Crouzon syndrome
Genetic disorder of the skull and face
| Crouzon syndrome | |
|---|---|

| |
| Synonyms | |
| Pronounce | |
| Field | Medical genetics |
| Symptoms | |
| Complications | |
| Onset | |
| Duration | |
| Types | |
| Causes | |
| Risks | |
| Diagnosis | |
| Differential diagnosis | |
| Prevention | |
| Treatment | |
| Medication | |
| Prognosis | |
| Frequency | |
| Deaths | |
Crouzon syndrome is an autosomal dominant genetic disorder known as a branchial arch syndrome. Specifically, this syndrome affects the first branchial (or pharyngeal) arch, which is the precursor of the maxilla and mandible. Since the branchial arches are important developmental features in a growing embryo, disturbances in their development create lasting and widespread effects.
This syndrome is named after Octave Crouzon,<ref>synd/1383 at Who Named It?</ref><ref>L. E. O. Crouzon. Dysostose cranio-faciale héréditaire. Bulletin de la Société des Médecins des Hôpitaux de Paris, 1912, 33: 545-555.</ref> a French physician who first described this disorder. First called "craniofacial dysostosis" ("craniofacial" refers to the skull and face, and "dysostosis" refers to malformation of bone), the disorder was characterized by a number of clinical features which can be described by the rudimentary meanings of its former name. This syndrome is caused by a mutation in the fibroblast growth factor receptor 2 (FGFR2), located on chromosome 10. The developing fetus's skull and facial bones fuse early or are unable to expand. Thus, normal bone growth cannot occur. Fusion of different sutures leads to abnormal patterns of growth of the skull.
Signs and symptoms

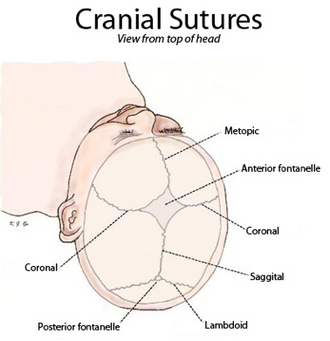
A defining characteristic of Crouzon syndrome is craniosynostosis, which results in an abnormal head shape. This is present in combinations of: turricephaly, frontal bossing, trigonocephaly (fusion of the metopic suture), brachycephaly (fusion of the coronal suture), dolichocephaly (fusion of the sagittal suture), plagiocephaly (unilateral premature closure of lambdoid and coronal sutures), oxycephaly (fusion of coronal and lambdoidal sutures), and complex craniosynostosis (premature closure of some or all sutures).
Exophthalmos (bulging eyes due to shallow eye sockets after early fusion of surrounding bones), hypertelorism (greater than normal distance between the eyes), and psittichorhina (beak-like nose) are also very common features. Other facial characteristics that are present in many cases include external strabismus and hypoplastic maxilla (insufficient growth of the midface), which results in relative mandibular prognathism (protruding chin) and gives the effect of the patient having a concave face.<ref name="nih">
Crouzon syndrome | Genetic and Rare Diseases Information Center (GARD) – an NCATS Program(link). rarediseases.info.nih.gov.
</ref>
Most symptoms are secondary to the abnormal skull structure. Approximately 30% of people with Crouzon syndrome develop hydrocephalus. Sensorineural hearing loss is present in some cases. The abnormalities in the manner in which the eyes fit in the eye sockets can cause vision problems, the most common of which is corneal exposure that can lead to visual impairment.<ref>,
Ophthalmic sequelae of Crouzon syndrome, Ophthalmology, Vol. 112, pp. 1129–1134,</ref> Some people with the condition have a restricted airway and can experience severe problems breathing.<ref name="nord">
Crouzon Syndrome - NORD (National Organization for Rare Disorders)(link). NORD (National Organization for Rare Disorders).
</ref>
Common features are a narrow/high-arched palate, posterior bilateral crossbite, hypodontia (missing some teeth), and crowding of teeth. Due to maxillary hypoplasia, people with Crouzon syndrome generally have a considerable permanent underbite.<ref>,
Cummings Otolaryngology, 6 edition, Elsevier, Pages: 2891–2914,</ref>
Causes
The current research indicates fibroblast growth factor receptors (FGFR) FGFR2 and FGFR3 as the leading factors in causing the autosomal dominant Crouzon syndrome.<ref name="pmid20133659">,
Analysis of a gain-of-function FGFR2 Crouzon mutation provides evidence of loss of function activity in the etiology of cleft palate, Proc. Natl. Acad. Sci. U.S.A., Vol. 107(Issue: 6), pp. 2515–20, DOI: 10.1073/pnas.0913985107, PMID: 20133659, PMC: 2823872,</ref><ref name=ghr/> These two transmembrane proteins are two of four fibroblast growth factor receptors involved in osteoblast differentiation during embryonic development; mutations amongst these receptors are involved in several genetic disorders.<ref name="pmid20133659"/> There are 40 known mutations, most of which are caused by a missense mutation.<ref name="pmid25174698">, Apparently synonymous substitutions in FGFR2 affect splicing and result in mild Crouzon syndrome, BMC Med. Genet., Vol. 15, pp. 95, DOI: 10.1186/s12881-014-0095-4, PMID: 25174698, PMC: 4236556,</ref> FGFR2 is the most commonly mutated gene, a missense at cysteine 342 in exon 9, which creates a gain-of-function.<ref name="pmid25174698"/> The FGFR2lllc isoform, created via alternative splicing of exon 3 of the FGFR2 gene, uses exon 9 and is used in mesenchymal stem cells to control ossification. However, the mutation constitutively activates the transmembrane protein via a disulfide bond formed incorrectly due to the loss of cysteine 342.<ref name="pmid25174698"/> FGFR3 is expressed more in the frontal bones during embryonic development, guiding cranial bone development. A point mutation causes constitutive activation of tyrosine in the activation loop, located in the cytosolic region of the protein, leading to accelerated differentiation of frontal osteoblasts,<ref name="pmid24419316">, FGFR3 mutation causes abnormal membranous ossification in achondroplasia, Hum. Mol. Genet., Vol. 23(Issue: 11), pp. 2914–25, DOI: 10.1093/hmg/ddu004, PMID: 24419316,</ref> resulting in premature fusion of frontal cranial bones.<ref name="pmid24419316"/>
Diagnosis
Diagnosis of Crouzon syndrome usually can occur at birth by assessing the physical appearance of the infant. Further analysis, including radiographs, magnetic resonance imaging (MRI) scans, genetic testing, X-rays and CT scans can be used to confirm the diagnosis of Crouzon syndrome. (November 2018)
Treatment

