Bronchopulmonary dysplasia
Bronchopulmonary dysplasia (BPD; formerly chronic lung disease of infancy) is a chronic lung disease in which premature infants, usually those who were treated with supplemental oxygen, require long-term oxygen.<ref>Merck Manual, Professional Edition, Bronchopulmonary Dysplasia (BPD).</ref>The alveoli that are present tend to not be mature enough to function normal.<ref>
Bronchopulmonary Dysplasia(link). American Lung Association.
Accessed 2020-03-12.
</ref> It is more common in infants with low birth weight (LBW) and those who receive prolonged mechanical ventilation to treat respiratory distress syndrome (RDS). It results in significant morbidity and mortality. The definition of BPD has continued to evolve primarily due to changes in the population, such as more survivors at earlier gestational ages, and improved neonatal management including surfactant, antenatal glucocorticoid therapy, and less aggressive mechanical ventilation.<ref name="pmid5334613">Northway Jr, WH,
Pulmonary disease following respirator therapy of hyaline-membrane disease. Bronchopulmonary dysplasia., The New England Journal of Medicine, Vol. 276(Issue: 7), pp. 357–68, DOI: 10.1056/NEJM196702162760701, PMID: 5334613,</ref>
Currently the description of BPD includes the grading of its severity into mild, moderate and severe. This correlates with the infant's maturity, growth and overall severity of illness.<ref name="pmid15538399">Sahni, R,
Is the new definition of bronchopulmonary dysplasia more useful?, Journal of Perinatology, Vol. 25(Issue: 1), pp. 41–6, DOI: 10.1038/sj.jp.7211210, PMID: 15538399,</ref> The new system offers a better description of underlying pulmonary disease and its severity.<ref name="pmid16322158">Ehrenkranz, RA, Validation of the National Institutes of Health consensus definition of bronchopulmonary dysplasia, Pediatrics, Vol. 116(Issue: 6), pp. 1353–60, DOI: 10.1542/peds.2005-0249, PMID: 16322158,</ref>
Presentation
Complications
Feeding problems are common in infants with BPD, often due to prolonged intubation. Such infants often display oral-tactile hypersensitivity (also known as oral aversion).<ref>Gaining & Growing. "Bronchopulmonary dysplasia", Gaining & Growing, March 20, 2007. (Retrieved June 12, 2008.)</ref> Physical findings:
- hypoxemia;
- hypercapnia;
- crackles, wheezing, & decreased breath sounds;
- increased bronchial secretions;
- hyperinflation;
- frequent lower respiratory infections;
- delayed growth & development;
- cor pulmonale;
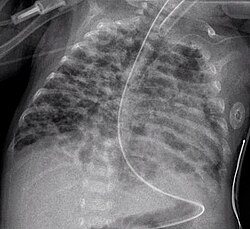
- CXR shows with hyperinflation, low diaphragm, atelectasis, cystic changes.
Cause
Prolonged high oxygen delivery in premature infants causes necrotizing bronchiolitis and alveolar septal injury, with inflammation and scarring. This results in hypoxemia. Today, with the advent of surfactant therapy and high frequency ventilation and oxygen supplementation, infants with BPD experience much milder injury without necrotizing bronchiolitis or alveolar septal fibrosis. Instead, there are usually uniformly dilated acini with thin alveolar septa and little or no interstitial fibrosis. It develops most commonly in the first 4 weeks after birth.
Diagnosis
Earlier criteria
The classic diagnosis of BPD may be assigned at 28 days of life if the following criteria are met:
- Positive pressure ventilation during the first 2 weeks of life for a minimum of 3 days.
- Clinical signs of abnormal respiratory function.
- Requirements for supplemental oxygen for longer than 28 days of age to maintain PaO2 above 50 mm Hg.
- Chest radiograph with diffuse abnormal findings characteristic of BPD.
