Foot drop: Difference between revisions
No edit summary |
No edit summary |
||
| (One intermediate revision by the same user not shown) | |||
| Line 1: | Line 1: | ||
{{Short description|Condition characterized by difficulty lifting the front part of the foot}} | |||
{{short description|Gait abnormality}} | {{short description|Gait abnormality}} | ||
{{Infobox medical condition (new) | {{Infobox medical condition (new) | ||
| name = | | name = Foot drop | ||
| synonym = | | synonym = Drop foot, peroneal nerve palsy | ||
| image = Foot drop.jpg | | image = Foot drop.jpg | ||
| image_size = | | image_size = 250px | ||
| alt = | | alt = Right foot with drop foot, left foot normal | ||
| caption = Shown here, <br>the right foot drops due to paralysis of the tibialis anterior muscle, <br>while the left foot demonstrates normal lifting abilities. | | caption = Shown here,<br>the right foot drops due to paralysis of the tibialis anterior muscle,<br>while the left foot demonstrates normal lifting abilities. | ||
| pronounce = | | pronounce = /fʊt drɒp/ | ||
| specialty = | | specialty = [[Neurology]], [[Orthopedics]], [[Physical medicine and rehabilitation]] | ||
| symptoms = | | symptoms = Difficulty lifting the front part of the foot, dragging of the toes while walking, high-stepping gait | ||
| complications = | | complications = Falls, muscle atrophy, gait abnormalities | ||
| onset = | | onset = Sudden or gradual, depending on cause | ||
| duration = | | duration = Variable; may be temporary or permanent | ||
| types = | | types = Unilateral or bilateral | ||
| causes = | | causes = Injury to the [[common peroneal nerve]], [[stroke]], [[multiple sclerosis]], [[herniated disc]], muscular or neurological disorders | ||
| risks = | | risks = Prolonged leg crossing, knee surgery, prolonged squatting, trauma | ||
| diagnosis = | | diagnosis = [[Physical examination]], [[electromyography (EMG)]], [[nerve conduction studies]], [[MRI]] | ||
| differential = | | differential = [[Charcot–Marie–Tooth disease]], [[ALS]], [[spinal cord injury]] | ||
| prevention = | | prevention = Avoid nerve compression, protective footwear, manage underlying conditions | ||
| treatment = | | treatment = [[Physical therapy]], [[orthotic]] devices, [[nerve decompression surgery]] | ||
| medication = | | medication = Anti-inflammatory drugs, corticosteroids (if inflammation is the cause) | ||
| prognosis = | | prognosis = Depends on cause; may resolve spontaneously or require long-term therapy | ||
| frequency = | | frequency = Relatively uncommon; exact prevalence unknown | ||
| deaths = | | deaths = Rare; usually not fatal on its own | ||
}} | }} | ||
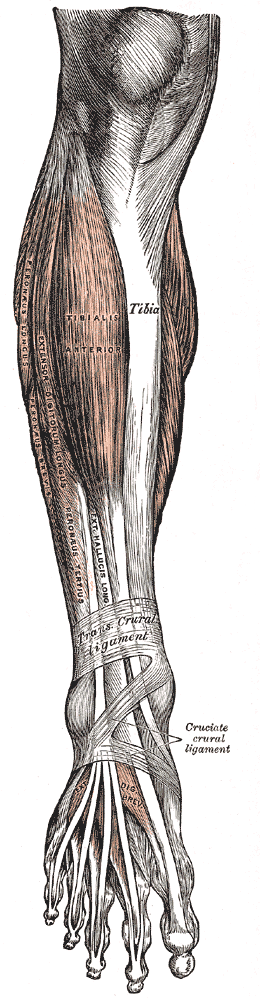
[[Image:gray437.png|thumb|upright=0.7px|Human lower leg anatomy|left]] | |||
[[File:AFO brace for foot drop.JPG|thumb|AFO (Ankle Foot Orthosis) brace is a type of orthotic used to support the foot and ankle.|left]] | |||
[[File:Treatment-of-peroneal-nerve-injuries-with-simultaneous-tendon-transfer-and-nerve-exploration-s13018-014-0067-6-S1.ogv|thumb|A patient recovering from surgery to treat foot drop, with limited [[dorsiflexion|plantar and dorsiflexion]].]] | [[File:Treatment-of-peroneal-nerve-injuries-with-simultaneous-tendon-transfer-and-nerve-exploration-s13018-014-0067-6-S1.ogv|thumb|A patient recovering from surgery to treat foot drop, with limited [[dorsiflexion|plantar and dorsiflexion]].]] | ||
'''Foot drop''' is a [[ | '''Foot drop''' is a [[medical condition]] characterized by difficulty in lifting the front part of the [[foot]]. This condition can cause the foot to drag along the ground while walking. It is not a disease in itself but rather a sign of an underlying neurological, muscular, or anatomical problem. | ||
