Autoimmune polyendocrine syndrome type 2

Editor-In-Chief: Prab R Tumpati, MD
Obesity, Sleep & Internal medicine
Founder, WikiMD Wellnesspedia &
W8MD's medical weight loss NYC, sleep center NYC
Philadelphia medical weight loss and Philadelphia sleep clinics
| Autoimmune polyendocrine syndrome type 2 | |
|---|---|
| |
| Synonyms | Schmidt syndrome |
| Pronounce | N/A |
| Specialty | N/A |
| Symptoms | Adrenal insufficiency, hypothyroidism, type 1 diabetes |
| Complications | Addisonian crisis, myxedema coma, diabetic ketoacidosis |
| Onset | Typically in adulthood |
| Duration | Chronic |
| Types | N/A |
| Causes | Autoimmune disease |
| Risks | Genetic predisposition, HLA-DR3, HLA-DR4 |
| Diagnosis | Clinical evaluation, blood tests for hormone levels, autoantibody testing |
| Differential diagnosis | Autoimmune polyendocrine syndrome type 1, isolated autoimmune conditions |
| Prevention | N/A |
| Treatment | Hormone replacement therapy, immunosuppressive drugs |
| Medication | Hydrocortisone, levothyroxine, insulin |
| Prognosis | Variable, depends on management of individual conditions |
| Frequency | Rare |
| Deaths | N/A |
Autoimmune Polyendocrine Syndrome Type 2 (APS-2), also known as Schmidt's syndrome, is a complex autoimmune disorder characterized by the coexistence of at least two autoimmune diseases, including Addison's disease, thyroid autoimmune diseases (such as Graves' disease or Hashimoto's thyroiditis), and type 1 diabetes mellitus. This syndrome is more common in females and typically presents in adulthood.
Etiology and Pathogenesis[edit]
The exact cause of APS-2 is unknown, but it is believed to involve a combination of genetic predisposition and environmental factors. The HLA-DQ gene is often associated with the syndrome, suggesting a strong genetic component. Environmental triggers may include viral infections, stress, and other unknown factors that initiate an autoimmune response in genetically susceptible individuals.
Clinical Manifestations[edit]
APS-2 presents with a variety of symptoms depending on the specific autoimmune diseases involved. Common manifestations include:
- Addison's disease symptoms: fatigue, weight loss, skin hyperpigmentation, low blood pressure, and salt craving.
- Thyroid autoimmune diseases symptoms: depending on whether the patient has Graves' disease (hyperthyroidism) or Hashimoto's thyroiditis (hypothyroidism), symptoms can include weight changes, mood swings, heat or cold intolerance, and changes in heart rate.
- Type 1 diabetes mellitus symptoms: increased thirst and urination, weight loss, fatigue, and blurred vision.
Diagnosis[edit]
Diagnosis of APS-2 involves a combination of clinical evaluation and laboratory tests. Key diagnostic tests include:
- Autoantibody tests: to detect antibodies against the adrenal cortex, thyroid, and pancreatic islet cells.
- Hormone level tests: to assess the function of the affected glands (e.g., cortisol, thyroid hormones, and insulin).
- Imaging studies: such as ultrasound or CT scans, may be used to evaluate the structure of the thyroid gland and adrenal glands.
Treatment[edit]
Treatment of APS-2 focuses on managing the symptoms of the individual autoimmune diseases involved and may require a multidisciplinary approach. Common treatments include:
- Corticosteroids: for Addison's disease to replace the deficient hormones.
- Thyroid hormone replacement therapy: for Hashimoto's thyroiditis.
- Antithyroid drugs or radioactive iodine therapy: for Graves' disease.
- Insulin therapy: for type 1 diabetes mellitus.
Regular monitoring and adjustments of therapy are essential due to the progressive nature of these autoimmune diseases.
Prognosis[edit]
With appropriate treatment and monitoring, individuals with APS-2 can manage their symptoms and maintain a relatively normal quality of life. However, they must remain vigilant for the development of additional autoimmune diseases.
Epidemiology[edit]
APS-2 is less common than Autoimmune Polyendocrine Syndrome Type 1 (APS-1) but is more prevalent in certain populations, particularly those of Northern European descent. It typically presents in adulthood, with a higher incidence in females.
Autoimmune polyendocrine syndrome type 2[edit]
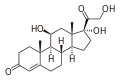
-
Hashimoto thyroiditis
-
Autoimmune polyendocrine syndrome type 2
-
Cortisol
See Also[edit]
Ad. Transform your life with W8MD's Budget GLP-1 injections from $49.99


W8MD offers a medical weight loss program to lose weight in Philadelphia. Our physician-supervised medical weight loss provides:
- Weight loss injections in NYC (generic and brand names):
- Zepbound / Mounjaro, Wegovy / Ozempic, Saxenda
- Most insurances accepted or discounted self-pay rates. We will obtain insurance prior authorizations if needed.
- Generic GLP1 weight loss injections from $49.99 for the starting dose of Semaglutide and $65.00 for Tirzepatide.
- Also offer prescription weight loss medications including Phentermine, Qsymia, Diethylpropion, Contrave etc.
NYC weight loss doctor appointmentsNYC weight loss doctor appointments
Start your NYC weight loss journey today at our NYC medical weight loss and Philadelphia medical weight loss clinics.
- Call 718-946-5500 to lose weight in NYC or for medical weight loss in Philadelphia 215-676-2334.
- Tags:NYC medical weight loss, Philadelphia lose weight Zepbound NYC, Budget GLP1 weight loss injections, Wegovy Philadelphia, Wegovy NYC, Philadelphia medical weight loss, Brookly weight loss and Wegovy NYC
|
WikiMD's Wellness Encyclopedia |
| Let Food Be Thy Medicine Medicine Thy Food - Hippocrates |
Medical Disclaimer: WikiMD is not a substitute for professional medical advice. The information on WikiMD is provided as an information resource only, may be incorrect, outdated or misleading, and is not to be used or relied on for any diagnostic or treatment purposes. Please consult your health care provider before making any healthcare decisions or for guidance about a specific medical condition. WikiMD expressly disclaims responsibility, and shall have no liability, for any damages, loss, injury, or liability whatsoever suffered as a result of your reliance on the information contained in this site. By visiting this site you agree to the foregoing terms and conditions, which may from time to time be changed or supplemented by WikiMD. If you do not agree to the foregoing terms and conditions, you should not enter or use this site. See full disclaimer.
Credits:Most images are courtesy of Wikimedia commons, and templates, categories Wikipedia, licensed under CC BY SA or similar.
Translate this page: - East Asian
中文,
日本,
한국어,
South Asian
हिन्दी,
தமிழ்,
తెలుగు,
Urdu,
ಕನ್ನಡ,
Southeast Asian
Indonesian,
Vietnamese,
Thai,
မြန်မာဘာသာ,
বাংলা
European
español,
Deutsch,
français,
Greek,
português do Brasil,
polski,
română,
русский,
Nederlands,
norsk,
svenska,
suomi,
Italian
Middle Eastern & African
عربى,
Turkish,
Persian,
Hebrew,
Afrikaans,
isiZulu,
Kiswahili,
Other
Bulgarian,
Hungarian,
Czech,
Swedish,
മലയാളം,
मराठी,
ਪੰਜਾਬੀ,
ગુજરાતી,
Portuguese,
Ukrainian