Adenoma
| Adenoma | |
|---|---|
| |
| Synonyms | |
| Pronounce | N/A |
| Specialty | N/A |
| Symptoms | Often asymptomatic, may cause hormonal imbalance if functional |
| Complications | Potential progression to adenocarcinoma |
| Onset | Varies depending on type and location |
| Duration | Indeterminate, may remain stable or progress |
| Types | Tubular adenoma, villous adenoma, tubulovillous adenoma |
| Causes | Genetic mutations, environmental factors |
| Risks | Age, family history, diet, smoking |
| Diagnosis | Biopsy, endoscopy, imaging studies |
| Differential diagnosis | Hyperplasia, adenocarcinoma, polyp |
| Prevention | Regular screening, healthy diet, avoiding smoking |
| Treatment | Surgical removal, endoscopic resection |
| Medication | None specific, may use hormonal therapy if functional |
| Prognosis | Generally good if benign, risk of malignancy varies |
| Frequency | Common, varies by type and location |
| Deaths | Rare, unless progresses to malignancy |
Benign glandular tumors with potential malignant transformation
| Adenoma | |
|---|---|

| |
| Synonyms | Adenomatous tumor |
| Pronounce | |
| Field | Oncology, Pathology, Endocrinology, Gastroenterology |
| Symptoms | Often asymptomatic; may cause hormonal imbalance, obstruction, pain |
| Complications | Malignant transformation, bleeding, organ dysfunction |
| Onset | Variable; often detected in adults |
| Duration | Chronic (often lifelong surveillance required) |
| Types | Colorectal, pituitary, thyroid, adrenal, hepatic, renal, sebaceous |
| Causes | Genetic mutations, hormonal imbalance, environmental factors |
| Risks | Age, genetics, obesity, hormonal therapy, radiation exposure |
| Diagnosis | Clinical evaluation, imaging, laboratory tests, biopsy |
| Differential diagnosis | Hyperplastic polyps, adenocarcinoma, neuroendocrine tumors |
| Prevention | Lifestyle modifications, genetic screening |
| Treatment | Surveillance, endoscopic removal, surgical excision, medical therapy |
| Medication | Hormone suppressants, antithyroid medications, dopamine agonists |
| Prognosis | Generally good; dependent on type, size, and malignant risk |
| Frequency | Common (colorectal adenomas); other types vary |
| Deaths | Rare, usually due to malignant transformation or complications |
Adenoma is a type of benign tumor originating from glandular epithelial cells. Although adenomas themselves are benign, some possess the potential to progress into malignant tumors (adenocarcinoma). They commonly affect various glandular organs, including the colon, pituitary gland, thyroid gland, adrenal gland, liver, and kidney. Understanding their characteristics, potential complications, and management strategies is vital for early detection and treatment.
Definition and Characteristics[edit]
An adenoma arises from glandular epithelial tissue, forming a well-defined, localized mass. Despite their benign nature, adenomas can cause complications by:
- Compressing nearby structures (mass effect)
- Producing excess hormones (functional adenomas)
- Potentially transforming into malignant adenocarcinoma (notably colorectal adenomas)
Epidemiology[edit]
The frequency and clinical significance of adenomas vary by organ:
- Colorectal adenomas: Common in adults >50 years; precursors to colorectal cancer.
- Pituitary adenomas: Account for 10–15% of intracranial tumors.
- Thyroid adenomas: Frequent in women; detected as thyroid nodules.
- Hepatic adenomas: Rare; linked to oral contraceptive use.
Clinical Significance[edit]
Adenomas can significantly impact health due to:
- Hormonal imbalance: Functional adenomas can cause endocrine disorders (e.g., Cushing’s syndrome, hyperthyroidism).
- Obstruction: Large adenomas in the colon may cause bowel obstruction.
- Malignant potential: Particularly colorectal adenomas that can transform into colorectal cancer.
- Early identification and management are essential to reduce morbidity.
Types of Adenomas[edit]
Adenomas vary by anatomical location and behavior:
Colorectal Adenomas[edit]

Common precursors to colorectal cancer; subtypes include:
Pituitary Adenomas[edit]
Arise in the pituitary gland; subtypes include:
- Prolactinoma
- Growth hormone-secreting adenoma
- ACTH-secreting adenoma
- Non-functioning adenomas
Thyroid Adenomas[edit]

Often solitary nodules arising from follicular cells; subtypes include:
Adrenal Adenomas[edit]

