = | |||
| OMIM = | |||
| MedlinePlus = | |||
| eMedicineSubj = derm | |||
| eMedicineTopic = 104 | |||
| MeshID = D003875 | |||
}} | |||
{{Diseases of the skin and appendages by morphology}} | |||
{{Dermatitis and eczema}} | |||
{{Urticaria and erythema}} | |||
{{Skin and subcutaneous tissue symptoms and signs}} | |||
{{External causes of morbidity and mortality}} | |||
[[Category:Drug eruptions| ]] | |||
[[Category:Clinical pharmacology]] | |||
[[Category:Dermatology]] | [[Category:Dermatology]] | ||
[[Category:Adverse drug reactions]] | [[Category:Adverse drug reactions]] | ||
Latest revision as of 19:17, 5 April 2025

Editor-In-Chief: Prab R Tumpati, MD
Obesity, Sleep & Internal medicine
Founder, WikiMD Wellnesspedia &
W8MD medical weight loss NYC and sleep center NYC
| Drug eruption | |
|---|---|
| |
| Synonyms | Drug rash, medication rash |
| Pronounce | N/A |
| Specialty | N/A |
| Symptoms | Rash, itching, redness, swelling |
| Complications | Anaphylaxis, Stevens-Johnson syndrome, toxic epidermal necrolysis |
| Onset | Varies, typically within days to weeks of starting a new medication |
| Duration | Varies, often resolves after discontinuation of the offending drug |
| Types | N/A |
| Causes | Adverse drug reaction |
| Risks | Previous drug reactions, multiple medications, autoimmune disease |
| Diagnosis | Clinical evaluation, skin biopsy, allergy testing |
| Differential diagnosis | Viral exanthem, contact dermatitis, psoriasis |
| Prevention | N/A |
| Treatment | Discontinuation of the offending drug, antihistamines, corticosteroids |
| Medication | Antihistamines, corticosteroids |
| Prognosis | Generally good with appropriate management |
| Frequency | Common, varies with drug and population |
| Deaths | N/A |
An adverse reaction to a medication manifesting on the skin
A drug eruption is a type of adverse drug reaction that manifests as a skin condition. These eruptions can vary widely in appearance and severity, ranging from mild rashes to severe, life-threatening conditions. Drug eruptions are a common reason for dermatological consultations and can be caused by a wide variety of medications.
Pathophysiology[edit]
Drug eruptions occur when the body's immune system reacts to a medication. This reaction can be mediated by different immunological mechanisms, including IgE-mediated hypersensitivity, T-cell mediated reactions, and immune complex formation. The specific mechanism often determines the type and severity of the eruption.
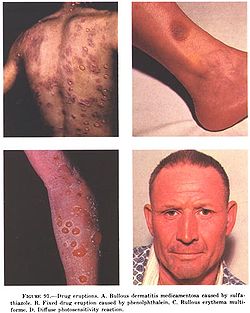
Types of Drug Eruptions[edit]
Exanthematous Eruptions[edit]
Exanthematous eruptions, also known as maculopapular rashes, are the most common type of drug eruption. They typically appear as widespread red spots and bumps on the skin and are usually symmetrical. These eruptions are often benign and resolve after discontinuation of the offending drug.
Urticarial Eruptions[edit]
Urticaria, or hives, are raised, itchy welts on the skin that can be caused by drug reactions. These eruptions are often associated with IgE-mediated hypersensitivity and can occur rapidly after drug exposure.
Fixed Drug Eruptions[edit]
A fixed drug eruption is characterized by a well-defined, round or oval patch that recurs at the same site each time the drug is taken. These lesions can be red, purple, or brown and may blister.
Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis[edit]
Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN) are severe, life-threatening drug eruptions. They involve widespread skin detachment and mucous membrane involvement. These conditions require immediate medical attention and often hospitalization.
Diagnosis[edit]
The diagnosis of a drug eruption is primarily clinical, based on the patient's history and the appearance of the skin lesions. A detailed medication history is crucial, including over-the-counter drugs and supplements. In some cases, skin biopsy or patch testing may be used to confirm the diagnosis.
Management[edit]
The primary treatment for drug eruptions is the discontinuation of the offending medication. Supportive care, such as antihistamines for itching or corticosteroids for inflammation, may be provided. In severe cases, such as SJS or TEN, hospitalization and intensive care may be necessary.
Prevention[edit]
Preventing drug eruptions involves careful prescribing practices, including reviewing patient allergies and previous drug reactions. Patients should be educated about the potential for drug eruptions and advised to report any new skin changes promptly.
See also[edit]
External links[edit]
| Diseases of the skin and appendages by morphology | ||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| Dermatitis and eczema | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| Urticaria and erythema | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| Signs and symptoms relating to skin and subcutaneous tissue | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| Adverse drug reactions | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|