Prolactinoma: Difference between revisions
No edit summary Tag: visualeditor-wikitext |
CSV import |
||
| Line 1: | Line 1: | ||
'''Other Names:''' Lactotroph adenoma; Pituitary lactotrophic adenoma; PRL-secreting pituitary adenoma; PRLoma; Prolactin-secreting pituitary adenoma; Forbes-Albright syndrome (formerly); Prolactin-Producing Pituitary Gland Adenoma | {{SI}} | ||
{{Infobox medical condition | |||
| name = Prolactinoma | |||
| image = [[File:PRL_HE_histology.jpg|250px]] | |||
| caption = Histopathology of a prolactinoma | |||
| field = [[Endocrinology]] | |||
| synonyms = Prolactin-secreting pituitary adenoma | |||
| symptoms = [[Galactorrhea]], [[amenorrhea]], [[infertility]], [[erectile dysfunction]], [[headache]], [[visual field defects]] | |||
| complications = [[Osteoporosis]], [[hypogonadism]] | |||
| onset = Typically in [[adulthood]] | |||
| duration = Chronic | |||
| causes = [[Pituitary adenoma]] | |||
| risks = [[Multiple endocrine neoplasia type 1]] | |||
| diagnosis = [[Blood test]] for [[prolactin]] levels, [[MRI]] of the [[pituitary gland]] | |||
| differential = [[Hypothyroidism]], [[pregnancy]], [[medication side effects]] | |||
| treatment = [[Dopamine agonists]], [[surgery]], [[radiation therapy]] | |||
| medication = [[Cabergoline]], [[bromocriptine]] | |||
| prognosis = Generally good with treatment | |||
| frequency = Most common type of [[functioning pituitary adenoma]] | |||
}} | |||
'''Other Names:''' Lactotroph adenoma; Pituitary lactotrophic adenoma; PRL-secreting pituitary adenoma; PRLoma; Prolactin-secreting pituitary adenoma; Forbes-Albright syndrome (formerly); Prolactin-Producing Pituitary Gland Adenoma | |||
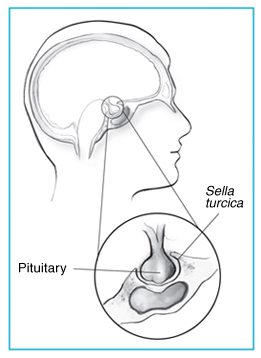
A prolactinoma is a benign (noncancerous) [[tumor]] of the [[pituitary gland]] that produces a hormone called [[prolactin]]. Located at the base of the brain, the pituitary is a pea-sized gland that controls the production of many hormones. | A prolactinoma is a benign (noncancerous) [[tumor]] of the [[pituitary gland]] that produces a hormone called [[prolactin]]. Located at the base of the brain, the pituitary is a pea-sized gland that controls the production of many hormones. | ||
Prolactin signals a | Prolactin signals a woman’s breasts to produce milk during pregnancy and breastfeeding. Having too much prolactin in the blood, a condition called [[hyperprolactinemia]], can cause [[infertility]] and other problems. In most cases, prolactinomas and related health problems can be successfully treated with medicines. | ||
[[File:Prolactinoma-art.jpg|thumb]] | [[File:Prolactinoma-art.jpg|left|thumb]] | ||
<youtube> | <youtube> | ||
title='''{{PAGENAME}}''' | title='''{{PAGENAME}}''' | ||
| Line 15: | Line 33: | ||
height=600 | height=600 | ||
</youtube> | </youtube> | ||
== '''Epidemiology''' == | == '''Epidemiology''' == | ||
Small, benign pituitary tumors are fairly common in the general population. A prolactinoma is the most common type of pituitary tumor, making up about 40 percent of all pituitary tumors. | Small, benign pituitary tumors are fairly common in the general population. A prolactinoma is the most common type of pituitary tumor, making up about 40 percent of all pituitary tumors. | ||
== '''Risk factors''' == | == '''Risk factors''' == | ||
Women are more likely than men to develop a prolactinoma. These tumors rarely occur in children and adolescents. In children, prolactinomas may prevent the start or block the progression of [[puberty]]. | Women are more likely than men to develop a prolactinoma. These tumors rarely occur in children and adolescents. In children, prolactinomas may prevent the start or block the progression of [[puberty]]. | ||
'''Cause''' | '''Cause''' | ||
Prolactin levels normally rise during pregnancy and breastfeeding. They may also rise slightly at other times because of1 | Prolactin levels normally rise during pregnancy and breastfeeding. They may also rise slightly at other times because of1 | ||
| Line 32: | Line 47: | ||
* [[epileptic seizures]] | * [[epileptic seizures]] | ||
These increases in [[prolactin]] are usually small and temporary. Other than a prolactinoma, the factors that most often lead to excess prolactin in the blood are medicines, illnesses, and other pituitary tumors. | These increases in [[prolactin]] are usually small and temporary. Other than a prolactinoma, the factors that most often lead to excess prolactin in the blood are medicines, illnesses, and other pituitary tumors. | ||