Occur in adrenal cortex; may produce hormones (e.g., cortisol or aldosterone):
- Functioning adenomas (Cushing’s syndrome, Conn’s syndrome)
Hepatic Adenomas[edit]
Benign liver tumors associated with oral contraceptive use; risk of hemorrhage or malignant transformation.
Renal Adenomas[edit]
Small benign kidney tumors; usually incidental findings.
Sebaceous Adenomas[edit]
Associated with sebaceous glands; linked to Muir-Torre syndrome.
Causes and Risk Factors[edit]

Adenomas develop due to genetic mutations, hormonal disturbances, and environmental factors:
- Genetic conditions (e.g., Familial adenomatous polyposis, Multiple endocrine neoplasia)
- Hormonal imbalances (pituitary, thyroid, adrenal adenomas)
- Diet and obesity (colorectal adenomas)
- Oral contraceptives (hepatic adenomas)
- Radiation exposure (thyroid adenomas)
Symptoms and Complications[edit]
Symptoms depend on adenoma location and hormone secretion:
- Colorectal adenomas: Rectal bleeding, bowel habit changes
- Pituitary adenomas: Vision changes, hormonal imbalance
- Thyroid adenomas: Hyperthyroidism, neck lump
- Adrenal adenomas: Cushing’s or Conn’s syndrome
- Hepatic adenomas: Abdominal pain, risk of bleeding
- Renal adenomas: Usually asymptomatic
Complications include malignant transformation, organ obstruction, hormonal disturbances, and bleeding.
Diagnosis[edit]

Diagnosis involves:
- Clinical evaluation: History, physical exam
- Imaging: Colonoscopy, ultrasound, MRI, CT
- Laboratory tests: Hormone levels, tumor markers
- Histopathology: Biopsy confirms diagnosis
Treatment and Management[edit]
Treatment varies by adenoma type and risk factors:
- Observation: Small, asymptomatic adenomas
- Endoscopic removal: Colorectal polyps
- Surgical excision: Large or high-risk adenomas
- Medical therapy: Hormone-suppressing medications for pituitary and adrenal adenomas
Long-term monitoring is often required due to recurrence risk.
Prognosis[edit]
Prognosis depends on adenoma type and malignant potential:
- Generally favorable with early detection and treatment
- High-risk adenomas require ongoing surveillance to prevent cancer progression
Prevention[edit]
Preventive strategies include lifestyle modifications, regular screenings (colonoscopy), genetic counseling, and hormonal regulation.
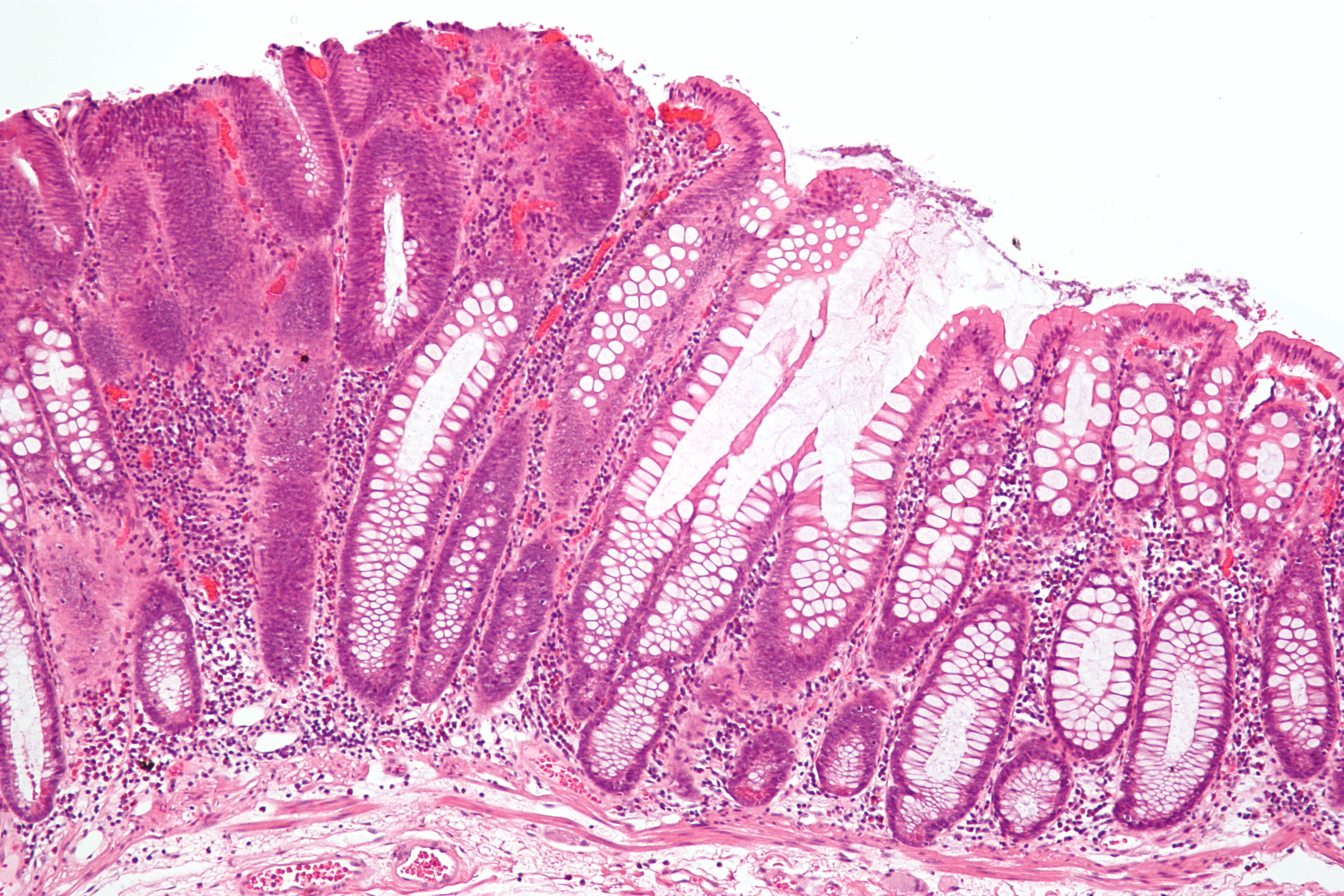
Gallery[edit]
-
Traditional serrated adenoma histopathology
-
Adenoma-carcinoma progression diagram
See also[edit]
External links[edit]
American Cancer Society – Adenomas Genetic and Rare Diseases Information Center (GARD)
| Overview of tumors, cancer and oncology | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| Endocrine disorders | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
This endocrine disorder-related article is a stub.
|
Ad. Transform your life with W8MD's Budget GLP-1 injections from $49.99