==Causes== | |||
Foot drop can result from a variety of causes, including: | |||
* [[Nerve injury]]: Damage to the [[peroneal nerve]], which controls the muscles that lift the foot, is a common cause of foot drop. This nerve can be injured due to trauma, surgery, or prolonged pressure on the nerve. | |||
* [[Muscle disorders]]: Conditions such as [[muscular dystrophy]], [[amyotrophic lateral sclerosis]] (ALS), and other muscle diseases can lead to foot drop. | |||
* [[Neurological disorders]]: Disorders affecting the brain or spinal cord, such as [[stroke]], [[multiple sclerosis]], or [[cerebral palsy]], can result in foot drop. | |||
* [[Anatomical abnormalities]]: Structural issues in the foot or leg, such as [[charcot-marie-tooth disease]], can also cause foot drop. | |||
==Symptoms== | |||
The primary symptom of foot drop is the inability to lift the front part of the foot, leading to a characteristic "steppage" gait. Individuals with foot drop may: | |||
* Drag the foot on the ground while walking | |||
* | * Lift the knee higher than usual to prevent the foot from dragging | ||
* | * Experience numbness or tingling in the foot or leg | ||
* | * Have muscle weakness in the foot or leg | ||
==Diagnosis== | ==Diagnosis== | ||
Diagnosing foot drop involves a thorough [[physical examination]] and [[medical history]] review. Additional tests may include: | |||
* [[Electromyography]] (EMG) to assess the electrical activity of muscles | |||
* [[Nerve conduction studies]] to evaluate the function of the nerves | |||
* [[Imaging studies]] such as [[MRI]] or [[CT scan]] to identify structural causes | |||
==Treatment== | ==Treatment== | ||
Treatment for foot drop depends on the underlying cause and may include: | |||
* [[Physical therapy]]: Exercises to strengthen the muscles and improve range of motion | |||
* [[Orthotic devices]]: An [[ankle-foot orthosis]] (AFO) can help support the foot and improve walking | |||
* | * [[Surgery]]: In some cases, surgical intervention may be necessary to repair damaged nerves or tendons | ||
* | * [[Medications]]: To manage pain or underlying conditions contributing to foot drop | ||
* | |||
* | |||
==Prognosis== | |||
The prognosis for foot drop varies depending on the cause. In some cases, foot drop may be temporary and improve with treatment, while in others, it may be permanent. Early diagnosis and treatment are crucial for the best outcomes. | |||
==Related pages== | |||
* [[Peripheral neuropathy]] | |||
* [[Muscular dystrophy]] | |||
* [[Nerve injury]] | |||
* [[Orthotics]] | |||
{{stub}} | |||
[[Category:Gait abnormalities]] | [[Category:Gait abnormalities]] | ||
[[Category:Musculoskeletal disorders]] | [[Category:Musculoskeletal disorders]] | ||
| Line 133: | Line 78: | ||
{{Congenital malformations and deformations of musculoskeletal system}} | {{Congenital malformations and deformations of musculoskeletal system}} | ||
[[Category:Arthropathies]] | [[Category:Arthropathies]] | ||
[[Category:Neurological disorders]] | |||
[[Category:Musculoskeletal disorders]] | |||
Latest revision as of 23:13, 23 March 2025
Condition characterized by difficulty lifting the front part of the foot
Gait abnormality
| Foot drop | |
|---|---|

| |
| Synonyms | N/A |
| Pronounce | /fʊt drɒp/ |
| Field | N/A |
| Symptoms | Difficulty lifting the front part of the foot, dragging of the toes while walking, high-stepping gait |
| Complications | Falls, muscle atrophy, gait abnormalities |
