Adiposis dolorosa: Difference between revisions
No edit summary |
CSV import |
||
| Line 115: | Line 115: | ||
{{Soft tissue tumors and sarcomas}} | {{Soft tissue tumors and sarcomas}} | ||
[[Category:Rare diseases]] | [[Category:Rare diseases]] | ||
<gallery> | |||
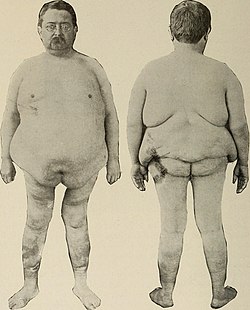
File:Nervous and mental diseases (1919) (14781727145).jpg|Adiposis dolorosa | |||
</gallery> | |||
Revision as of 01:13, 20 February 2025
Adiposis dolorosa, also known as Dercum's disease<ref>Dercum's disease or syndrome at Who Named It?</ref> or Anders disease, is a rare condition characterized by generalized obesity and fatty tumors in the adipose tissue. The tumors are normally painful and found in multiples on the extremities.<ref name=":1">
Learning About Dercum Disease(link). www.genome.gov.
</ref> The cause and mechanism of Dercum's disease remains unknown.<ref name="genome">
Learning About Dercum Disease(link). {{{website}}}. National Human Genome Research Institute. 2012-06-27.
</ref> Possible causes include nervous system dysfunction, mechanical pressure on nerves, adipose tissue dysfunction and trauma.<ref name="ojrd.com">,
Review of Dercum's disease and proposal of diagnostic criteria, diagnostic methods, classification and management, Orphanet Journal of Rare Diseases, 2012, Vol. 7, DOI: 10.1186/1750-1172-7-23, PMID: 22546240, PMC: 3444313, Full text,</ref>
Dercum's disease was first described at Jefferson Medical College by neurologist Francis Xavier Dercum in 1892.<ref name=EMedicine1082083>Adiposis Dolorosa at eMedicine </ref>
Signs and symptoms
Four cardinal symptoms have sometimes been used as diagnostic criteria:
- painful, fatty lipomas (benign fatty tumors) across anatomy
- obesity, frequently in menopausal age
- weakness and fatigue
- emotional instability, depression, epilepsy, confusion and dementia.
There are also potential signs of the disease which are identified as the following:
However, as it is unclear which symptoms are cardinal and which symptoms are minor signs in Dercum's disease, it is unclear which should be used as diagnostic criteria. Researchers have proposed a 'minimal definition' based on symptoms most often part of Dercum's disease: 1) Generalized overweight or obesity. 2) Chronic pain in the adipose tissue.<ref name="ojrd.com" /> The associated symptoms in Dercum's disease include obesity, fatty deposits, easy bruisability, sleep disturbances, impaired memory, depression, difficulty concentrating, anxiety, rapid heartbeat, shortness of breath, diabetes, bloating, constipation, fatigue, weakness and joint and muscle aches.<ref name=EMedicine1082083/> Regarding the associated symptoms in Dercum's disease, only case reports have been published. No study involving medical examinations has been performed in a large group of patients.<ref name="ojrd.com" />
Causes
There are no currently known causes of this disease. There are studies currently proposing several theories of the causes which include inflammation of the adipose tissue, nervous system malfunction and endocrine malfunction. None of the theories that are currently proposed have been found viable.<ref>Adiposis Dolorosa~clinical at eMedicine </ref> Since little is known about Dercum's disease, there are currently no known modes of prevention.
Mechanisms
There are currently no known mechanisms for this disease.
