HIV: Difference between revisions
CSV import |
No edit summary |
||
| Line 1: | Line 1: | ||
' | [[File:HIV-budding-Color.jpg|HIV-budding-Color.jpg|thumb]] | ||
[[File:HI-virion-structure en.svg|thumb|Diagram of the HIV virion]] | |||
[[File:HIV Mature and Immature.PNG|thumb|right|Diagram of the immature and mature forms of HIV]] | |||
[[File:HIV Membrane fusion panel.svg|thumb|Mechanism of viral entry]] | |||
[[File:HIV on macrophage.png|thumb|right|HIV assembling on the [[Cell membrane|surface]] of an infected [[macrophage]]. The HIV virions have been marked with a green [[fluorescent tag]] and then viewed under a fluorescent microscope.]] | |||
[[File:HIV-genome.png|thumb|Structure of the RNA genome of HIV-1]] | |||
[[File:HIV-replication-cycle-en.svg|thumb|The HIV replication cycle]] | |||
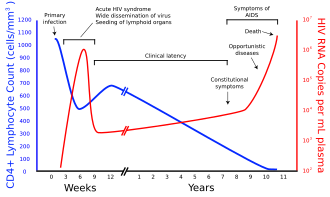
[[File:Hiv-timecourse copy.svg|thumb|right|A generalized graph of the relationship between HIV copies (viral load) and CD4 counts over the average course of untreated HIV infection; any particular individual's disease course may vary considerably.]] | |||
[[File:Itrafig2.jpg|thumb|[[Clathrin-mediated endocytosis]]]] | |||
[[File:Protein Structure Diagram of Fusion Peptide Epitope on HIV Spike (41863579304).jpg|thumb|A diagram of the HIV spike protein (green), with the fusion peptide epitope highlighted in red, and a broadly neutralizing antibody (yellow) binding to the fusion peptide]] | |||
[[File:Reverse Transcription.png|thumb|[[Reverse transcription]] of the HIV [[genome]] into [[double-stranded DNA]]]] | |||
[[File:Virus infecting lymphocytes.gif|thumb|Animation demonstrating cell-free spread of HIV]] | |||
[[File:SIV primates.jpg|left|thumb|Left to right: the [[African green monkey]] source of [[Simian immunodeficiency virus|SIV]], the [[sooty mangabey]] source of [[HIV-2]], and the chimpanzee source of [[HIV-1]]]] | |||
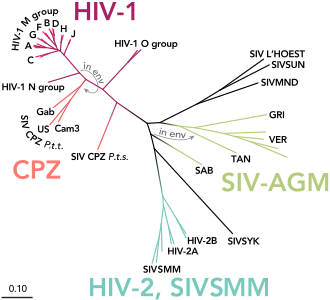
[[File:HIV-SIV-phylogenetic-tree straight.svg|thumb|The [[phylogenetic tree]] of the SIV and HIV]] | |||
'''Human Immunodeficiency Virus''' ('''HIV''') is a [[retrovirus]] that targets the [[human immune system]], particularly [[CD4+ T cells]], leading to progressive immune dysfunction. If left untreated, HIV can progress to [[Acquired Immunodeficiency Syndrome]] ('''AIDS'''), a condition characterized by severe immune suppression and susceptibility to [[opportunistic infections]] and certain types of cancer. | |||
== | ==== Discovery and History ==== | ||
The first cases of AIDS were identified in the early 1980s among populations in the [[United States]], particularly in [[San Francisco]] and [[New York City]]. The virus itself was discovered in 1983 by researchers at the [[Pasteur Institute]] in [[France]]. | |||
== | ==== Global Impact ==== | ||
HIV is a major global public health issue, with an estimated 38.4 million people living with the virus worldwide as of 2023. While advances in [[antiretroviral therapy]] (ART) have significantly reduced [[mortality]] and improved quality of life, there is still no [[cure]] for HIV. | |||
== | ==== Modes of Transmission ==== | ||
HIV is | HIV is primarily transmitted through: | ||
* [[Sexual contact]] involving exchange of bodily fluids. | |||
* Sharing of [[contaminated needles]] or syringes. | |||
* [[Mother-to-child transmission]] during childbirth or breastfeeding. | |||
* Transfusion of [[infected blood]] (rare in countries with rigorous screening processes). | |||
== | ==== Common Misconceptions ==== | ||
HIV is not transmitted through: | |||
* Casual contact (e.g., hugging, shaking hands). | |||
* Sharing utensils or toilet seats. | |||
* [[Mosquito]] bites. | |||
== | ==== Stigma and Discrimination ==== | ||
