Eosinophilic granulomatosis with polyangiitis: Difference between revisions
mNo edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
{{Infobox medical condition (new) | {{Infobox medical condition (new) | ||
| name | | name = Eosinophilic Granulomatosis with Polyangiitis (EGPA) | ||
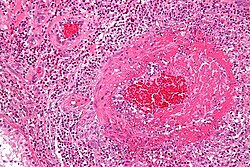
| image | | image = Churg-Strauss syndrome - high mag.jpg | ||
| caption | | caption = [[Micrograph]] showing eosinophilic [[vasculitis]] consistent with eosinophilic granulomatosis with polyangiitis. [[H&E stain]]. | ||
| pronounce = | |||
| pronounce | | field = [[Rheumatology]], [[Immunology]] | ||
| field | | synonyms = '''Churg–Strauss Syndrome''', '''Allergic Angiitis and Granulomatosis''' | ||
| synonyms | | symptoms = Fatigue, fever, weight loss, night sweats, [[asthma]], [[arthralgia]], [[myalgia]], [[purpura]], [[urticaria]], skin nodules, cough, nasal polyps, [[sinusitis]], [[neuropathy]], gastrointestinal distress. | ||
| symptoms | | complications = [[Hypereosinophilia]], [[vasculitis]], [[cardiac disease]], [[neuropathy]], [[renal failure]], [[pulmonary involvement]]. | ||
| complications | | onset = Gradual, typically in adulthood, often in individuals with a history of asthma or allergic conditions. | ||
| onset | | duration = Chronic with periods of remission and flare-ups. | ||
| duration | | types = Systemic necrotizing [[vasculitis]] affecting small-to-medium blood vessels. | ||
| types | | causes = Autoimmune response; associated with [[antineutrophil cytoplasmic antibodies]] (ANCA). | ||
| causes | | risks = History of [[asthma]], [[allergic rhinitis]], [[eosinophilia]], exposure to allergens or environmental triggers. | ||
| risks | | diagnosis = Blood tests for eosinophilia and ANCA, imaging studies, tissue biopsy, clinical criteria (American College of Rheumatology). | ||
| | | differential = [[Granulomatosis with polyangiitis]], [[hypereosinophilic syndrome]], [[microscopic polyangiitis]], [[sarcoidosis]], [[asthma]]. | ||
| | | prevention = No known prevention; early treatment can help manage disease progression. | ||
| treatment = [[Immunosuppression]] with corticosteroids and immunomodulatory drugs. | |||
| treatment | | medication = [[Corticosteroids]] (e.g., [[prednisone]]), [[mepolizumab]], [[cyclophosphamide]], [[azathioprine]], [[methotrexate]]. | ||
| medication | | prognosis = Variable; some achieve remission, while others develop progressive complications. | ||
| prognosis | | frequency = Rare; estimated prevalence of 10–15 cases per million. | ||
| frequency | | deaths = Can be fatal if untreated, particularly due to cardiac or pulmonary complications. | ||
| deaths | |||
}} | }} | ||
[[ | '''Eosinophilic Granulomatosis with Polyangiitis''' (EGPA), formerly known as '''Churg–Strauss Syndrome''', is a rare [[autoimmune disease]] characterized by [[vasculitis]] affecting small and medium-sized blood vessels. It primarily occurs in individuals with a history of [[asthma]] or other allergic conditions, and is distinguished by elevated levels of [[eosinophils]] in the blood and tissues, leading to widespread inflammation. | ||
== Pathophysiology == | |||
EGPA is considered an [[antineutrophil cytoplasmic antibody]] (ANCA)-associated [[vasculitis]], though not all cases are ANCA-positive. The disease progresses in three overlapping stages: | |||
* Allergic stage: Characterized by long-standing or newly developed [[asthma]], [[allergic rhinitis]], and [[nasal polyps]]. | |||
* Eosinophilic stage: Marked by high levels of [[eosinophilia]] (greater than 10% of total white blood cells), leading to [[pulmonary infiltrates]], [[gastrointestinal damage]], and [[cardiac involvement]]. | |||
* Vasculitic stage: The most severe phase, where systemic [[vasculitis]] affects multiple organs, causing [[neuropathy]], [[glomerulonephritis]], [[myocarditis]], and [[skin lesions]]. | |||
== Signs and Symptoms == | |||
EGPA manifests with a wide range of symptoms, which vary depending on the stage and organ involvement. Common symptoms include: | |||
* Respiratory symptoms: Severe [[asthma]], sinusitis, nasal polyps, chronic cough, lung infiltrates. | |||