'''Medicines.''' The brain chemical [[dopamine]] helps curb the production of prolactin in the body. Any medicine that affects the production or use of dopamine can make prolactin levels rise. | '''Medicines.''' The brain chemical [[dopamine]] helps curb the production of prolactin in the body. Any medicine that affects the production or use of dopamine can make prolactin levels rise. | ||
Medicines that can increase prolactin levels include some types of | Medicines that can increase prolactin levels include some types of | ||
* [[antipsychotic]] medicines , such as [[risperidone]], but not others, such as [[clozapine]]. | * [[antipsychotic]] medicines , such as [[risperidone]], but not others, such as [[clozapine]]. | ||
| Line 42: | Line 55: | ||
* Although the hormone [[estrogen]] stimulates the release of prolactin, estrogen-containing birth control pills and [[hormone replacement therapy]] have not been found to cause hyperprolactinemia. | * Although the hormone [[estrogen]] stimulates the release of prolactin, estrogen-containing birth control pills and [[hormone replacement therapy]] have not been found to cause hyperprolactinemia. | ||
* If high prolactin levels are because of a medicine, these levels will usually return to normal 3 to 4 days after the drug is stopped. | * If high prolactin levels are because of a medicine, these levels will usually return to normal 3 to 4 days after the drug is stopped. | ||
'''Other illnesses.''' Illnesses that may increase prolactin levels include | '''Other illnesses.''' Illnesses that may increase prolactin levels include | ||
* kidney disease | * kidney disease | ||
* an underactive thyroid, or hypothyroidism | * an underactive thyroid, or hypothyroidism | ||
* [[shingles]] particularly when lesions affect your chest | * [[shingles]] particularly when lesions affect your chest | ||
'''Other pituitary tumors.''' Other large tumors located in or near the [[pituitary gland]] may also raise prolactin levels, usually by preventing [[dopamine]] from reaching the pituitary gland. | '''Other pituitary tumors.''' Other large tumors located in or near the [[pituitary gland]] may also raise prolactin levels, usually by preventing [[dopamine]] from reaching the pituitary gland. | ||
Sometimes the cause of excess prolactin is unknown. | Sometimes the cause of excess prolactin is unknown. | ||
== '''Signs and symptoms''' == | == '''Signs and symptoms''' == | ||
Among women, common symptoms of having a prolactinoma include | Among women, common symptoms of having a prolactinoma include | ||
| Line 57: | Line 67: | ||
* milky discharge from the breasts, also called galactorrhea | * milky discharge from the breasts, also called galactorrhea | ||
* loss of interest in sex | * loss of interest in sex | ||
* pain or discomfort during sex due to vaginal dryness | * pain or discomfort during sex due to vaginal dryness | ||
Among men, common symptoms include | Among men, common symptoms include | ||
* loss of interest in sex associated with low levels of [[testosterone]] | * loss of interest in sex associated with low levels of [[testosterone]] | ||
* [[erectile]] dysfunction | * [[erectile]] dysfunction | ||
Women often report symptoms earlier than men because they may notice changes in their periods or milky discharge from their breasts when they are not pregnant or breastfeeding. But women who are taking sex hormones—in birth control pills or [[hormone replacement therapy]] —may not experience these changes. | |||
Women often report symptoms earlier than men because they may notice changes in their periods or milky discharge from their breasts when they are not pregnant or breastfeeding. But women who are taking sex | |||
The same is true for women who have reached menopause and no longer have periods. Among these women, and among men, a lack of clear signs and symptoms may lead to a delayed diagnosis. | The same is true for women who have reached menopause and no longer have periods. Among these women, and among men, a lack of clear signs and symptoms may lead to a delayed diagnosis. | ||
== '''Diagnosis''' == | == '''Diagnosis''' == | ||
Doctors diagnose prolactinomas based on the results of two tests | Doctors diagnose prolactinomas based on the results of two tests | ||
'''Blood test.''' The prolactin blood test will measure the level of [[prolactin]] in your blood. If the level is too high, your doctor will order an imaging test to detect a possible tumor. | '''Blood test.''' The prolactin blood test will measure the level of [[prolactin]] in your blood. If the level is too high, your doctor will order an imaging test to detect a possible tumor. | ||