Stigma surrounding HIV remains a significant barrier to [[diagnosis]] and treatment. Education and [[awareness campaigns]] are essential for reducing misconceptions and supporting affected individuals. | |||
==== Public Health Response ==== | |||
Global organizations like [[UNAIDS]], [[WHO]], and [[HIV.gov]] work tirelessly to: | |||
* Promote [[testing and diagnosis]]. | |||
* Ensure access to life-saving [[antiretroviral drugs]]. | |||
* Educate the public about prevention strategies, including [[safe sex]] and [[needle exchange programs]]. | |||
=== Pathophysiology of HIV === | |||
==== Virus Structure and Composition ==== | |||
HIV is an [[enveloped virus]] belonging to the [[Lentivirus]] genus of the [[Retroviridae]] family. Its structure includes: | |||
* A lipid envelope derived from the host cell membrane. | |||
* Surface [[glycoproteins]] (gp120 and gp41) essential for [[host cell]] attachment and entry. | |||
* A capsid containing [[RNA genome]] and essential enzymes, including [[reverse transcriptase]], [[integrase]], and [[protease]]. | |||
==== Mechanism of Infection ==== | |||
1. '''Attachment and Entry''': HIV binds to the [[CD4 receptor]] and a co-receptor (CCR5 or CXCR4) on target cells, facilitating entry into the host cell. | |||
2. '''Reverse Transcription''': The viral RNA genome is reverse-transcribed into [[DNA]] by reverse transcriptase. | |||
3. '''Integration''': The viral DNA is integrated into the host genome by integrase, forming a [[provirus]]. | |||
4. '''Replication''': The host cell machinery transcribes and translates viral proteins. | |||
5. '''Assembly and Release''': New virions are assembled and released to infect other cells. | |||
==== Impact on the Immune System ==== | |||
HIV primarily targets [[CD4+ T cells]], leading to: | |||
* Gradual depletion of CD4+ T cells. | |||
* Impaired [[cell-mediated immunity]]. | |||
* Increased vulnerability to opportunistic infections such as [[Pneumocystis jirovecii pneumonia]] and [[tuberculosis]]. | |||
==== Stages of HIV Infection ==== | |||
HIV infection progresses through the following stages: | |||
* '''Acute Stage''': Characterized by flu-like symptoms and high viral load. | |||
* '''Chronic Stage''': Often asymptomatic but marked by ongoing viral replication and immune decline. | |||
* '''AIDS''': Defined by CD4+ T cell counts below 200 cells/μL or the presence of opportunistic infections. | |||
==== Key Statistics ==== | |||
* Approximately 1.5 million new infections occur annually. | |||
* HIV disproportionately affects [[sub-Saharan Africa]], which accounts for nearly 70% of cases worldwide. | |||
* Early detection and ART can increase life expectancy to near normal levels. | |||
=== Diagnosis and Testing === | |||
==== Importance of Early Diagnosis ==== | |||
Early diagnosis of HIV is critical for improving outcomes, reducing transmission, and initiating [[antiretroviral therapy]] (ART) as soon as possible. Testing helps individuals: | |||
* Understand their status. | |||
* Seek early treatment. | |||
* Reduce the risk of spreading the virus to others. | |||
==== Types of HIV Tests ==== | |||
HIV tests are broadly categorized into: | |||
1. '''[[Antibody Tests]]''': Detect the presence of HIV antibodies in blood or saliva. These are the most common and are effective after the [[window period]]. | |||
2. '''[[Antigen/Antibody Tests]]''': Detect both HIV antigens (p24) and antibodies, providing earlier detection than antibody-only tests. | |||
3. '''[[Nucleic Acid Tests (NAT)]]''': Detect the presence of HIV RNA, often used for early detection or in cases of high-risk exposure. | |||
==== Testing Methods ==== | |||
* '''[[Rapid Diagnostic Tests (RDTs)]]''': Provide results within 20–30 minutes using a small blood sample or oral fluid. | |||