* Skin manifestations: [[Purpura]], [[urticaria]], nodules, [[livedo reticularis]], or necrotic lesions. | |||
* Neurological involvement: Peripheral [[neuropathy]] such as [[mononeuritis multiplex]], characterized by muscle weakness, numbness, and pain. | |||
* Gastrointestinal issues: Abdominal pain, diarrhea, gastrointestinal bleeding, eosinophilic colitis. | |||
* Cardiovascular complications: [[Myocarditis]], pericarditis, arrhythmias, [[heart failure]]. | |||
* Renal involvement: Rare but can include [[glomerulonephritis]]. | |||
* General symptoms: Weight loss, fever, fatigue, night sweats, joint and muscle pain. | |||
== Diagnosis == | == Diagnosis == | ||
EGPA is diagnosed based on a combination of clinical symptoms, laboratory findings, and histopathological examination. Diagnostic criteria include: | |||
* | * Blood tests: | ||
* | * Elevated eosinophil count (>1,500/microliter). | ||
*Presence of [[ | * Presence of ANCA antibodies (positive in ~40% of cases). | ||
* | * Elevated [[C-reactive protein]] (CRP) and [[erythrocyte sedimentation rate]] (ESR). | ||
* Increased [[IgE]] levels. | |||
*[[ | * Imaging: | ||
* Chest X-ray or CT scan showing lung infiltrates or nodules. | |||
* MRI or nerve conduction studies to assess neuropathy. | |||
* [[Biopsy]]: | |||
* Tissue biopsy from affected organs (e.g., skin, lung, nerve) demonstrating vasculitis, eosinophilic infiltration, and granuloma formation. | |||
* American College of Rheumatology (ACR) Classification Criteria: | |||
* | * Asthma. | ||
* | * Eosinophilia (>10% of total white blood cells). | ||
* | * Neuropathy (mono- or polyneuropathy). | ||
* | * Pulmonary infiltrates. | ||
* | * Sinus abnormalities. | ||
* Extravascular eosinophil accumulation on biopsy. | |||
* A patient is classified as having EGPA if four or more of these criteria are met. | |||
== Treatment == | == Treatment == | ||
Management of EGPA depends on the severity of organ involvement. The primary goal is to reduce inflammation and prevent long-term damage. | |||
===First-Line Treatment=== | |||
* [[Corticosteroids]] ([[Prednisone]], [[Methylprednisolone]]): | |||
* High-dose corticosteroids are the cornerstone of treatment, particularly during acute exacerbations. | |||
* Gradual tapering is required to avoid flare-ups. | |||
===Immunosuppressive Therapy=== | |||
* Used in cases with severe organ involvement or steroid-refractory disease. | |||
* [[Cyclophosphamide]]: Indicated for life-threatening manifestations (cardiac, neurological, or renal involvement). | |||
* Azathioprine or Methotrexate: Used as steroid-sparing agents for long-term maintenance. | |||
== | ===Biologic Therapy=== | ||
* [[Mepolizumab]] (IL-5 inhibitor): Approved for EGPA, particularly for cases with eosinophilia and asthma. | |||
* [[Rituximab]] (B-cell inhibitor): Sometimes used in ANCA-positive EGPA. | |||
== | ===Supportive Treatment=== | ||
* Bronchodilators and inhaled steroids for asthma symptoms. | |||
* Anticoagulation if vasculitis leads to blood clotting complications. | |||
* Pain management for neuropathy-related symptoms. | |||
== Prognosis == | |||
The prognosis of EGPA varies based on disease severity and response to treatment: | |||
* Mild cases (limited to asthma and skin involvement) often have a good prognosis with corticosteroids alone. | |||
* Severe cases (cardiac, renal, or neurological complications) require aggressive treatment. | |||
* Relapses are common, and lifelong monitoring is necessary. | |||
Without treatment, EGPA can lead to life-threatening complications, particularly from cardiac and pulmonary involvement. With appropriate immunosuppressive therapy, the 5-year survival rate exceeds 80%. | |||
== Epidemiology == | |||
EGPA is rare, with an estimated incidence of 1–3 cases per million per year. It primarily affects adults between ages 30 and 50, with no significant gender predominance. It is more common in individuals with long-standing asthma or allergic rhinitis. | |||
== History == | |||
