Brugada syndrome: Difference between revisions
CSV import |
CSV import |
||
| Line 47: | Line 47: | ||
[[Category:Genetic disorders with OMIM but no gene]] | [[Category:Genetic disorders with OMIM but no gene]] | ||
[[Category:Rare diseases]] | [[Category:Rare diseases]] | ||
<gallery> | |||
File:Brugada syndrome ECGs.jpg|Brugada syndrome ECGs | |||
File:Wavebreak and re-entry as a mechanism of arrhythmias.png|Wavebreak and re-entry as a mechanism of arrhythmias | |||
File:Brugada.jpg|Brugada | |||
File:Brugada syndrome type1 example1 (CardioNetworks ECGpedia).png|Brugada syndrome type 1 example 1 | |||
File:Brugada syndrome type2 example1 (CardioNetworks ECGpedia).png|Brugada syndrome type 2 example 1 | |||
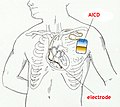
File:AICD.jpg|AICD | |||
</gallery> | |||
Revision as of 00:49, 20 February 2025
Brugada Syndrome
Brugada syndrome is a genetic disorder that results in abnormal electrical activity within the heart, leading to an increased risk of sudden cardiac death. It is characterized by a specific pattern on an electrocardiogram (ECG) and is often associated with ventricular fibrillation.
Epidemiology
Brugada syndrome is more prevalent in certain populations, particularly in Southeast Asia. It is estimated to affect 1 in 2,000 people worldwide. The condition is more common in males than females, with a male-to-female ratio of approximately 8:1.
Genetics
Brugada syndrome is primarily inherited in an autosomal dominant manner. Mutations in the SCN5A gene, which encodes the cardiac sodium channel, are the most common genetic cause. However, mutations in other genes such as CACNA1C, CACNB2, and SCN1B have also been implicated.
Pathophysiology
The hallmark of Brugada syndrome is the disruption of the normal electrical activity of the heart, particularly in the right ventricular outflow tract. This disruption is often due to a loss of function in the sodium channels, leading to a predisposition to ventricular arrhythmias.
Clinical Presentation
Patients with Brugada syndrome may be asymptomatic or present with symptoms such as:
- Syncope
- Palpitations
- Sudden cardiac arrest
The condition is often diagnosed after a family member experiences sudden cardiac death or during an evaluation for syncope.
Diagnosis
The diagnosis of Brugada syndrome is primarily based on the characteristic ECG findings, which include:
- Coved-type ST-segment elevation in the right precordial leads (V1-V3)
A provocative test with sodium channel blockers such as ajmaline or flecainide may be used to unmask the ECG pattern in suspected cases.
Management
The management of Brugada syndrome focuses on preventing sudden cardiac death. Treatment options include:
- Implantable cardioverter-defibrillator (ICD) for high-risk patients
- Avoidance of drugs that can exacerbate the condition
- Lifestyle modifications, such as avoiding excessive alcohol and fever management
Prognosis
The prognosis of Brugada syndrome varies depending on the presence of symptoms and the risk of arrhythmias. Asymptomatic individuals with a normal ECG have a lower risk of sudden cardiac death compared to those with a history of syncope or documented ventricular arrhythmias.
See Also
External Links
- [Brugada Syndrome Foundation](https://www.brugada.org)
Cardiovascular disease A-Z
Most common cardiac diseases
- Cardiac arrhythmia
- Cardiogenetic disorders
- Cardiomegaly
- Cardiomyopathy
- Cardiopulmonary resuscitation
- Chronic rheumatic heart diseases
- Congenital heart defects
- Heart neoplasia
- Ischemic heart diseases
- Pericardial disorders
- Syndromes affecting the heart
- Valvular heart disease
A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z
A
- Accelerated idioventricular rhythm
- Acute decompensated heart failure
- Arteriosclerotic heart disease
- Athletic heart syndrome
- Atrial flutter
- Atrioventricular fistula
- Cardiovascular disease in Australia
- Autoimmune heart disease
B
C
- Ebb Cade
- Cardiac allograft vasculopathy
- Cardiac amyloidosis
- Cardiac asthma
- Cardiac tamponade
- Cardiogenic shock
- Cardiogeriatrics
- Cardiorenal syndrome
- Cardiotoxicity
- Carditis
- Coronary artery aneurysm
- Coronary artery anomaly
- Coronary artery disease
- Spontaneous coronary artery dissection
- Coronary artery ectasia
- Coronary occlusion
- Coronary steal
- Coronary thrombosis
- Coronary vasospasm
- Cœur en sabot
- Coxsackievirus-induced cardiomyopathy
D
E
H
- Heart attack
- Heart failure
- Heart failure with preserved ejection fraction
- Heart to Heart (1949 film)
- High-output heart failure
- Hyperdynamic precordium
A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z
I
- Idiopathic giant-cell myocarditis
- Interventricular dyssynchrony
- Intraventricular dyssynchrony
- Isolated atrial amyloidosis
K
L
M
- Mydicar
- Myocardial bridge
- Myocardial disarray
- Myocardial rupture
- Myocardial scarring
- Myocardial stunning
- Myocarditis
N
O
P
- Papillary fibroelastoma
- Pathophysiology of heart failure
- Postpericardiotomy syndrome
- Pulmonary vein stenosis
R
S
- Saturated fat and cardiovascular disease
- SCAR-Fc
- Shone's syndrome
- Strain pattern
- Subacute bacterial endocarditis
- Sudden cardiac death of athletes
A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z
T
V
W
| Genetic disorders relating to deficiencies of transcription factor or coregulators | ||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
-
Brugada syndrome ECGs
-
Wavebreak and re-entry as a mechanism of arrhythmias
-
Brugada
-
Brugada syndrome type 1 example 1
-
Brugada syndrome type 2 example 1
-
AICD