* '''[[Laboratory-Based Tests]]''': Include [[ELISA]] and [[Western blot]] tests, which offer high accuracy but require longer processing times. | |||
* '''[[Home Testing Kits]]''': Approved for use in many countries, allowing individuals to test themselves privately. | |||
==== HIV Testing Recommendations ==== | |||
* Routine testing is recommended for individuals aged 13–64 years at least once in their lifetime. | |||
* High-risk populations, such as those with multiple sexual partners or [[intravenous drug use|IV drug users]], should be tested more frequently. | |||
* Pregnant women are advised to undergo HIV testing during prenatal care to prevent mother-to-child transmission. | |||
==== Confidentiality and Counseling ==== | |||
HIV testing should always be accompanied by: | |||
* '''[[Pre-test counseling]]''': Educating individuals about the testing process and potential outcomes. | |||
* '''[[Post-test counseling]]''': Providing support and resources for both positive and negative results. | |||
* Ensuring confidentiality to reduce stigma and encourage testing. | |||
==== Advances in Testing ==== | |||
Technological advancements have led to: | |||
* Development of [[point-of-care testing]] for quicker results. | |||
* Improved sensitivity and specificity of tests, reducing false negatives and false positives. | |||
* Integration of HIV testing into routine healthcare services. | |||
=== Treatment and Management === | |||
==== Antiretroviral Therapy (ART) ==== | |||
Antiretroviral therapy is the cornerstone of HIV management. It involves a combination of medications that: | |||
* Suppress [[viral replication]]. | |||
* Restore and preserve [[immune function]]. | |||
* Reduce the risk of [[HIV transmission]]. | |||
Common classes of ART include: | |||
* '''[[Nucleoside Reverse Transcriptase Inhibitors (NRTIs)]]''': Block reverse transcription by mimicking natural nucleosides. | |||
* '''[[Non-Nucleoside Reverse Transcriptase Inhibitors (NNRTIs)]]''': Bind directly to reverse transcriptase, inhibiting its function. | |||
* '''[[Protease Inhibitors (PIs)]]''': Prevent the processing of viral proteins, disrupting the formation of new virions. | |||
* '''[[Integrase Strand Transfer Inhibitors (INSTIs)]]''': Block the integration of viral DNA into the host genome. | |||
* '''[[Entry and Fusion Inhibitors]]''': Prevent the virus from entering host cells. | |||
==== Goals of Treatment ==== | |||
The primary goals of ART are: | |||
* Achieving and maintaining an undetectable [[viral load]]. | |||
* Increasing [[CD4+ T cell counts]]. | |||
* Improving overall quality of life. | |||
==== Monitoring and Follow-Up ==== | |||
Regular monitoring is essential for effective HIV management. Key aspects include: | |||
* '''Viral Load Testing''': To assess the effectiveness of ART. | |||
* '''CD4 Count Monitoring''': To evaluate immune function. | |||
* '''Drug Resistance Testing''': To adjust treatment if resistance develops. | |||
==== Managing Comorbidities ==== | |||
People living with HIV are at increased risk of comorbidities such as: | |||
* [[Cardiovascular disease]]. | |||
* [[Chronic kidney disease]]. | |||
* [[Hepatitis B]] and [[Hepatitis C]] coinfections. | |||
Integrated care addressing these conditions is crucial for optimal outcomes. | |||
==== Adherence to Therapy ==== | |||
Adherence to ART is critical for: | |||
* Preventing the development of [[drug resistance]]. | |||
* Achieving long-term viral suppression. | |||
Strategies to improve adherence include: | |||
* Patient education. | |||
* Simplified regimens with fewer pills. | |||
* Regular counseling and support. | |||
=== Prevention Strategies === | |||
Preventing the spread of HIV is critical to controlling the global epidemic. Comprehensive prevention strategies focus on reducing transmission through a combination of behavioral, biomedical, and structural interventions. | |||