Newer criteria
The newer National Institute of Health (US) criteria for BPD (for neonates treated with more than 21% oxygen for at least 28 days)<ref name="pmid16650652">Kinsella, JP,
Bronchopulmonary dysplasia, Lancet, Vol. 367(Issue: 9520), pp. 1421–31, DOI: 10.1016/S0140-6736(06)68615-7, PMID: 16650652,</ref> is as follows:,<ref>
Bronchopulmonary Dysplasia(link). {{{website}}}.
</ref><ref>,
Bronchopulmonary dysplasia, Am J Respir Crit Care Med, Vol. 163(Issue: 7), pp. 1723–9, DOI: 10.1164/ajrccm.163.7.2011060, PMID: 11401896,</ref>
- Mild
- Breathing room air at 36 weeks' post-menstrual age or discharge (whichever comes first) for babies born before 32 weeks, or
- breathing room air by 56 days' postnatal age, or discharge (whichever comes first) for babies born after 32 weeks' gestation.
- Moderate
- Need for <30% oxygen at 36 weeks' postmenstrual age, or discharge (whichever comes first) for babies born before 32 weeks, or
- need for <30% oxygen to 56 days' postnatal age, or discharge (whichever comes first) for babies born after 32 weeks' gestation.
- Severe
- Need for >30% oxygen, with or without positive pressure ventilation or continuous positive pressure at 36 weeks' postmenstrual age, or discharge (whichever comes first) for babies born before 32 weeks, or
- need for >30% oxygen with or without positive pressure ventilation or continuous positive pressure at 56 days' postnatal age, or discharge (whichever comes first) for babies born after 32 weeks' gestation.
Management
There is evidence to show that steroids given to babies less than 8 days old can prevent bronchopulmonary dysplasia.<ref name=":0">Doyle, Lex W,
Early (< 8 days) systemic postnatal corticosteroids for prevention of bronchopulmonary dysplasia in preterm infants, Cochrane Database of Systematic Reviews, Vol. 10, pp. CD001146, DOI: 10.1002/14651858.cd001146.pub5, PMID: 29063585, PMC: 6485683,</ref> However, the risks of neurodevelopmental sequelae may outweigh the benefits.<ref name=":0" /> It is unclear if starting steroids more than 7 days after birth is harmful or beneficial.<ref name=":1">Doyle, Lex W, Late (> 7 days) systemic postnatal corticosteroids for prevention of bronchopulmonary dysplasia in preterm infants, Cochrane Database of Systematic Reviews, Vol. 10, pp. CD001145, DOI: 10.1002/14651858.cd001145.pub4, PMID: 29063594, PMC: 6485440,</ref> It is thus recommended that they only be used in those who cannot be taken off of a ventilator.<ref name=":1" /> Evidence suggests that vitamin A in LBW babies is associated with a reduction in mortality and bronchopulmonary dysplasia.<ref>Guimarães, Hercília, Vitamin A in prevention of bronchopulmonary dysplasia, Current Pharmaceutical Design, Vol. 18(Issue: 21), pp. 3101–3113, DOI: 10.2174/1381612811209023101, PMID: 22564302,</ref>
Oxygen therapy at home is recommended in those with significant low oxygen levels.<ref>,
Home Oxygen Therapy for Children. An Official American Thoracic Society Clinical Practice Guideline., American Journal of Respiratory and Critical Care Medicine, Vol. 199(Issue: 3), pp. e5–e23, DOI: 10.1164/rccm.201812-2276ST, PMID: 30707039, PMC: 6802853,</ref>
Epidemiology
The rate of BPD varies among institutions, which may reflect neonatal risk factors, care practices (e.g., target levels for acceptable oxygen saturation), and differences in the clinical definitions of BPD.<ref name="pmid17306659">,