The condition was first described in 1951 by Jacob Churg and Lotte Strauss, who identified the combination of asthma, eosinophilia, and vasculitis. The name was changed from Churg–Strauss Syndrome to Eosinophilic Granulomatosis with Polyangiitis (EGPA) in 2012 to align with standardized nomenclature for vasculitides. | |||
== Notable Cases == | |||
* Ben Watt, musician and author, chronicled his experience with EGPA in his memoir ''Patient''. | |||
* Umaru Musa Yar'Adua, former President of Nigeria, reportedly had EGPA. | |||
* Charlie Gillett, renowned DJ and music historian, passed away due to EGPA complications. | |||
* Toni Street, New Zealand broadcaster, publicly shared her battle with EGPA. | |||
== | == See Also == | ||
* [[Vasculitis]] | |||
* [[Eosinophilia]] | |||
* [[Asthma]] | |||
* [[Antineutrophil cytoplasmic antibody]] | |||
* | |||
* | |||
* | |||
{{Systemic vasculitis}} | {{Systemic vasculitis}} | ||
{{Autoimmune diseases}} | |||
{{ | {{stub}} | ||
[[Category:Autoimmune diseases]] | [[Category:Autoimmune diseases]] | ||
[[Category:Eosinophilic | [[Category:Eosinophilic conditions]] | ||
[[Category:Lung disorders]] | [[Category:Lung disorders]] | ||
[[Category:Steroid-responsive inflammatory conditions]] | [[Category:Steroid-responsive inflammatory conditions]] | ||
[[Category: | [[Category:Rare diseases]] | ||
Latest revision as of 18:50, 19 March 2025
| Eosinophilic Granulomatosis with Polyangiitis (EGPA) | |
|---|---|
| |
| Synonyms | Churg–Strauss Syndrome, Allergic Angiitis and Granulomatosis |
| Pronounce | |
| Field | Rheumatology, Immunology |
| Symptoms | Fatigue, fever, weight loss, night sweats, asthma, arthralgia, myalgia, purpura, urticaria, skin nodules, cough, nasal polyps, sinusitis, neuropathy, gastrointestinal distress. |
| Complications | Hypereosinophilia, vasculitis, cardiac disease, neuropathy, renal failure, pulmonary involvement. |
| Onset | Gradual, typically in adulthood, often in individuals with a history of asthma or allergic conditions. |
| Duration | Chronic with periods of remission and flare-ups. |
| Types | Systemic necrotizing vasculitis affecting small-to-medium blood vessels. |
| Causes | Autoimmune response; associated with antineutrophil cytoplasmic antibodies (ANCA). |
| Risks | History of asthma, allergic rhinitis, eosinophilia, exposure to allergens or environmental triggers. |
| Diagnosis | Blood tests for eosinophilia and ANCA, imaging studies, tissue biopsy, clinical criteria (American College of Rheumatology). |
| Differential diagnosis | Granulomatosis with polyangiitis, hypereosinophilic syndrome, microscopic polyangiitis, sarcoidosis, asthma. |
| Prevention | No known prevention; early treatment can help manage disease progression. |
| Treatment | Immunosuppression with corticosteroids and immunomodulatory drugs. |
| Medication | Corticosteroids (e.g., prednisone), mepolizumab, cyclophosphamide, azathioprine, methotrexate. |
| Prognosis | Variable; some achieve remission, while others develop progressive complications. |
| Frequency | Rare; estimated prevalence of 10–15 cases per million. |
| Deaths | Can be fatal if untreated, particularly due to cardiac or pulmonary complications. |
Eosinophilic Granulomatosis with Polyangiitis (EGPA), formerly known as Churg–Strauss Syndrome, is a rare autoimmune disease characterized by vasculitis affecting small and medium-sized blood vessels. It primarily occurs in individuals with a history of asthma or other allergic conditions, and is distinguished by elevated levels of eosinophils in the blood and tissues, leading to widespread inflammation.
Pathophysiology[edit]
EGPA is considered an antineutrophil cytoplasmic antibody (ANCA)-associated vasculitis, though not all cases are ANCA-positive. The disease progresses in three overlapping stages:
- Allergic stage: Characterized by long-standing or newly developed asthma, allergic rhinitis, and nasal polyps.
- Eosinophilic stage: Marked by high levels of eosinophilia (greater than 10% of total white blood cells), leading to pulmonary infiltrates, gastrointestinal damage, and cardiac involvement.
- Vasculitic stage: The most severe phase, where systemic vasculitis affects multiple organs, causing neuropathy, glomerulonephritis, myocarditis, and skin lesions.