==== Biomedical Interventions ==== | |||
* '''[[Pre-exposure Prophylaxis (PrEP)]]''': A daily medication that significantly reduces the risk of acquiring HIV when taken consistently. | |||
* '''[[Post-exposure Prophylaxis (PEP)]]''': An emergency treatment started within 72 hours of potential HIV exposure to prevent infection. | |||
* '''[[Condoms]]''': Consistent and correct use of male and female condoms significantly reduces the risk of sexual transmission. | |||
* '''[[Needle and Syringe Programs (NSPs)]]''': Provide clean injecting equipment to reduce transmission among people who inject drugs. | |||
* '''[[Treatment as Prevention (TasP)]]''': Achieving and maintaining an undetectable viral load through ART eliminates the risk of sexual transmission (Undetectable = Untransmittable or U=U). | |||
==== Behavioral Interventions ==== | |||
* '''Education and Awareness Campaigns''': Increase knowledge about HIV transmission and prevention. | |||
* '''Reducing Risky Behaviors''': Encourage safe sex practices, including limiting the number of sexual partners. | |||
* '''Voluntary Medical Male Circumcision (VMMC)''': Reduces the risk of heterosexual transmission in high-prevalence settings. | |||
==== Structural Interventions ==== | |||
* '''HIV Testing and Counseling Services''': Increase access to and utilization of testing facilities. | |||
* '''Reducing Stigma and Discrimination''': Promote supportive environments for people living with and at risk of HIV. | |||
* '''Policy and Legal Frameworks''': Enforce measures to ensure equitable access to prevention tools and healthcare services. | |||
==== Special Considerations for Key Populations ==== | |||
Prevention strategies must address the unique needs of: | |||
* [[Sex workers]]. | |||
* [[Men who have sex with men (MSM)]]. | |||
* [[People who inject drugs]]. | |||
* [[Adolescents and young adults]]. | |||
* [[Pregnant women]] to prevent mother-to-child transmission. | |||
=== HIV in Vulnerable Populations === | |||
HIV disproportionately affects vulnerable populations due to a combination of social, economic, and behavioral factors. Addressing the needs of these groups is critical for reducing HIV prevalence and improving health outcomes. | |||
==== Key Populations ==== | |||
1. '''[[Men who have sex with men (MSM)]]''': | |||
* Higher risk due to biological and behavioral factors. | |||
* Stigma and discrimination often limit access to prevention and treatment services. | |||
2. '''[[Sex Workers]]''': | |||
* Increased risk due to multiple sexual partners and limited access to protective measures. | |||
* Advocacy for legal and health protections is essential. | |||
3. '''[[People who inject drugs (PWID)]]''': | |||
* Shared needles and syringes significantly increase transmission risk. | |||
* Needle exchange programs and opioid substitution therapy (OST) are effective interventions. | |||
4. '''[[Transgender Individuals]]''': | |||
* Experience high levels of stigma, discrimination, and violence. | |||
* Tailored interventions are required to address their unique needs. | |||
5. '''[[Adolescents and Young Adults]]''': | |||
* Account for a significant proportion of new infections. | |||
* Comprehensive sexual education and youth | |||
==== References ==== | |||
* [[HIV.gov]]. (2024). "What is HIV?" [https://www.hiv.gov] | |||
* [[World Health Organization]]. (2023). "HIV/AIDS Fact Sheet." [https://www.who.int] | |||
* UNAIDS. (2023). "Global HIV & AIDS Statistics." [https://www.unaids.org] | |||
* [[Centers for Disease Control and Prevention]]. (2023). "HIV Basics." [https://www.cdc.gov] | |||
* [[National Institutes of Health]]. (2023). "HIV Mechanisms." [https://www.nih.gov] | |||
