Bronchopulmonary dysplasia: Difference between revisions
m 1 revision imported |
CSV import |
||
| (6 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
{{SI}} | |||
{{Infobox medical condition | |||
| name = Bronchopulmonary dysplasia | |||
| image = [[File:CXR_-_Bronchopulmonary_dysplasia.jpg|250px]] | |||
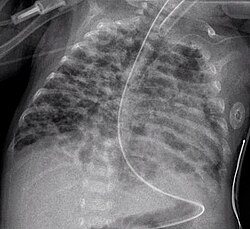
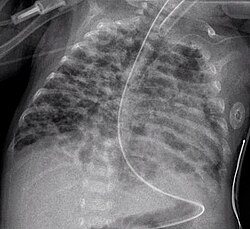
| caption = Chest X-ray of a patient with bronchopulmonary dysplasia | |||
| synonyms = Chronic lung disease of prematurity | |||
| field = [[Pediatrics]], [[Neonatology]] | |||
| symptoms = [[Tachypnea]], [[retractions]], [[hypoxemia]], [[cyanosis]] | |||
| complications = [[Pulmonary hypertension]], [[growth failure]], [[neurodevelopmental impairment]] | |||
| onset = Usually in [[premature infants]] | |||
| duration = Can be chronic | |||
| causes = [[Premature birth]], [[mechanical ventilation]], [[oxygen toxicity]] | |||
| risks = [[Prematurity]], [[low birth weight]], [[prolonged mechanical ventilation]] | |||
| diagnosis = [[Chest X-ray]], [[clinical evaluation]] | |||
| differential = [[Respiratory distress syndrome]], [[pneumonia]], [[congenital heart disease]] | |||
| prevention = [[Antenatal steroids]], [[surfactant therapy]], [[gentle ventilation strategies]] | |||
| treatment = [[Oxygen therapy]], [[diuretics]], [[bronchodilators]], [[nutritional support]] | |||
| prognosis = Variable; some improve with age, others may have long-term complications | |||
| frequency = Affects a significant number of very low birth weight infants | |||
}} | |||
{{Short description|A chronic lung disease affecting premature infants}} | |||
{{Infobox medical condition (new) | {{Infobox medical condition (new) | ||
| name | | name = Bronchopulmonary dysplasia | ||
| synonyms | | synonyms = BPD | ||
| image | | image = CXR - Bronchopulmonary dysplasia.jpg | ||
| caption | | caption = Chest X-ray of bronchopulmonary dysplasia showing diffuse haziness and areas of hyperinflation | ||
| pronounce | | pronounce = | ||
| field | | field = [[Pulmonology]], [[Neonatology]] | ||
| symptoms | | symptoms = [[Tachypnea]], [[retractions]], hypoxemia, need for prolonged [[oxygen therapy]] | ||
| complications | | complications = [[Pulmonary hypertension]], [[growth failure]], recurrent [[respiratory infections]] | ||
| onset | | onset = Typically within the first 4 weeks of life | ||
| duration | | duration = Chronic; may persist into childhood | ||
| types | | types = Mild, moderate, severe (based on oxygen requirement at 36 weeks postmenstrual age) | ||
| causes | | causes = Lung injury from mechanical ventilation and/or oxygen therapy | ||
| risks | | risks = Prematurity, low birth weight, infection, PDA, high oxygen exposure | ||
| diagnosis | | diagnosis = Clinical criteria, oxygen requirement at 28 days and 36 weeks PMA, [[chest X-ray]] | ||
| differential | | differential = [[Respiratory distress syndrome]], [[congenital pneumonia]], pulmonary hypoplasia | ||
| prevention | | prevention = [[Antenatal corticosteroids]], [[non-invasive ventilation]], [[surfactant therapy]] | ||
| treatment | | treatment = Respiratory support, nutrition, bronchodilators, diuretics, corticosteroids | ||
| medication | | medication = [[Albuterol]], [[furosemide]], [[dexamethasone]] | ||
| prognosis | | prognosis = Variable; some resolve over time, others have long-term respiratory issues | ||
| frequency | | frequency = ~10,000–15,000 cases/year in the U.S. | ||
| deaths | | deaths = Associated with severity; improved survival with neonatal care advances | ||
}} | }} | ||
'''Bronchopulmonary dysplasia''' ('''BPD | '''Bronchopulmonary dysplasia''' ('''BPD''') is a chronic [[lung disease]] that primarily affects [[premature birth|premature infants]] who have received [[mechanical ventilation]] or supplemental [[oxygen therapy]] to treat [[respiratory distress syndrome]] (RDS). It is characterized by abnormal development of the [[alveoli]], inflammation, and pulmonary fibrosis, leading to long-term respiratory difficulties. | ||
== History == | |||