'''Imaging tests.''' The preferred test is the [[magnetic resonance imaging]] (MRI) scan , which uses radio waves and magnets to create detailed images of your internal organs and soft tissues without x-rays. If an MRI is not a good option for you (for example, if you have a pacemaker or other implant that has metal), your doctor may order a [[computed tomography]] (CT) scan instead. The results of the imaging test usually will allow your doctor to confirm a diagnosis of prolactinoma and determine its size and location. | '''Imaging tests.''' The preferred test is the [[magnetic resonance imaging]] (MRI) scan , which uses radio waves and magnets to create detailed images of your internal organs and soft tissues without x-rays. If an MRI is not a good option for you (for example, if you have a pacemaker or other implant that has metal), your doctor may order a [[computed tomography]] (CT) scan instead. The results of the imaging test usually will allow your doctor to confirm a diagnosis of prolactinoma and determine its size and location. | ||
After confirming the prolactinoma diagnosis, your doctor may conduct other tests to find out if the tumor is affecting other hormones. Depending on the tumor’s size, your doctor may also ask you to take a vision test. | |||
After confirming the prolactinoma diagnosis, your doctor may conduct other tests to find out if the tumor is affecting other hormones. Depending on the | |||
== '''Treatment''' == | == '''Treatment''' == | ||
Doctors commonly treat prolactinomas with medicines. More rarely, [[surgery]] or [[radiation therapy]] may be used. The goals of treatment are to | Doctors commonly treat prolactinomas with medicines. More rarely, [[surgery]] or [[radiation therapy]] may be used. The goals of treatment are to | ||
* bring [[prolactin]] levels back to normal | * bring [[prolactin]] levels back to normal | ||
* shrink the [[tumor]] | * shrink the [[tumor]] | ||
* make sure the [[pituitary gland]] is working properly | * make sure the [[pituitary gland]] is working properly | ||
* correct any problems caused by the tumor, such as menstrual problems, milky discharge from the breasts, low testosterone levels, headaches, or vision problems | * correct any problems caused by the tumor, such as menstrual problems, milky discharge from the breasts, low testosterone levels, headaches, or vision problems | ||
=== '''Medicines''' === | === '''Medicines''' === | ||
Medicines called [[dopamine]] agonists control prolactin levels and shrink the tumor very effectively. These drugs mimic the effects of the brain chemical dopamine. | Medicines called [[dopamine]] agonists control prolactin levels and shrink the tumor very effectively. These drugs mimic the effects of the brain chemical dopamine. | ||
Two '''dopamine agonists''' are most commonly used to treat prolactinomas | Two '''dopamine agonists''' are most commonly used to treat prolactinomas | ||
*''' [[bromocriptine]]''' , a drug that must be taken twice or three times daily | *''' [[bromocriptine]]''' , a drug that must be taken twice or three times daily | ||
*''' [[cabergoline]] ''', a drug that can be taken once or twice per week | *''' [[cabergoline]] ''', a drug that can be taken once or twice per week | ||
Cabergoline is the preferred drug for treating prolactinomas, because it is more effective than bromocriptine and has fewer side effects.1 | Cabergoline is the preferred drug for treating prolactinomas, because it is more effective than bromocriptine and has fewer side effects.1 | ||
'''Outcomes.''' For most small prolactinomas, dopamine agonists bring prolactin levels back to normal and shrink tumors in 4 out of 5 patients.5 | '''Outcomes.''' For most small prolactinomas, dopamine agonists bring prolactin levels back to normal and shrink tumors in 4 out of 5 patients.5 | ||
'''Side effects. '''Common side effects of the drugs include nausea, vomiting, and dizziness. Both medicines should always be taken with food. Starting treatment at a low dose and taking the medicine at bedtime can reduce side effects. | '''Side effects. '''Common side effects of the drugs include nausea, vomiting, and dizziness. Both medicines should always be taken with food. Starting treatment at a low dose and taking the medicine at bedtime can reduce side effects. | ||
