Duodenal cancer

Editor-In-Chief: Prab R Tumpati, MD
Obesity, Sleep & Internal medicine
Founder, WikiMD Wellnesspedia &
W8MD's medical weight loss NYC, sleep center NYC
Philadelphia medical weight loss and Philadelphia sleep clinics
| Duodenal cancer | |
|---|---|
| |
| Synonyms | N/A |
| Pronounce | N/A |
| Specialty | N/A |
| Symptoms | Abdominal pain, nausea, vomiting, weight loss, jaundice |
| Complications | Bowel obstruction, metastasis |
| Onset | Typically in adulthood |
| Duration | Variable |
| Types | Adenocarcinoma, sarcoma, neuroendocrine tumor, lymphoma |
| Causes | Genetic mutations, familial adenomatous polyposis, Lynch syndrome |
| Risks | Smoking, alcohol consumption, diet, family history |
| Diagnosis | Endoscopy, biopsy, CT scan, MRI |
| Differential diagnosis | Peptic ulcer disease, Crohn's disease, pancreatic cancer |
| Prevention | Healthy diet, regular screening for high-risk individuals |
| Treatment | Surgery, chemotherapy, radiation therapy |
| Medication | N/A |
| Prognosis | Depends on stage at diagnosis |
| Frequency | Rare |
| Deaths | N/A |
Duodenal cancer is a rare but serious health condition characterized by the development of malignant cells in the duodenum, the first part of the small intestine.
Types[edit]
Duodenal cancers are generally classified by their histology, or cell type. The vast majority of duodenal cancers are adenocarcinomas, which originate from the glandular cells lining the duodenum. Other types, such as sarcomas, lymphomas, and carcinoid tumors, are far less common.
Etiology[edit]
The exact cause of duodenal cancer is unknown, but several risk factors have been identified. These include:
- Age: Duodenal cancer is more common in older individuals, typically occurring after the age of 50.
- Gender: Men are slightly more likely to develop duodenal cancer than women.
- Family history: Individuals with a family history of gastrointestinal cancers may have an increased risk.
- Genetic syndromes: Certain inherited conditions, like familial adenomatous polyposis (FAP) or Lynch syndrome, are associated with a higher risk of duodenal cancer.
- Chronic inflammation: Conditions like celiac disease or Crohn's disease, which cause chronic inflammation in the small intestine, may increase the risk.
- Helicobacter pylori infection: Infection with this bacterium, which is also linked to stomach ulcers and cancer, may increase risk.
Symptoms[edit]
Symptoms of duodenal cancer can be non-specific and often mirror other gastrointestinal disorders. They may include:
- Abdominal pain or discomfort
- Nausea and vomiting
- Weight loss
- Loss of appetite
- Fatigue
- Anemia
- Jaundice (yellowing of the skin and eyes) if the tumor blocks the bile duct
- Melena (black, tarry stools) or hematochezia (bright red blood in stools) indicating gastrointestinal bleeding
Diagnosis[edit]
Diagnosing duodenal cancer typically involves a combination of the following:
- Medical history and physical examination: The doctor will take a detailed medical history and perform a physical examination.
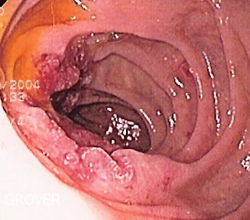
- Endoscopy: An upper endoscopy allows the physician to visually examine the duodenum using a flexible tube with a light and camera.
- Biopsy: Tissue samples collected during endoscopy can be examined under a microscope to confirm the diagnosis.
- Imaging studies: Techniques such as computed tomography (CT), magnetic resonance imaging (MRI), or positron emission tomography (PET) scans may be used to determine the extent of the disease and whether it has spread (metastasized).
Treatment[edit]
Treatment options for duodenal cancer depend on the stage of the disease, the patient's overall health, and personal preferences. They may include:
- Surgery: The mainstay of treatment for localized duodenal cancer is surgical removal of the tumor. This may involve a partial or total duodenectomy, or pancreaticoduodenectomy (Whipple procedure) in more advanced cases.
- Chemotherapy: Chemotherapy may be used before surgery to shrink tumors, after surgery to kill remaining cancer cells, or as the main treatment for advanced or metastatic duodenal cancer.
- Radiation therapy: Radiation may be used in conjunction with surgery and chemotherapy, particularly in advanced cases.
- Targeted therapy: For some types of duodenal cancer, targeted drug treatments may be available that attack specific abnormalities in cancer cells.
Prognosis[edit]
The prognosis for duodenal cancer depends on several factors, including the stage of the disease at diagnosis, the patient's overall health, the type of cancer, and the response to treatment. Early-stage duodenal cancer that is confined to the duodenum has a better prognosis than cancer that has spread to nearby lymph nodes or distant organs. Unfortunately, due to the non-specific symptoms of duodenal cancer, many cases are diagnosed at later stages when the disease is more advanced.