The term "bronchopulmonary dysplasia" was first described in 1967 by Dr. William Northway to characterize the chronic lung damage observed in premature infants treated with high levels of oxygen and prolonged mechanical ventilation. Advances in [[neonatal intensive care]] have since altered the presentation and understanding of BPD, shifting from scarring to more developmental arrest in alveolarization. | |||
== Pathophysiology == | |||
== | BPD results from a combination of factors that injure the immature lungs, including: | ||
* Barotrauma from [[mechanical ventilation]] | |||
* Oxygen toxicity from high inspired oxygen concentrations | |||
* Inflammatory responses to infection or ventilation | |||
* [[ | * Poor postnatal nutrition | ||
* [[ | These injuries disrupt the normal development of alveoli and pulmonary vasculature. The lungs of infants with BPD show fewer, larger alveoli with thickened septa, impaired gas exchange, and increased airway resistance. | ||
* [[ | == Risk Factors == | ||
Risk factors for developing BPD include: | |||
* Extreme [[prematurity]] (especially <28 weeks gestation) | |||
* | * Very low [[birth weight]] (<1500g) | ||
* | * Prolonged requirement for [[positive pressure ventilation]] | ||
* High concentrations of inspired oxygen | |||
* [[ | * Prenatal or postnatal [[infections]] (e.g., [[chorioamnionitis]], [[sepsis]]) | ||
* [[Patent ductus arteriosus]] (PDA) | |||
* Genetic susceptibility and intrauterine growth restriction (IUGR) | |||
== Clinical Presentation == | |||
Signs and symptoms may include: | |||
* Persistent [[tachypnea]] and [[retractions]] | |||
* Difficulty weaning from respiratory support | |||
* Poor feeding and [[failure to thrive]] | |||
* Need for supplemental oxygen beyond 28 days of life | |||
* Recurrent [[respiratory infections]] | |||
* Signs of [[pulmonary hypertension]] in severe cases | |||
== Diagnosis == | == Diagnosis == | ||
BPD is diagnosed based on: | |||
* The need for oxygen supplementation at 28 days of life and at 36 weeks postmenstrual age (PMA) | |||
* Severity classification (mild, moderate, severe) depends on oxygen dependency and respiratory support at 36 weeks PMA or 56 days of life | |||
* [[Chest X-ray]] may show areas of: | |||
** [[Atelectasis]] | |||
** Hyperinflation | |||
** Linear opacities or cystic changes | |||
* Pulmonary function testing and echocardiography may aid in assessment | |||
== Management == | |||
Management of BPD involves a multidisciplinary approach: | |||
The | * Respiratory support: Minimize further lung injury using non-invasive methods like CPAP or nasal cannula when possible | ||
* Pharmacologic therapy: | |||
** [[Bronchodilators]] (e.g., albuterol) | |||
** [[Diuretics]] (e.g., furosemide) to reduce pulmonary edema | |||
* | ** [[Corticosteroids]] (e.g., dexamethasone or hydrocortisone) in select cases | ||
* Nutrition: High-calorie feeds and possible [[gastrostomy]] to support growth and healing | |||
* Treatment of complications: Monitor for and manage [[pulmonary hypertension]], tracheomalacia, and infections | |||
== Complications == | |||
Long-term complications of BPD may include: | |||
* Chronic obstructive lung disease in childhood | |||
* [[Asthma]]-like symptoms | |||
* | * Recurrent [[bronchiolitis]] or pneumonia | ||
* | * Need for home oxygen or [[tracheostomy]] in severe cases | ||
* [[Neurodevelopmental delay]] due to prolonged NICU stay | |||
==Management== | == Prognosis == | ||
Prognosis depends on: | |||
* Degree of prematurity | |||
[[ | * Severity of lung damage | ||
* Presence of comorbidities | |||
With modern neonatal care, survival rates have improved, and many infants recover lung function over time. However, some children continue to have respiratory and developmental issues into adolescence. | |||
== Prevention == | |||
Preventive measures include: | |||
* [[Antenatal corticosteroids]] to accelerate fetal lung maturation | |||
* Early use of [[surfactant]] therapy | |||
* Minimizing invasive ventilation using [[CPAP]] or [[NIPPV]] | |||
* Targeted oxygen saturation goals to reduce oxygen toxicity | |||