| Onset | Sudden or gradual, depending on cause |
| Duration | Variable; may be temporary or permanent |
| Types | Unilateral or bilateral |
| Causes | Injury to the common peroneal nerve, stroke, multiple sclerosis, herniated disc, muscular or neurological disorders |
| Risks | Prolonged leg crossing, knee surgery, prolonged squatting, trauma |
| Diagnosis | Physical examination, electromyography (EMG), nerve conduction studies, MRI |
| Differential diagnosis | Charcot–Marie–Tooth disease, ALS, spinal cord injury |
| Prevention | Avoid nerve compression, protective footwear, manage underlying conditions |
| Treatment | Physical therapy, orthotic devices, nerve decompression surgery |
| Medication | Anti-inflammatory drugs, corticosteroids (if inflammation is the cause) |
| Prognosis | Depends on cause; may resolve spontaneously or require long-term therapy |
| Frequency | Relatively uncommon; exact prevalence unknown |
| Deaths | Rare; usually not fatal on its own |

Foot drop is a medical condition characterized by difficulty in lifting the front part of the foot. This condition can cause the foot to drag along the ground while walking. It is not a disease in itself but rather a sign of an underlying neurological, muscular, or anatomical problem.
Causes[edit]
Foot drop can result from a variety of causes, including:
- Nerve injury: Damage to the peroneal nerve, which controls the muscles that lift the foot, is a common cause of foot drop. This nerve can be injured due to trauma, surgery, or prolonged pressure on the nerve.
- Muscle disorders: Conditions such as muscular dystrophy, amyotrophic lateral sclerosis (ALS), and other muscle diseases can lead to foot drop.
- Neurological disorders: Disorders affecting the brain or spinal cord, such as stroke, multiple sclerosis, or cerebral palsy, can result in foot drop.
- Anatomical abnormalities: Structural issues in the foot or leg, such as charcot-marie-tooth disease, can also cause foot drop.
Symptoms[edit]
The primary symptom of foot drop is the inability to lift the front part of the foot, leading to a characteristic "steppage" gait. Individuals with foot drop may:
- Drag the foot on the ground while walking
- Lift the knee higher than usual to prevent the foot from dragging
- Experience numbness or tingling in the foot or leg
- Have muscle weakness in the foot or leg
Diagnosis[edit]
Diagnosing foot drop involves a thorough physical examination and medical history review. Additional tests may include:
- Electromyography (EMG) to assess the electrical activity of muscles
- Nerve conduction studies to evaluate the function of the nerves
- Imaging studies such as MRI or CT scan to identify structural causes
Treatment[edit]
Treatment for foot drop depends on the underlying cause and may include:
- Physical therapy: Exercises to strengthen the muscles and improve range of motion
- Orthotic devices: An ankle-foot orthosis (AFO) can help support the foot and improve walking
- Surgery: In some cases, surgical intervention may be necessary to repair damaged nerves or tendons
- Medications: To manage pain or underlying conditions contributing to foot drop
Prognosis[edit]
The prognosis for foot drop varies depending on the cause. In some cases, foot drop may be temporary and improve with treatment, while in others, it may be permanent. Early diagnosis and treatment are crucial for the best outcomes.
Related pages[edit]
|
|
|
| Congenital malformations and deformations of musculoskeletal system / musculoskeletal abnormality | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|