==See Also== | ==See Also== | ||
* [[AIDS]] | * [[AIDS]] | ||
| Line 22: | Line 222: | ||
* [[Pre-exposure prophylaxis]] | * [[Pre-exposure prophylaxis]] | ||
* [[Post-exposure prophylaxis]] | * [[Post-exposure prophylaxis]] | ||
[[Category:Medical Conditions]] | [[Category:Medical Conditions]] | ||
[[Category:Infectious Diseases]] | [[Category:Infectious Diseases]] | ||
[[Category:Virology]] | [[Category:Virology]] | ||
{{HIV and AIDS}} | |||
{{STD and STI}} | |||
{{Retroviruses}} | |||
{{Taxonbar|from=Q15787}} | |||
{{DEFAULTSORT:Hiv}} | |||
[[Category:HIV/AIDS|*]] | |||
[[Category:Causes of death]] | |||
[[Category:Discovery and invention controversies]] | |||
[[Category:IARC Group 2B carcinogens]] | |||
[[Category:Lentiviruses]] | |||
[[Category:Sexually transmitted diseases and infections]] | |||
[[Category:1983 in biology]] | |||
{{stub}} | {{stub}} | ||
Revision as of 21:20, 18 January 2025












Human Immunodeficiency Virus (HIV) is a retrovirus that targets the human immune system, particularly CD4+ T cells, leading to progressive immune dysfunction. If left untreated, HIV can progress to Acquired Immunodeficiency Syndrome (AIDS), a condition characterized by severe immune suppression and susceptibility to opportunistic infections and certain types of cancer.
Discovery and History
The first cases of AIDS were identified in the early 1980s among populations in the United States, particularly in San Francisco and New York City. The virus itself was discovered in 1983 by researchers at the Pasteur Institute in France.
Global Impact
HIV is a major global public health issue, with an estimated 38.4 million people living with the virus worldwide as of 2023. While advances in antiretroviral therapy (ART) have significantly reduced mortality and improved quality of life, there is still no cure for HIV.
Modes of Transmission
HIV is primarily transmitted through:
- Sexual contact involving exchange of bodily fluids.
- Sharing of contaminated needles or syringes.
- Mother-to-child transmission during childbirth or breastfeeding.
- Transfusion of infected blood (rare in countries with rigorous screening processes).
Common Misconceptions
HIV is not transmitted through:
- Casual contact (e.g., hugging, shaking hands).
- Sharing utensils or toilet seats.
- Mosquito bites.
Stigma and Discrimination
Stigma surrounding HIV remains a significant barrier to diagnosis and treatment. Education and awareness campaigns are essential for reducing misconceptions and supporting affected individuals.
Public Health Response
Global organizations like UNAIDS, WHO, and HIV.gov work tirelessly to:
- Promote testing and diagnosis.
- Ensure access to life-saving antiretroviral drugs.
- Educate the public about prevention strategies, including safe sex and needle exchange programs.
Pathophysiology of HIV
Virus Structure and Composition
HIV is an enveloped virus belonging to the Lentivirus genus of the Retroviridae family. Its structure includes:
- A lipid envelope derived from the host cell membrane.
- Surface glycoproteins (gp120 and gp41) essential for host cell attachment and entry.
- A capsid containing RNA genome and essential enzymes, including reverse transcriptase, integrase, and protease.
Mechanism of Infection
1. Attachment and Entry: HIV binds to the CD4 receptor and a co-receptor (CCR5 or CXCR4) on target cells, facilitating entry into the host cell. 2. Reverse Transcription: The viral RNA genome is reverse-transcribed into DNA by reverse transcriptase. 3. Integration: The viral DNA is integrated into the host genome by integrase, forming a provirus. 4. Replication: The host cell machinery transcribes and translates viral proteins. 5. Assembly and Release: New virions are assembled and released to infect other cells.