Signs and Symptoms[edit]
EGPA manifests with a wide range of symptoms, which vary depending on the stage and organ involvement. Common symptoms include:
- Respiratory symptoms: Severe asthma, sinusitis, nasal polyps, chronic cough, lung infiltrates.
- Skin manifestations: Purpura, urticaria, nodules, livedo reticularis, or necrotic lesions.
- Neurological involvement: Peripheral neuropathy such as mononeuritis multiplex, characterized by muscle weakness, numbness, and pain.
- Gastrointestinal issues: Abdominal pain, diarrhea, gastrointestinal bleeding, eosinophilic colitis.
- Cardiovascular complications: Myocarditis, pericarditis, arrhythmias, heart failure.
- Renal involvement: Rare but can include glomerulonephritis.
- General symptoms: Weight loss, fever, fatigue, night sweats, joint and muscle pain.
Diagnosis[edit]
EGPA is diagnosed based on a combination of clinical symptoms, laboratory findings, and histopathological examination. Diagnostic criteria include:
- Blood tests:
- Elevated eosinophil count (>1,500/microliter).
- Presence of ANCA antibodies (positive in ~40% of cases).
- Elevated C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR).
- Increased IgE levels.
- Imaging:
- Chest X-ray or CT scan showing lung infiltrates or nodules.
- MRI or nerve conduction studies to assess neuropathy.
- Biopsy:
- Tissue biopsy from affected organs (e.g., skin, lung, nerve) demonstrating vasculitis, eosinophilic infiltration, and granuloma formation.
- American College of Rheumatology (ACR) Classification Criteria:
- Asthma.
- Eosinophilia (>10% of total white blood cells).
- Neuropathy (mono- or polyneuropathy).
- Pulmonary infiltrates.
- Sinus abnormalities.
- Extravascular eosinophil accumulation on biopsy.
- A patient is classified as having EGPA if four or more of these criteria are met.
Treatment[edit]
Management of EGPA depends on the severity of organ involvement. The primary goal is to reduce inflammation and prevent long-term damage.
First-Line Treatment[edit]
- Corticosteroids (Prednisone, Methylprednisolone):
- High-dose corticosteroids are the cornerstone of treatment, particularly during acute exacerbations.
- Gradual tapering is required to avoid flare-ups.
Immunosuppressive Therapy[edit]
- Used in cases with severe organ involvement or steroid-refractory disease.
- Cyclophosphamide: Indicated for life-threatening manifestations (cardiac, neurological, or renal involvement).
- Azathioprine or Methotrexate: Used as steroid-sparing agents for long-term maintenance.
Biologic Therapy[edit]
- Mepolizumab (IL-5 inhibitor): Approved for EGPA, particularly for cases with eosinophilia and asthma.
- Rituximab (B-cell inhibitor): Sometimes used in ANCA-positive EGPA.
Supportive Treatment[edit]
- Bronchodilators and inhaled steroids for asthma symptoms.
- Anticoagulation if vasculitis leads to blood clotting complications.
- Pain management for neuropathy-related symptoms.
Prognosis[edit]
The prognosis of EGPA varies based on disease severity and response to treatment:
- Mild cases (limited to asthma and skin involvement) often have a good prognosis with corticosteroids alone.
- Severe cases (cardiac, renal, or neurological complications) require aggressive treatment.
- Relapses are common, and lifelong monitoring is necessary.
Without treatment, EGPA can lead to life-threatening complications, particularly from cardiac and pulmonary involvement. With appropriate immunosuppressive therapy, the 5-year survival rate exceeds 80%.
Epidemiology[edit]
EGPA is rare, with an estimated incidence of 1–3 cases per million per year. It primarily affects adults between ages 30 and 50, with no significant gender predominance. It is more common in individuals with long-standing asthma or allergic rhinitis.
History[edit]
The condition was first described in 1951 by Jacob Churg and Lotte Strauss, who identified the combination of asthma, eosinophilia, and vasculitis. The name was changed from Churg–Strauss Syndrome to Eosinophilic Granulomatosis with Polyangiitis (EGPA) in 2012 to align with standardized nomenclature for vasculitides.
Notable Cases[edit]
- Ben Watt, musician and author, chronicled his experience with EGPA in his memoir Patient.
- Umaru Musa Yar'Adua, former President of Nigeria, reportedly had EGPA.
- Charlie Gillett, renowned DJ and music historian, passed away due to EGPA complications.
- Toni Street, New Zealand broadcaster, publicly shared her battle with EGPA.
See Also[edit]
| Systemic vasculitis | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| Hypersensitivity and autoimmune diseases (279.5–6) | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|