W8MD offers a medical weight loss program to lose weight in Philadelphia. Our physician-supervised medical weight loss provides:
- Weight loss injections in NYC (generic and brand names):
- Zepbound / Mounjaro, Wegovy / Ozempic, Saxenda
- Most insurances accepted or discounted self-pay rates. We will obtain insurance prior authorizations if needed.
- Generic GLP1 weight loss injections from $49.99 for the starting dose of Semaglutide and $65.00 for Tirzepatide.
- Also offer prescription weight loss medications including Phentermine, Qsymia, Diethylpropion, Contrave etc.
NYC weight loss doctor appointmentsNYC weight loss doctor appointments
Start your NYC weight loss journey today at our NYC medical weight loss and Philadelphia medical weight loss clinics.
- Call 718-946-5500 to lose weight in NYC or for medical weight loss in Philadelphia 215-676-2334.
- Tags:NYC medical weight loss, Philadelphia lose weight Zepbound NYC, Budget GLP1 weight loss injections, Wegovy Philadelphia, Wegovy NYC, Philadelphia medical weight loss, Brookly weight loss and Wegovy NYC
|
WikiMD's Wellness Encyclopedia |
| Let Food Be Thy Medicine Medicine Thy Food - Hippocrates |
Medical Disclaimer: WikiMD is not a substitute for professional medical advice. The information on WikiMD is provided as an information resource only, may be incorrect, outdated or misleading, and is not to be used or relied on for any diagnostic or treatment purposes. Please consult your health care provider before making any healthcare decisions or for guidance about a specific medical condition. WikiMD expressly disclaims responsibility, and shall have no liability, for any damages, loss, injury, or liability whatsoever suffered as a result of your reliance on the information contained in this site. By visiting this site you agree to the foregoing terms and conditions, which may from time to time be changed or supplemented by WikiMD. If you do not agree to the foregoing terms and conditions, you should not enter or use this site. See full disclaimer.
Credits:Most images are courtesy of Wikimedia commons, and templates, categories Wikipedia, licensed under CC BY SA or similar.
Translate this page: - East Asian
中文,
日本,
한국어,
South Asian
हिन्दी,
தமிழ்,
తెలుగు,
Urdu,
ಕನ್ನಡ,
Southeast Asian
Indonesian,
Vietnamese,
Thai,
မြန်မာဘာသာ,
বাংলা
European
español,
Deutsch,
français,
Greek,
português do Brasil,
polski,
română,
русский,
Nederlands,
norsk,
svenska,
suomi,
Italian
Middle Eastern & African
عربى,
Turkish,
Persian,
Hebrew,
Afrikaans,
isiZulu,
Kiswahili,
Other
Bulgarian,
Hungarian,
Czech,
Swedish,
മലയാളം,
मराठी,
ਪੰਜਾਬੀ,
ગુજરાતી,
Portuguese,
Ukrainian