Surgery is typically used to prevent the closure of sutures of the skull from damaging the brain's development. Without surgery, blindness and intellectual disability are typical outcomes. To move the orbits forward, surgeons expose the skull and orbits and reshape the bone. To treat the midface deficiency, surgeons can move the lower orbit and midface bones forward. (November 2018)
People with Crouzon syndrome tend to have multiple sutures involved, most specifically bilateral coronal craniosynostoses, and either open vault surgery or strip craniectomy (if child is under 6 months) can be performed. In the later scenario, a helmet is worn for several months following surgery.
(November 2018)
Once treated for the cranial vault abnormalities, Crouzon patients generally go on to live a normal lifespan.
(November 2018)
Epidemiology
Incidence of Crouzon syndrome is currently estimated to occur in 1.6 out of every 100,000 people<ref name="pmid20301628">,
FGFR-Related Craniosynostosis Syndromes., GeneReviews, PMID: 20301628,</ref> and is the most common craniostenosis syndrome.<ref name="ghr">
Crouzon syndrome(link). Genetics Home Reference.
</ref>
History
Crouzon syndrome was first described by Octave Crouzon in 1912.<ref name="rodriguez">,
Plastic Surgery: Volume 3: Craniofacial, Head and Neck Surgery and Pediatric Plastic Surgery, 4 edition, Elsevier,</ref> He noted the affected patients were a mother and her daughter, implying a genetic basis.
See also
References
<references group="" responsive="1"></references>
External links
- Crouzon syndrome on Genetics Home Reference from U.S. National Library of Medicine & National Institutes of Health
- GeneReviews/NIH/NCBI/UW entry on FGFR-Related Craniosynostosis Syndromes
| Congenital malformations and deformations of musculoskeletal system / musculoskeletal abnormality | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Ad. Transform your life with W8MD's Budget GLP-1 injections from $75


W8MD offers a medical weight loss program to lose weight in Philadelphia. Our physician-supervised medical weight loss provides:
- Weight loss injections in NYC (generic and brand names):
- Zepbound / Mounjaro, Wegovy / Ozempic, Saxenda
- Most insurances accepted or discounted self-pay rates. We will obtain insurance prior authorizations if needed.
- Generic GLP1 weight loss injections from $75 for the starting dose.
- Also offer prescription weight loss medications including Phentermine, Qsymia, Diethylpropion, Contrave etc.
NYC weight loss doctor appointmentsNYC weight loss doctor appointments
Start your NYC weight loss journey today at our NYC medical weight loss and Philadelphia medical weight loss clinics.
- Call 718-946-5500 to lose weight in NYC or for medical weight loss in Philadelphia 215-676-2334.
- Tags:NYC medical weight loss, Philadelphia lose weight Zepbound NYC, Budget GLP1 weight loss injections, Wegovy Philadelphia, Wegovy NYC, Philadelphia medical weight loss, Brookly weight loss and Wegovy NYC
|
WikiMD's Wellness Encyclopedia |
| Let Food Be Thy Medicine Medicine Thy Food - Hippocrates |
Medical Disclaimer: WikiMD is not a substitute for professional medical advice. The information on WikiMD is provided as an information resource only, may be incorrect, outdated or misleading, and is not to be used or relied on for any diagnostic or treatment purposes. Please consult your health care provider before making any healthcare decisions or for guidance about a specific medical condition. WikiMD expressly disclaims responsibility, and shall have no liability, for any damages, loss, injury, or liability whatsoever suffered as a result of your reliance on the information contained in this site. By visiting this site you agree to the foregoing terms and conditions, which may from time to time be changed or supplemented by WikiMD. If you do not agree to the foregoing terms and conditions, you should not enter or use this site. See full disclaimer.
Credits:Most images are courtesy of Wikimedia commons, and templates, categories Wikipedia, licensed under CC BY SA or similar.
Translate this page: - East Asian
中文,
日本,
한국어,
South Asian
हिन्दी,
தமிழ்,
తెలుగు,
Urdu,
ಕನ್ನಡ,
Southeast Asian
Indonesian,
Vietnamese,
Thai,
မြန်မာဘာသာ,
বাংলা
European
español,
Deutsch,
français,
Greek,
português do Brasil,
polski,
română,
русский,
Nederlands,
norsk,
svenska,
suomi,
Italian
Middle Eastern & African
عربى,
Turkish,
Persian,
Hebrew,
Afrikaans,
isiZulu,
Kiswahili,
Other
Bulgarian,
Hungarian,
Czech,
Swedish,
മലയാളം,
मराठी,
ਪੰਜਾਬੀ,
ગુજરાતી,
Portuguese,
Ukrainian