* Infection control and nutritional support | |||
== See also == | == See also == | ||
* [[ | * [[Premature birth]] | ||
* [[ | * [[Respiratory distress syndrome]] | ||
* [[Pulmonary fibrosis]] | |||
* [[Patent ductus arteriosus]] | |||
* [[Pediatric pulmonology]] | |||
* [[Neonatal intensive care unit]] | |||
* | |||
* [ | |||
== External links == | == External links == | ||
* [https://www.nhlbi.nih.gov/health-topics/bronchopulmonary-dysplasia NHLBI – Bronchopulmonary Dysplasia] | |||
* [https://www.nichd.nih.gov/health/topics/bpd NICHD – Bronchopulmonary Dysplasia Overview] | |||
{{Certain conditions originating in the perinatal period}} | |||
{{Respiratory diseases}} | |||
{{Neonatology}} | |||
{{Stub}} | |||
}} | |||
{{ | |||
[[Category:Bronchus disorders]] | [[Category:Bronchus disorders]] | ||
[[Category:Neonatology]] | [[Category:Neonatology]] | ||
[[Category:Rare diseases]] | |||
[[Category:Respiratory diseases]] | |||
[[Category:Pediatrics]] | |||
[[Category:Lung disorders]] | |||
[[Category:Conditions diagnosed in infancy]] | |||
Latest revision as of 19:37, 4 April 2025

Editor-In-Chief: Prab R Tumpati, MD
Obesity, Sleep & Internal medicine
Founder, WikiMD Wellnesspedia &
W8MD's medical weight loss NYC, sleep center NYC
Philadelphia medical weight loss and Philadelphia sleep clinics
| Bronchopulmonary dysplasia | |
|---|---|
| |
| Synonyms | Chronic lung disease of prematurity |
| Pronounce | N/A |
| Specialty | N/A |
| Symptoms | Tachypnea, retractions, hypoxemia, cyanosis |
| Complications | Pulmonary hypertension, growth failure, neurodevelopmental impairment |
| Onset | Usually in premature infants |
| Duration | Can be chronic |
| Types | N/A |
| Causes | Premature birth, mechanical ventilation, oxygen toxicity |
| Risks | Prematurity, low birth weight, prolonged mechanical ventilation |
| Diagnosis | Chest X-ray, clinical evaluation |
| Differential diagnosis | Respiratory distress syndrome, pneumonia, congenital heart disease |
| Prevention | Antenatal steroids, surfactant therapy, gentle ventilation strategies |
| Treatment | Oxygen therapy, diuretics, bronchodilators, nutritional support |
| Medication | N/A |
| Prognosis | Variable; some improve with age, others may have long-term complications |
| Frequency | Affects a significant number of very low birth weight infants |
| Deaths | N/A |
A chronic lung disease affecting premature infants
| Bronchopulmonary dysplasia | |
|---|---|
| |
| Synonyms | BPD |
| Pronounce | |
| Field | Pulmonology, Neonatology |
| Symptoms | Tachypnea, retractions, hypoxemia, need for prolonged oxygen therapy |
| Complications | Pulmonary hypertension, growth failure, recurrent respiratory infections |
| Onset | Typically within the first 4 weeks of life |
| Duration | Chronic; may persist into childhood |
| Types | Mild, moderate, severe (based on oxygen requirement at 36 weeks postmenstrual age) |
| Causes | Lung injury from mechanical ventilation and/or oxygen therapy |
| Risks | Prematurity, low birth weight, infection, PDA, high oxygen exposure |
| Diagnosis | Clinical criteria, oxygen requirement at 28 days and 36 weeks PMA, chest X-ray |
| Differential diagnosis | Respiratory distress syndrome, congenital pneumonia, pulmonary hypoplasia |
| Prevention | Antenatal corticosteroids, non-invasive ventilation, surfactant therapy |
| Treatment | Respiratory support, nutrition, bronchodilators, diuretics, corticosteroids |
| Medication | Albuterol, furosemide, dexamethasone |
| Prognosis | Variable; some resolve over time, others have long-term respiratory issues |
| Frequency | ~10,000–15,000 cases/year in the U.S. |
| Deaths | Associated with severity; improved survival with neonatal care advances |
Bronchopulmonary dysplasia (BPD) is a chronic lung disease that primarily affects premature infants who have received mechanical ventilation or supplemental oxygen therapy to treat respiratory distress syndrome (RDS). It is characterized by abnormal development of the alveoli, inflammation, and pulmonary fibrosis, leading to long-term respiratory difficulties.