'''Complications.''' Although dopamine agonists have been linked to heart valve damage, these problems were found mainly among people taking these medicines to treat Parkinson’s disease . These patients typically take much higher doses (usually about 10 times higher) of these medicines than are used to treat prolactinomas. If you need to take a high dose of a dopamine agonist, your doctor may order an echocardiogram (echo) to check your heart valves and heart function. Rarely, psychiatric disorders related to impulse control, such as compulsive gambling , have been seen in people taking these medicines.6 | |||
'''Complications.''' Although dopamine agonists have been linked to heart valve damage, these problems were found mainly among people taking these medicines to treat | |||
'''Duration of treatment.''' You may have to take these medicines for a long time to prevent the tumor from growing back, especially if the prolactinoma is large. After 2 years, the medicines may be slowly reduced and stopped if prolactin levels are normal and the tumor is no longer visible.1 But if your prolactin level goes back up again, you may need to go back on the medicine for as long as needed to bring your prolactin level under control. | '''Duration of treatment.''' You may have to take these medicines for a long time to prevent the tumor from growing back, especially if the prolactinoma is large. After 2 years, the medicines may be slowly reduced and stopped if prolactin levels are normal and the tumor is no longer visible.1 But if your prolactin level goes back up again, you may need to go back on the medicine for as long as needed to bring your prolactin level under control. | ||
=== '''Surgery''' === | === '''Surgery''' === | ||
Although doctors most often treat prolactinomas with medicines, in some cases surgery may be an option. Examples include | Although doctors most often treat prolactinomas with medicines, in some cases surgery may be an option. Examples include | ||
* you | * you can’t tolerate the medicines | ||
* the medicines | * the medicines aren’t working for you | ||
* you take antipsychotic medicines that interact with the medicines used to treat prolactinomas | * you take antipsychotic medicines that interact with the medicines used to treat prolactinomas | ||
* In some cases, when a prolactinoma is large, a woman may choose to have surgery to remove the tumor before trying to become pregnant. | * In some cases, when a prolactinoma is large, a woman may choose to have surgery to remove the tumor before trying to become pregnant. | ||
Two types of surgery may be used | Two types of surgery may be used | ||
'''[[Transsphenoidal surgery]]''' is most commonly used to treat prolactinoma. The surgery is done through an incision, or cut, at the back of the nasal cavity or under the upper lip. | '''[[Transsphenoidal surgery]]''' is most commonly used to treat prolactinoma. The surgery is done through an incision, or cut, at the back of the nasal cavity or under the upper lip. | ||
Transcranial surgery is used more rarely if the tumor is large or has spread to other areas. The surgeon removes the tumor through an opening in the skull. | Transcranial surgery is used more rarely if the tumor is large or has spread to other areas. The surgeon removes the tumor through an opening in the skull. | ||
More rarely, if medicines and surgery fail to reduce prolactin levels, radiation therapy may be used. This type of treatment uses high-energy x-rays or particle waves to kill tumor cells. Depending on the size and location of the tumor, the total radiation dose is delivered in one session, or in lower doses over the course of 4 to 6 weeks. | More rarely, if medicines and surgery fail to reduce prolactin levels, radiation therapy may be used. This type of treatment uses high-energy x-rays or particle waves to kill tumor cells. Depending on the size and location of the tumor, the total radiation dose is delivered in one session, or in lower doses over the course of 4 to 6 weeks. | ||
'''Outcomes.''' Prolactin levels return to normal in 1 out of 3 patients treated with radiation therapy.1 However, as radiation treatment lowers prolactin levels over time, it may take years to reach this outcome. Your doctor is likely to prescribe medicines while you wait to see results. | '''Outcomes.''' Prolactin levels return to normal in 1 out of 3 patients treated with radiation therapy.1 However, as radiation treatment lowers prolactin levels over time, it may take years to reach this outcome. Your doctor is likely to prescribe medicines while you wait to see results. | ||