Diagnosis
Diagnosis of Dercum's disease is done through a physical examination. In order to properly diagnose the patient, the doctor must first exclude all other possible differential diagnosis. The basic criteria for Dercum's disease are patients with chronic pain in the adipose tissue (body fat) and patients who are also obese. Although rare, the diagnosis may not include obesity.<ref name="Hansson 23">Hansson, Emma,
Review of Dercum's disease and proposal of diagnostic criteria, diagnostic methods, classification and management, Orphanet Journal of Rare Diseases, Vol. 7, pp. 23, DOI: 10.1186/1750-1172-7-23, PMID: 22546240, PMC: 3444313,</ref> Dercum's disease can also be inherited and a family medical history may aid in the diagnosis of this disease.<ref name=":0">Hansson, Emma, Review of Dercum's disease and proposal of diagnostic criteria, diagnostic methods, classification and management, Orphanet Journal of Rare Diseases, Vol. 7(Issue: 1), pp. 23, DOI: 10.1186/1750-1172-7-23, PMID: 22546240, PMC: 3444313,</ref> There are no specific laboratory test for this disease. Ultrasound and magnetic resonance imaging can play a role in diagnosis.<ref name="MRI & Ultrasound Appearances">, Adiposis dolorosa (Dercum's disease): MRI and ultrasound appearances, Clinical Radiology, Vol. 68(Issue: 10), pp. 1047–53, DOI: 10.1016/j.crad.2013.05.004, PMID: 23809264,</ref>
Treatment
Common treatments for Dercum's disease is directed towards treating the individual symptoms. Pain relief medication may be administered to temporarily reduce the discomfort in the patient. Cortisone shots have also been shown to be effective in temporarily reducing the chronic pain. Surgical removal of the damaged adipose tissue can be effective, but often the disease will recur. <ref>Hansson, Emma,
Liposuction may reduce pain in Dercum's disease (adiposis dolorosa), Pain Medicine, Vol. 12(Issue: 6), pp. 942–952, DOI: 10.1111/j.1526-4637.2011.01101.x, PMID: 21481169,</ref>
Few convincing large studies on the treatment of Dercum's disease have been conducted. Most of the different treatment strategies that exist are based on case reports.<ref name="ojrd.com" /> Currently, there is a lack of scientific data on the use of integrative therapies for the treatment or prevention of Dercum's disease.<ref name="Natural Standard Research Collaboration">
Dercum's disease(link). Natural Retail Group.
</ref><ref>
Dercum's disease(link). Natural Standard Professional Database.
(registration required) </ref> Not enough studies have been done to substantiate that diet and supplements could help with the disease.
Treatment methods include the following modalities:
Surgery
Surgical excision of fatty tissue deposits around joints (liposuction) has been used in some cases.<ref>,
Liposuction in the treatment of juxta-articular adiposis dolorosa, Annals of the Rheumatic Diseases, 1990, Vol. 49(Issue: 6), pp. 403–404, DOI: 10.1136/ard.49.6.403, PMID: 2383065, PMC: 1004110,</ref> Liposuction may temporarily relieve symptoms although recurrences often develop. <ref>Hansson, Emma, Liposuction may reduce pain in Dercum's disease (adiposis dolorosa), Pain Medicine, Vol. 12(Issue: 6), pp. 942–952, DOI: 10.1111/j.1526-4637.2011.01101.x, PMID: 21481169,</ref>
Medication
Traditional analgesics
The pain in Dercum's disease is often reported to be refractory to analgesics and to non-steroidal anti-inflammatory drugs (NSAIDs). However, this has been contradicted by the findings of Herbst et al. They reported that the pain diminished in 89% of patients (n=89) when treated with NSAIDs and in 97% of patients when treated with narcotic analgesics (n=37). The dosage required and the duration of the pain relief are not precisely stated in the article.<ref name="ojrd.com"/><ref name="painful fat">,
Adiposis Dolorosa Is More Than Painful Fat, The Endocrinologist, Vol. 17(Issue: 6), pp. 326–334, DOI: 10.1097/TEN.0b013e31815942294,</ref>
Lidocaine
An early report from 1934 showed that intralesional injections of procaine (Novocain®) relieved pain in six cases. More recently, other types of local treatment of painful sites with lidocaine patches (5%) (Lidoderm®) or lidocaine/prilocaine (25 mg/25 mg) cream (EMLA®) have shown a reduction of pain in a few cases.<ref name="ojrd.com"/>
In the 1980s, treatment with intravenous infusions of lidocaine (Xylocaine®) in varying doses was reported in nine patients. The resulting pain relief lasted from 10 hours to 12 months. In five of the cases, the lidocaine treatment was combined with mexiletine (Mexitil®), which is a class 1B anti-arrhythmic with similar pharmacological properties as lidocaine. The mechanism by which lidocaine reduces pain in Dercum's disease is unclear. It may block impulse conduction in peripheral nerves, and thereby disconnect abnormal nervous impulse circuits. Nonetheless, it might also depress cerebral activity that could lead to increased pain thresholds. Iwane et al. performed an EEG during the administration of intravenous lidocaine. The EEG showed slow waves appearing 7 minutes after the start of the infusion and disappearing within 20 minutes after the end of the infusion. On the other hand, the pain relief effect was the greatest at about 20 minutes after the end of the infusion.<ref name="ojrd.com"/>