Impact on the Immune System
HIV primarily targets CD4+ T cells, leading to:
- Gradual depletion of CD4+ T cells.
- Impaired cell-mediated immunity.
- Increased vulnerability to opportunistic infections such as Pneumocystis jirovecii pneumonia and tuberculosis.
Stages of HIV Infection
HIV infection progresses through the following stages:
- Acute Stage: Characterized by flu-like symptoms and high viral load.
- Chronic Stage: Often asymptomatic but marked by ongoing viral replication and immune decline.
- AIDS: Defined by CD4+ T cell counts below 200 cells/μL or the presence of opportunistic infections.
Key Statistics
- Approximately 1.5 million new infections occur annually.
- HIV disproportionately affects sub-Saharan Africa, which accounts for nearly 70% of cases worldwide.
- Early detection and ART can increase life expectancy to near normal levels.
Diagnosis and Testing
Importance of Early Diagnosis
Early diagnosis of HIV is critical for improving outcomes, reducing transmission, and initiating antiretroviral therapy (ART) as soon as possible. Testing helps individuals:
- Understand their status.
- Seek early treatment.
- Reduce the risk of spreading the virus to others.
Types of HIV Tests
HIV tests are broadly categorized into: 1. Antibody Tests: Detect the presence of HIV antibodies in blood or saliva. These are the most common and are effective after the window period. 2. Antigen/Antibody Tests: Detect both HIV antigens (p24) and antibodies, providing earlier detection than antibody-only tests. 3. Nucleic Acid Tests (NAT): Detect the presence of HIV RNA, often used for early detection or in cases of high-risk exposure.
Testing Methods
- Rapid Diagnostic Tests (RDTs): Provide results within 20–30 minutes using a small blood sample or oral fluid.
- Laboratory-Based Tests: Include ELISA and Western blot tests, which offer high accuracy but require longer processing times.
- Home Testing Kits: Approved for use in many countries, allowing individuals to test themselves privately.
HIV Testing Recommendations
- Routine testing is recommended for individuals aged 13–64 years at least once in their lifetime.
- High-risk populations, such as those with multiple sexual partners or IV drug users, should be tested more frequently.
- Pregnant women are advised to undergo HIV testing during prenatal care to prevent mother-to-child transmission.
Confidentiality and Counseling
HIV testing should always be accompanied by:
- Pre-test counseling: Educating individuals about the testing process and potential outcomes.
- Post-test counseling: Providing support and resources for both positive and negative results.
- Ensuring confidentiality to reduce stigma and encourage testing.
Advances in Testing
Technological advancements have led to:
- Development of point-of-care testing for quicker results.
- Improved sensitivity and specificity of tests, reducing false negatives and false positives.
- Integration of HIV testing into routine healthcare services.
Treatment and Management
Antiretroviral Therapy (ART)
Antiretroviral therapy is the cornerstone of HIV management. It involves a combination of medications that:
- Suppress viral replication.
- Restore and preserve immune function.
- Reduce the risk of HIV transmission.
Common classes of ART include:
- Nucleoside Reverse Transcriptase Inhibitors (NRTIs): Block reverse transcription by mimicking natural nucleosides.
- Non-Nucleoside Reverse Transcriptase Inhibitors (NNRTIs): Bind directly to reverse transcriptase, inhibiting its function.
- Protease Inhibitors (PIs): Prevent the processing of viral proteins, disrupting the formation of new virions.
- Integrase Strand Transfer Inhibitors (INSTIs): Block the integration of viral DNA into the host genome.
- Entry and Fusion Inhibitors: Prevent the virus from entering host cells.
Goals of Treatment
The primary goals of ART are:
- Achieving and maintaining an undetectable viral load.
- Increasing CD4+ T cell counts.
- Improving overall quality of life.