'''Side effects and complications.''' The most common side effect is low levels of thyroid hormone. In up to half of patients, radiation therapy may also lead to a decrease in other pituitary hormones.8 Vision loss and brain injury are rare complications. Rarely, other types of tumors can develop many years later in areas that were in the path of the radiation beam. | '''Side effects and complications.''' The most common side effect is low levels of thyroid hormone. In up to half of patients, radiation therapy may also lead to a decrease in other pituitary hormones.8 Vision loss and brain injury are rare complications. Rarely, other types of tumors can develop many years later in areas that were in the path of the radiation beam. | ||
'''When pregnancy is confirmed.''' Although studies suggest that both bromocriptine and [[cabergoline[[ can be safely taken in the early stages of pregnancy, [[bromocriptine]] is typically preferred because of its longer safety record. As soon as your pregnancy is confirmed, your doctor will usually advise you to stop taking these medicines to prevent any possible effects on the fetus. | '''When pregnancy is confirmed.''' Although studies suggest that both bromocriptine and [[cabergoline[[ can be safely taken in the early stages of pregnancy, [[bromocriptine]] is typically preferred because of its longer safety record. As soon as your pregnancy is confirmed, your doctor will usually advise you to stop taking these medicines to prevent any possible effects on the fetus. | ||
'''During pregnancy.''' Prolactin levels normally increase during pregnancy, preparing your breasts to make milk after your baby is born. The [[pituitary gland]] often doubles in size during pregnancy. Your prolactinoma may also grow in size, especially if it is already large. If you begin to have symptoms such as headaches and changes in vision, your doctor may recommend that you start taking the medicine again. | '''During pregnancy.''' Prolactin levels normally increase during pregnancy, preparing your breasts to make milk after your baby is born. The [[pituitary gland]] often doubles in size during pregnancy. Your prolactinoma may also grow in size, especially if it is already large. If you begin to have symptoms such as headaches and changes in vision, your doctor may recommend that you start taking the medicine again. | ||
'''After delivery.''' After delivery, women with small prolactinomas can usually nurse their babies. If your prolactinoma is large, your doctor may suggest that you consult with an [[endocrinologist]] about breastfeeding. | '''After delivery.''' After delivery, women with small prolactinomas can usually nurse their babies. If your prolactinoma is large, your doctor may suggest that you consult with an [[endocrinologist]] about breastfeeding. | ||
Doctors don’t usually measure [[prolactin]] levels during pregnancy and breastfeeding. Your doctor will usually begin to do so again a couple of months after you stop nursing. In some cases, prolactin levels remain normal after delivery and nursing. | |||
Doctors | |||
{{Tumor histology}} | {{Tumor histology}} | ||
{{Endocrine gland neoplasia}} | {{Endocrine gland neoplasia}} | ||
[[Category:Endocrine neoplasia]] | [[Category:Endocrine neoplasia]] | ||
{{rarediseases}} | {{rarediseases}} | ||
{{stub}} | {{stub}} | ||
Revision as of 20:20, 8 April 2025

Editor-In-Chief: Prab R Tumpati, MD
Obesity, Sleep & Internal medicine
Founder, WikiMD Wellnesspedia &
W8MD medical weight loss NYC and sleep center NYC
| Prolactinoma | |
|---|---|

| |
| Synonyms | Prolactin-secreting pituitary adenoma |
| Pronounce | N/A |
| Specialty | N/A |
| Symptoms | Galactorrhea, amenorrhea, infertility, erectile dysfunction, headache, visual field defects |
| Complications | Osteoporosis, hypogonadism |
| Onset | Typically in adulthood |
| Duration | Chronic |
| Types | N/A |
| Causes | Pituitary adenoma |
| Risks | Multiple endocrine neoplasia type 1 |
| Diagnosis | Blood test for prolactin levels, MRI of the pituitary gland |
| Differential diagnosis | Hypothyroidism, pregnancy, medication side effects |
| Prevention | N/A |
| Treatment | Dopamine agonists, surgery, radiation therapy |
| Medication | Cabergoline, bromocriptine |
| Prognosis | Generally good with treatment |
| Frequency | Most common type of functioning pituitary adenoma |
| Deaths | N/A |
Other Names: Lactotroph adenoma; Pituitary lactotrophic adenoma; PRL-secreting pituitary adenoma; PRLoma; Prolactin-secreting pituitary adenoma; Forbes-Albright syndrome (formerly); Prolactin-Producing Pituitary Gland Adenoma
A prolactinoma is a benign (noncancerous) tumor of the pituitary gland that produces a hormone called prolactin. Located at the base of the brain, the pituitary is a pea-sized gland that controls the production of many hormones.