Trends in neonatal morbidity and mortality for very low birthweight infants, Am J Obstet Gynecol, 2007, Vol. 196(Issue: 2), pp. 147.e1–8, DOI: 10.1016/j.ajog.2006.09.014, PMID: 17306659,</ref><ref name="pmid10835057">, Do clinical markers of barotrauma and oxygen toxicity explain interhospital variation in rates of chronic lung disease? The Neonatology Committee for the Developmental Network, Pediatrics, 2000, Vol. 105(Issue: 6), pp. 1194–201, DOI: 10.1542/peds.105.6.1194, PMID: 10835057,</ref><ref name="pmid14726936">, Controversy surrounding the use of home oxygen for premature infants with bronchopulmonary dysplasia, J Perinatol, 2004, Vol. 24(Issue: 1), pp. 36–40, DOI: 10.1038/sj.jp.7211012, PMID: 14726936,</ref>
See also
References
<references group="" responsive="1"></references>
Further reading
- Bhandari, A,
Bronchopulmonary dysplasia: an update, Indian Journal of Pediatrics, Vol. 74(Issue: 1), pp. 73–7, DOI: 10.1007/s12098-007-0032-z, PMID: 17264460, Full text,
- Bronchopulmonary Dysplasia on National Institutes of Health
External links
| Conditions originating in the perinatal period / fetal disease | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
Bronchopulmonary dysplasia
-
Chest X-ray showing bronchopulmonary dysplasia
Ad. Transform your life with W8MD's Budget GLP-1 injections from $49.99


W8MD offers a medical weight loss program to lose weight in Philadelphia. Our physician-supervised medical weight loss provides:
- Weight loss injections in NYC (generic and brand names):
- Zepbound / Mounjaro, Wegovy / Ozempic, Saxenda
- Most insurances accepted or discounted self-pay rates. We will obtain insurance prior authorizations if needed.
- Generic GLP1 weight loss injections from $49.99 for the starting dose of Semaglutide and $65.00 for Tirzepatide.
- Also offer prescription weight loss medications including Phentermine, Qsymia, Diethylpropion, Contrave etc.
NYC weight loss doctor appointmentsNYC weight loss doctor appointments
Start your NYC weight loss journey today at our NYC medical weight loss and Philadelphia medical weight loss clinics.
- Call 718-946-5500 to lose weight in NYC or for medical weight loss in Philadelphia 215-676-2334.
- Tags:NYC medical weight loss, Philadelphia lose weight Zepbound NYC, Budget GLP1 weight loss injections, Wegovy Philadelphia, Wegovy NYC, Philadelphia medical weight loss, Brookly weight loss and Wegovy NYC
|
WikiMD's Wellness Encyclopedia |
| Let Food Be Thy Medicine Medicine Thy Food - Hippocrates |
Medical Disclaimer: WikiMD is not a substitute for professional medical advice. The information on WikiMD is provided as an information resource only, may be incorrect, outdated or misleading, and is not to be used or relied on for any diagnostic or treatment purposes. Please consult your health care provider before making any healthcare decisions or for guidance about a specific medical condition. WikiMD expressly disclaims responsibility, and shall have no liability, for any damages, loss, injury, or liability whatsoever suffered as a result of your reliance on the information contained in this site. By visiting this site you agree to the foregoing terms and conditions, which may from time to time be changed or supplemented by WikiMD. If you do not agree to the foregoing terms and conditions, you should not enter or use this site. See full disclaimer.
Credits:Most images are courtesy of Wikimedia commons, and templates, categories Wikipedia, licensed under CC BY SA or similar.
Translate this page: - East Asian
中文,
日本,
한국어,
South Asian
हिन्दी,
தமிழ்,
తెలుగు,
Urdu,
ಕನ್ನಡ,
Southeast Asian
Indonesian,
Vietnamese,
Thai,
မြန်မာဘာသာ,
বাংলা
European
español,
Deutsch,
français,
Greek,
português do Brasil,
polski,
română,
русский,
Nederlands,
norsk,
svenska,
suomi,
Italian
Middle Eastern & African
عربى,
Turkish,
Persian,
Hebrew,
Afrikaans,
isiZulu,
Kiswahili,
Other
Bulgarian,
Hungarian,
Czech,
Swedish,
മലയാളം,
मराठी,
ਪੰਜਾਬੀ,
ગુજરાતી,
Portuguese,
Ukrainian