Based on this, the authors concluded that the effect of lidocaine on peripheral nerves most likely explains why the drug has an effect on pain in Dercum's disease. In contrast, Atkinson et al. have suggested that an effect on the central nervous system is more likely, as lidocaine can depress consciousness and decrease cerebral metabolism. In addition, Skagen et al. demonstrated that a patient with Dercum's disease lacked the vasoconstrictor response to arm and leg lowering, which indicated that the sympathicusmediated local veno-arteriolar reflex was absent. This could suggest increased sympathetic activity. An infusion of lidocaine increased blood flow in subcutaneous tissue and normalised the vasoconstrictor response when the limbs were lowered. The authors suggested that the pain relief was caused by a normalisation of up-regulated sympathetic activity.<ref name="ojrd.com"/>
Methotrexate and infliximab
One patient's symptoms were improved with methotrexate and infliximab. However, in another patient with Dercum's disease, the effect of methotrexate was discreet. The mechanism of action is unclear. Previously, methotrexate has been shown to reduce neuropathic pain caused by peripheral nerve injury in a study on rats. The mechanism in the rat study case was thought to be a decrease in microglial activation subsequent to nerve injury. Furthermore, a study has shown that infliximab reduces neuropathic pain in patients with central nervous system sarcoidosis. The mechanism is thought to be mediated by tumour necrosis factor inhibition.<ref name="ojrd.com"/>
Interferon α-2b
Two patients were successfully treated with interferon α-2b. The authors speculated on whether the mechanism could be the antiviral effect of the drug, the production of endogenous substances, such as endorphins, or interference with the production of interleukin-1 and tumour necrosis factor. Interleukin-1 and tumour necrosis factor are involved in cutaneous hyperalgesia.<ref name="ojrd.com"/>
Corticosteroids
A few patients noted some improvement when treated with systemic corticosteroids (prednisolone), whereas others experienced worsening of the pain. Weinberg et al. treated two patients with juxta-articular Dercum's disease with intralesional injections of methylprednisolone (Depo-Medrol). The patients experienced a dramatic improvement. The mechanism for the pain-reducing ability of corticosteroids in some conditions is unknown. One theory is that they inhibit the effects of substances, such as histamine, serotonin, bradykinin, and prostaglandins. As the aetiology of Dercum's disease is probably not inflammatory, it is plausible that the improvement some of the patients experience when using corticosteroids is not caused by an anti-inflammatory effect.<ref name="ojrd.com"/>
Alternative treatment
CVAC sessions
Cyclic Variations in Adaptive Conditioning (CVAC) is a method of touch free cyclic hypobaric pneumatic compression for treatment of tissue edema and, therefore, edema-associated pain. As a pilot study, 10 participants with AD completed pain and quality of life questionnaires before and after 20–40 minutes of CVAC process daily for 5 days. After treatment, there was a significant decrease in pain as measured by the Pain Catastrophizing Scale and the Visual Analogue Scale, but there was no change in pain quality by the McGill Pain Questionnaire. However, there were no changes in the Pain Disability Index or Pittsburgh Sleep Quality Index. This study suggests a potential treatment role for CVAC, and the authors recommended randomized controlled clinical trials.<ref>,
Pilot study: Rapidly cycling hypobaric pressure improves pain after 5 days in adiposis dolorosa, Journal of Pain Research, 2010, Vol. 3, pp. 147–153, DOI: 10.2147/JPR.S12351, PMID: 21197318, PMC: 3004643,</ref><ref>
Terms of Use(link). {{{website}}}.
</ref>
Epidemiology
Dercum's disease most commonly appears between the ages of 35 and 50 years of age.<ref name="ojrd.com"/> It is five to thirty times more common in women than in men.<ref name="ojrd.com"/> Originally, Dercum proposed that the condition mainly affects postmenopausal women. However, a 2007 survey has revealed that 85.7 percent of the included patients developed Dercum's disease before menopause.<ref name="ojrd.com"/> The prevalence of Dercum's disease has not yet been exactly established.<ref name="ojrd.com"/>
-
Adiposis dolorosa