Prolactin signals a woman’s breasts to produce milk during pregnancy and breastfeeding. Having too much prolactin in the blood, a condition called hyperprolactinemia, can cause infertility and other problems. In most cases, prolactinomas and related health problems can be successfully treated with medicines.
Epidemiology
Small, benign pituitary tumors are fairly common in the general population. A prolactinoma is the most common type of pituitary tumor, making up about 40 percent of all pituitary tumors.
Risk factors
Women are more likely than men to develop a prolactinoma. These tumors rarely occur in children and adolescents. In children, prolactinomas may prevent the start or block the progression of puberty. Cause Prolactin levels normally rise during pregnancy and breastfeeding. They may also rise slightly at other times because of1
- physical stress, such as a painful blood draw
- exercise
- a meal
- sexual intercourse
- nipple stimulation
- injury to the chest area
- epileptic seizures
These increases in prolactin are usually small and temporary. Other than a prolactinoma, the factors that most often lead to excess prolactin in the blood are medicines, illnesses, and other pituitary tumors. Medicines. The brain chemical dopamine helps curb the production of prolactin in the body. Any medicine that affects the production or use of dopamine can make prolactin levels rise. Medicines that can increase prolactin levels include some types of
- antipsychotic medicines , such as risperidone, but not others, such as clozapine.
- high blood pressure medicines
- drugs used to treat nausea and vomiting
- pain relievers that contain opioids.
- Although the hormone estrogen stimulates the release of prolactin, estrogen-containing birth control pills and hormone replacement therapy have not been found to cause hyperprolactinemia.
- If high prolactin levels are because of a medicine, these levels will usually return to normal 3 to 4 days after the drug is stopped.
Other illnesses. Illnesses that may increase prolactin levels include
- kidney disease
- an underactive thyroid, or hypothyroidism
- shingles particularly when lesions affect your chest
Other pituitary tumors. Other large tumors located in or near the pituitary gland may also raise prolactin levels, usually by preventing dopamine from reaching the pituitary gland. Sometimes the cause of excess prolactin is unknown.
Signs and symptoms
Among women, common symptoms of having a prolactinoma include
- changes in menstruation , such as irregular periods or no periods
- infertility
- milky discharge from the breasts, also called galactorrhea
- loss of interest in sex
- pain or discomfort during sex due to vaginal dryness
Among men, common symptoms include
- loss of interest in sex associated with low levels of testosterone
- erectile dysfunction
Women often report symptoms earlier than men because they may notice changes in their periods or milky discharge from their breasts when they are not pregnant or breastfeeding. But women who are taking sex hormones—in birth control pills or hormone replacement therapy —may not experience these changes. The same is true for women who have reached menopause and no longer have periods. Among these women, and among men, a lack of clear signs and symptoms may lead to a delayed diagnosis.
Diagnosis
Doctors diagnose prolactinomas based on the results of two tests Blood test. The prolactin blood test will measure the level of prolactin in your blood. If the level is too high, your doctor will order an imaging test to detect a possible tumor. Imaging tests. The preferred test is the magnetic resonance imaging (MRI) scan , which uses radio waves and magnets to create detailed images of your internal organs and soft tissues without x-rays. If an MRI is not a good option for you (for example, if you have a pacemaker or other implant that has metal), your doctor may order a computed tomography (CT) scan instead. The results of the imaging test usually will allow your doctor to confirm a diagnosis of prolactinoma and determine its size and location. After confirming the prolactinoma diagnosis, your doctor may conduct other tests to find out if the tumor is affecting other hormones. Depending on the tumor’s size, your doctor may also ask you to take a vision test.