Monitoring and Follow-Up
Regular monitoring is essential for effective HIV management. Key aspects include:
- Viral Load Testing: To assess the effectiveness of ART.
- CD4 Count Monitoring: To evaluate immune function.
- Drug Resistance Testing: To adjust treatment if resistance develops.
Managing Comorbidities
People living with HIV are at increased risk of comorbidities such as:
- Cardiovascular disease.
- Chronic kidney disease.
- Hepatitis B and Hepatitis C coinfections.
Integrated care addressing these conditions is crucial for optimal outcomes.
Adherence to Therapy
Adherence to ART is critical for:
- Preventing the development of drug resistance.
- Achieving long-term viral suppression.
Strategies to improve adherence include:
- Patient education.
- Simplified regimens with fewer pills.
- Regular counseling and support.
Prevention Strategies
Preventing the spread of HIV is critical to controlling the global epidemic. Comprehensive prevention strategies focus on reducing transmission through a combination of behavioral, biomedical, and structural interventions.
Biomedical Interventions
- Pre-exposure Prophylaxis (PrEP): A daily medication that significantly reduces the risk of acquiring HIV when taken consistently.
- Post-exposure Prophylaxis (PEP): An emergency treatment started within 72 hours of potential HIV exposure to prevent infection.
- Condoms: Consistent and correct use of male and female condoms significantly reduces the risk of sexual transmission.
- Needle and Syringe Programs (NSPs): Provide clean injecting equipment to reduce transmission among people who inject drugs.
- Treatment as Prevention (TasP): Achieving and maintaining an undetectable viral load through ART eliminates the risk of sexual transmission (Undetectable = Untransmittable or U=U).
Behavioral Interventions
- Education and Awareness Campaigns: Increase knowledge about HIV transmission and prevention.
- Reducing Risky Behaviors: Encourage safe sex practices, including limiting the number of sexual partners.
- Voluntary Medical Male Circumcision (VMMC): Reduces the risk of heterosexual transmission in high-prevalence settings.
Structural Interventions
- HIV Testing and Counseling Services: Increase access to and utilization of testing facilities.
- Reducing Stigma and Discrimination: Promote supportive environments for people living with and at risk of HIV.
- Policy and Legal Frameworks: Enforce measures to ensure equitable access to prevention tools and healthcare services.
Special Considerations for Key Populations
Prevention strategies must address the unique needs of:
- Sex workers.
- Men who have sex with men (MSM).
- People who inject drugs.
- Adolescents and young adults.
- Pregnant women to prevent mother-to-child transmission.
HIV in Vulnerable Populations
HIV disproportionately affects vulnerable populations due to a combination of social, economic, and behavioral factors. Addressing the needs of these groups is critical for reducing HIV prevalence and improving health outcomes.
Key Populations
1. Men who have sex with men (MSM):
- Higher risk due to biological and behavioral factors.
- Stigma and discrimination often limit access to prevention and treatment services.
2. Sex Workers:
- Increased risk due to multiple sexual partners and limited access to protective measures.
- Advocacy for legal and health protections is essential.
3. People who inject drugs (PWID):
- Shared needles and syringes significantly increase transmission risk.
- Needle exchange programs and opioid substitution therapy (OST) are effective interventions.
- Experience high levels of stigma, discrimination, and violence.
- Tailored interventions are required to address their unique needs.
5. Adolescents and Young Adults:
- Account for a significant proportion of new infections.
- Comprehensive sexual education and youth
References
- HIV.gov. (2024). "What is HIV?" [1]
- World Health Organization. (2023). "HIV/AIDS Fact Sheet." [2]
- UNAIDS. (2023). "Global HIV & AIDS Statistics." [3]
- Centers for Disease Control and Prevention. (2023). "HIV Basics." [4]
- National Institutes of Health. (2023). "HIV Mechanisms." [5]
See Also
| Sexually transmitted infections (STI) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| Virus: Reverse transcribing viruses (Revtraviricetes) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|