Epidemiology[edit]
Duodenal cancer is a relatively rare form of cancer. It accounts for only about 0.3% of all new cancer cases in the United States. However, it is the most common type of small intestine cancer. Its incidence seems to be slightly higher in men than in women, and it is more frequently diagnosed in older individuals.
Research[edit]
Given the relative rarity of duodenal cancer, it has been under-studied compared to other cancers. However, current research efforts are focused on understanding the genetic changes that lead to the development of duodenal cancer, improving early detection methods, and developing new treatment strategies. Clinical trials are ongoing to evaluate new chemotherapy regimens, targeted therapies, and immunotherapies.
External links[edit]
- National Cancer Institute: Small Intestine Cancer Treatment (PDQ¬Æ)–Patient Version
- American Cancer Society: Small Intestine Cancer
|
|
|
| Health science - Medicine - Gastroenterology - edit |
|---|
| Diseases of the esophagus - stomach |
| Halitosis | Nausea | Vomiting | GERD | Achalasia | Esophageal cancer | Esophageal varices | Peptic ulcer | Abdominal pain | Stomach cancer | Functional dyspepsia | Gastroparesis |
| Diseases of the liver - pancreas - gallbladder - biliary tree |
| Hepatitis | Cirrhosis | NASH | PBC | PSC | Budd-Chiari | Hepatocellular carcinoma | Acute pancreatitis | Chronic pancreatitis | Pancreatic cancer | Gallstones | Cholecystitis |
| Diseases of the small intestine |
| Peptic ulcer | Intussusception | Malabsorption (e.g. Coeliac, lactose intolerance, fructose malabsorption, Whipple's) | Lymphoma |
| Diseases of the colon |
| Diarrhea | Appendicitis | Diverticulitis | Diverticulosis | IBD (Crohn's, Ulcerative colitis) | IBS | Constipation | Colorectal cancer | Hirschsprung's | Pseudomembranous colitis |
Ad. Transform your life with W8MD's Budget GLP-1 injections from $49.99


W8MD offers a medical weight loss program to lose weight in Philadelphia. Our physician-supervised medical weight loss provides:
- Weight loss injections in NYC (generic and brand names):
- Zepbound / Mounjaro, Wegovy / Ozempic, Saxenda
- Most insurances accepted or discounted self-pay rates. We will obtain insurance prior authorizations if needed.
- Generic GLP1 weight loss injections from $49.99 for the starting dose of Semaglutide and $65.00 for Tirzepatide.
- Also offer prescription weight loss medications including Phentermine, Qsymia, Diethylpropion, Contrave etc.
NYC weight loss doctor appointmentsNYC weight loss doctor appointments
Start your NYC weight loss journey today at our NYC medical weight loss and Philadelphia medical weight loss clinics.
- Call 718-946-5500 to lose weight in NYC or for medical weight loss in Philadelphia 215-676-2334.
- Tags:NYC medical weight loss, Philadelphia lose weight Zepbound NYC, Budget GLP1 weight loss injections, Wegovy Philadelphia, Wegovy NYC, Philadelphia medical weight loss, Brookly weight loss and Wegovy NYC
Error creating thumbnail: Error creating thumbnail: ![]()
![]()
|
WikiMD's Wellness Encyclopedia |
| Let Food Be Thy Medicine Medicine Thy Food - Hippocrates |
Medical Disclaimer: WikiMD is not a substitute for professional medical advice. The information on WikiMD is provided as an information resource only, may be incorrect, outdated or misleading, and is not to be used or relied on for any diagnostic or treatment purposes. Please consult your health care provider before making any healthcare decisions or for guidance about a specific medical condition. WikiMD expressly disclaims responsibility, and shall have no liability, for any damages, loss, injury, or liability whatsoever suffered as a result of your reliance on the information contained in this site. By visiting this site you agree to the foregoing terms and conditions, which may from time to time be changed or supplemented by WikiMD. If you do not agree to the foregoing terms and conditions, you should not enter or use this site. See full disclaimer.
Credits:Most images are courtesy of Wikimedia commons, and templates, categories Wikipedia, licensed under CC BY SA or similar.
Translate this page: - East Asian
中文,
日本,
한국어,
South Asian
हिन्दी,
தமிழ்,
తెలుగు,
Urdu,
ಕನ್ನಡ,
Southeast Asian
Indonesian,
Vietnamese,
Thai,
မြန်မာဘာသာ,
বাংলা
European
español,
Deutsch,
français,
Greek,
português do Brasil,
polski,
română,
русский,
Nederlands,
norsk,
svenska,
suomi,
Italian
Middle Eastern & African
عربى,
Turkish,
Persian,
Hebrew,
Afrikaans,
isiZulu,
Kiswahili,
Other
Bulgarian,
Hungarian,
Czech,
Swedish,
മലയാളം,
मराठी,
ਪੰਜਾਬੀ,
ગુજરાતી,
Portuguese,
Ukrainian