Treatment
Doctors commonly treat prolactinomas with medicines. More rarely, surgery or radiation therapy may be used. The goals of treatment are to
- bring prolactin levels back to normal
- shrink the tumor
- make sure the pituitary gland is working properly
- correct any problems caused by the tumor, such as menstrual problems, milky discharge from the breasts, low testosterone levels, headaches, or vision problems
Medicines
Medicines called dopamine agonists control prolactin levels and shrink the tumor very effectively. These drugs mimic the effects of the brain chemical dopamine. Two dopamine agonists are most commonly used to treat prolactinomas
- bromocriptine , a drug that must be taken twice or three times daily
- cabergoline , a drug that can be taken once or twice per week
Cabergoline is the preferred drug for treating prolactinomas, because it is more effective than bromocriptine and has fewer side effects.1 Outcomes. For most small prolactinomas, dopamine agonists bring prolactin levels back to normal and shrink tumors in 4 out of 5 patients.5 Side effects. Common side effects of the drugs include nausea, vomiting, and dizziness. Both medicines should always be taken with food. Starting treatment at a low dose and taking the medicine at bedtime can reduce side effects. Complications. Although dopamine agonists have been linked to heart valve damage, these problems were found mainly among people taking these medicines to treat Parkinson’s disease . These patients typically take much higher doses (usually about 10 times higher) of these medicines than are used to treat prolactinomas. If you need to take a high dose of a dopamine agonist, your doctor may order an echocardiogram (echo) to check your heart valves and heart function. Rarely, psychiatric disorders related to impulse control, such as compulsive gambling , have been seen in people taking these medicines.6 Duration of treatment. You may have to take these medicines for a long time to prevent the tumor from growing back, especially if the prolactinoma is large. After 2 years, the medicines may be slowly reduced and stopped if prolactin levels are normal and the tumor is no longer visible.1 But if your prolactin level goes back up again, you may need to go back on the medicine for as long as needed to bring your prolactin level under control.
Surgery
Although doctors most often treat prolactinomas with medicines, in some cases surgery may be an option. Examples include
- you can’t tolerate the medicines
- the medicines aren’t working for you
- you take antipsychotic medicines that interact with the medicines used to treat prolactinomas
- In some cases, when a prolactinoma is large, a woman may choose to have surgery to remove the tumor before trying to become pregnant.
Two types of surgery may be used Transsphenoidal surgery is most commonly used to treat prolactinoma. The surgery is done through an incision, or cut, at the back of the nasal cavity or under the upper lip. Transcranial surgery is used more rarely if the tumor is large or has spread to other areas. The surgeon removes the tumor through an opening in the skull. More rarely, if medicines and surgery fail to reduce prolactin levels, radiation therapy may be used. This type of treatment uses high-energy x-rays or particle waves to kill tumor cells. Depending on the size and location of the tumor, the total radiation dose is delivered in one session, or in lower doses over the course of 4 to 6 weeks. Outcomes. Prolactin levels return to normal in 1 out of 3 patients treated with radiation therapy.1 However, as radiation treatment lowers prolactin levels over time, it may take years to reach this outcome. Your doctor is likely to prescribe medicines while you wait to see results. Side effects and complications. The most common side effect is low levels of thyroid hormone. In up to half of patients, radiation therapy may also lead to a decrease in other pituitary hormones.8 Vision loss and brain injury are rare complications. Rarely, other types of tumors can develop many years later in areas that were in the path of the radiation beam. When pregnancy is confirmed. Although studies suggest that both bromocriptine and [[cabergoline[[ can be safely taken in the early stages of pregnancy, bromocriptine is typically preferred because of its longer safety record. As soon as your pregnancy is confirmed, your doctor will usually advise you to stop taking these medicines to prevent any possible effects on the fetus. During pregnancy. Prolactin levels normally increase during pregnancy, preparing your breasts to make milk after your baby is born. The pituitary gland often doubles in size during pregnancy. Your prolactinoma may also grow in size, especially if it is already large. If you begin to have symptoms such as headaches and changes in vision, your doctor may recommend that you start taking the medicine again. After delivery. After delivery, women with small prolactinomas can usually nurse their babies. If your prolactinoma is large, your doctor may suggest that you consult with an endocrinologist about breastfeeding. Doctors don’t usually measure prolactin levels during pregnancy and breastfeeding. Your doctor will usually begin to do so again a couple of months after you stop nursing. In some cases, prolactin levels remain normal after delivery and nursing.
| Glandular and epithelial cancer | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| Tumours of endocrine glands | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
NIH genetic and rare disease info
Prolactinoma is a rare disease.
| Rare and genetic diseases | ||||||
|---|---|---|---|---|---|---|
|
Rare diseases - Prolactinoma
|