History[edit]
The term "bronchopulmonary dysplasia" was first described in 1967 by Dr. William Northway to characterize the chronic lung damage observed in premature infants treated with high levels of oxygen and prolonged mechanical ventilation. Advances in neonatal intensive care have since altered the presentation and understanding of BPD, shifting from scarring to more developmental arrest in alveolarization.
Pathophysiology[edit]
BPD results from a combination of factors that injure the immature lungs, including:
- Barotrauma from mechanical ventilation
- Oxygen toxicity from high inspired oxygen concentrations
- Inflammatory responses to infection or ventilation
- Poor postnatal nutrition
These injuries disrupt the normal development of alveoli and pulmonary vasculature. The lungs of infants with BPD show fewer, larger alveoli with thickened septa, impaired gas exchange, and increased airway resistance.
Risk Factors[edit]
Risk factors for developing BPD include:
- Extreme prematurity (especially <28 weeks gestation)
- Very low birth weight (<1500g)
- Prolonged requirement for positive pressure ventilation
- High concentrations of inspired oxygen
- Prenatal or postnatal infections (e.g., chorioamnionitis, sepsis)
- Patent ductus arteriosus (PDA)
- Genetic susceptibility and intrauterine growth restriction (IUGR)
Clinical Presentation[edit]
Signs and symptoms may include:
- Persistent tachypnea and retractions
- Difficulty weaning from respiratory support
- Poor feeding and failure to thrive
- Need for supplemental oxygen beyond 28 days of life
- Recurrent respiratory infections
- Signs of pulmonary hypertension in severe cases
Diagnosis[edit]
BPD is diagnosed based on:
- The need for oxygen supplementation at 28 days of life and at 36 weeks postmenstrual age (PMA)
- Severity classification (mild, moderate, severe) depends on oxygen dependency and respiratory support at 36 weeks PMA or 56 days of life
- Chest X-ray may show areas of:
- Atelectasis
- Hyperinflation
- Linear opacities or cystic changes
- Pulmonary function testing and echocardiography may aid in assessment
Management[edit]
Management of BPD involves a multidisciplinary approach:
- Respiratory support: Minimize further lung injury using non-invasive methods like CPAP or nasal cannula when possible
- Pharmacologic therapy:
- Bronchodilators (e.g., albuterol)
- Diuretics (e.g., furosemide) to reduce pulmonary edema
- Corticosteroids (e.g., dexamethasone or hydrocortisone) in select cases
- Nutrition: High-calorie feeds and possible gastrostomy to support growth and healing
- Treatment of complications: Monitor for and manage pulmonary hypertension, tracheomalacia, and infections
Complications[edit]
Long-term complications of BPD may include:
- Chronic obstructive lung disease in childhood
- Asthma-like symptoms
- Recurrent bronchiolitis or pneumonia
- Need for home oxygen or tracheostomy in severe cases
- Neurodevelopmental delay due to prolonged NICU stay
Prognosis[edit]
Prognosis depends on:
- Degree of prematurity
- Severity of lung damage
- Presence of comorbidities
With modern neonatal care, survival rates have improved, and many infants recover lung function over time. However, some children continue to have respiratory and developmental issues into adolescence.
Prevention[edit]
Preventive measures include:
- Antenatal corticosteroids to accelerate fetal lung maturation
- Early use of surfactant therapy
- Minimizing invasive ventilation using CPAP or NIPPV
- Targeted oxygen saturation goals to reduce oxygen toxicity
- Infection control and nutritional support
See also[edit]
- Premature birth
- Respiratory distress syndrome
- Pulmonary fibrosis
- Patent ductus arteriosus
- Pediatric pulmonology
- Neonatal intensive care unit
External links[edit]
| Conditions originating in the perinatal period / fetal disease | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| Respiratory diseases | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
This respiratory disease-related article is a stub.
|
| Neonatology | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
This Neonatology related article is a stub.
|


