Mixed Müllerian tumor: Difference between revisions
CSV import Tags: mobile edit mobile web edit |
No edit summary |
||
| Line 1: | Line 1: | ||
{{short description|Malignant tumor of the uterus, containing both carcinoma and sarcoma components}} | |||
{{Infobox medical condition (new) | {{Infobox medical condition (new) | ||
| name = Mixed Müllerian tumor | |||
| image = MalignantMixedMullerianTumor.JPG | |||
| caption = | |||
| field = [[Oncology]], [[gynecology]] | |||
| synonyms | | synonyms = Malignant mixed mesodermal tumor (MMMT) | ||
| specialty | | specialty = | ||
| symptoms | | symptoms = Abdominal pain, vaginal bleeding, pelvic mass, and possible gastrointestinal or urinary tract involvement due to metastasis | ||
| complications | | complications = Peritoneal dissemination, metastasis to lymph nodes, lung, and other organs | ||
| onset | | onset = Typically postmenopausal or in older women, though it can occur at any age | ||
| duration | | duration = Chronic; may progress to advanced stages if untreated | ||
| types | | types = Homologous, heterologous | ||
| causes | | causes = Genetic mutations, hormonal factors, environmental exposures (e.g., radiation, tamoxifen) | ||
| risks | | risks = Obesity, exogenous estrogen therapies, nulliparity, tamoxifen therapy, pelvic irradiation | ||
| diagnosis | | diagnosis = Histopathological examination, imaging (ultrasound, CT, MRI), biopsy | ||
| differential | | differential = Endometrial carcinoma, ovarian carcinoma, other uterine sarcomas | ||
| prevention | | prevention = No known prevention; early detection and regular gynecological screening | ||
| treatment | | treatment = Surgery (hysterectomy), chemotherapy (e.g., Ifosfamide), radiation therapy | ||
| medication | | medication = Chemotherapy agents (Ifosfamide, Cisplatin, Carboplatin), hormonal therapy | ||
| prognosis | | prognosis = Poor prognosis with low survival rates, influenced by stage and grade of the carcinoma | ||
| frequency | | frequency = Rare; accounts for 2-5% of all uterine cancers | ||
| deaths | | deaths = High mortality due to aggressive nature and late-stage diagnosis | ||
}} | }} | ||
'''Mixed Müllerian tumor''' (MMMT), also known as '''malignant mixed mesodermal tumor''', is a rare and aggressive cancer of the uterus that contains both epithelial (carcinomatous) and mesenchymal (sarcomatous) components. These tumors are often diagnosed in postmenopausal women and have a poor prognosis due to their aggressive nature. | |||
==Classification== | == Classification == | ||
MMMT is traditionally classified into two subtypes: | |||
* '''Homologous MMMT''': In which the sarcomatous component consists of tissues normally found in the uterus, such as endometrial, fibrous, and smooth muscle tissues. | |||
* '''Heterologous MMMT''': In which the sarcomatous component consists of tissues not normally found in the uterus, such as cartilage, bone, or skeletal muscle. | |||
The term "malignant mixed Müllerian tumor" was historically used to describe tumors with heterologous sarcomatous components, while "carcinosarcoma" was used to describe those with homologous components. However, "carcinosarcoma" is now the standard term, though "malignant mixed Müllerian tumor" remains widely used, especially in gynecological literature. | |||
== | == Pathophysiology == | ||
The tumor is thought to develop from a single stem cell line, which differentiates into both epithelial and mesenchymal components. The presence of these two distinct tissue types in one tumor mass has led to multiple theories regarding the origin of MMMT. The most accepted theory is the "combination theory," which suggests that the tumor originates from a single precursor cell that differentiates into both tissue types. Other theories include the "collision theory," where separate tumors collide, and the "composition theory," where the carcinoma induces the stroma to produce the sarcomatous component. | |||
In some cases, the epithelial portion of MMMTs behaves more aggressively and is primarily responsible for metastasis, while the sarcomatous component often remains confined to the primary site. | |||
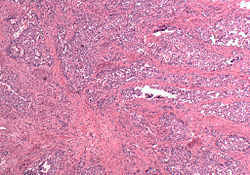
== Morphology == | |||
MMMTs tend to be bulkier and fleshier than other forms of uterine tumors, often appearing polypoid and sometimes protruding through the cervical os. On histological examination, MMMTs consist of adenocarcinoma (commonly endometrioid, serous, or clear cell) mixed with malignant mesenchymal elements. The sarcomatous components may also mimic extrauterine tissues such as cartilage, bone, and striated muscle. The tumors are often highly vascular and may invade surrounding tissues, including the serosa and adjacent organs. | |||
== | == Prognosis == | ||
The prognosis for MMMTs is generally poor due to their high malignancy. Survival rates are heavily dependent on the stage at diagnosis, with early-stage MMMTs having a better chance of survival. The 5-year survival rate for stage I MMMTs is around 50%, while the overall 5-year survival rate for all stages is less than 20%. Prognosis is further influenced by the grade of the carcinoma, with serous carcinoma having the worst prognosis. | |||
# Staging of MMMT: | |||
* '''Stage I''': Tumor confined to the corpus uteri. | |||
* '''Stage II''': Tumor involves both the corpus and cervix. | |||
* '''Stage III''': Tumor extends outside the uterus but remains within the lesser pelvis. | |||
* '''Stage IV''': Tumor extends outside the pelvis or involves the bladder or rectum mucosa. | |||
== Treatment == | |||
The primary treatment for MMMTs is surgical resection, typically involving a total hysterectomy (removal of the uterus) and bilateral salpingo-oophorectomy (removal of the ovaries and fallopian tubes). Surgical intervention is often followed by adjuvant chemotherapy, with the chemotherapy regimen typically including Ifosfamide and platinum-based agents like Cisplatin or Carboplatin. Radiation therapy may also be used in some cases, particularly in high-risk or advanced-stage MMMTs. | |||
Treatment for MMMT is often aggressive, given the tumor's high metastatic potential. The use of chemotherapy and radiation is controversial, but studies have shown improved outcomes for patients with advanced-stage disease when these treatments are combined. | |||
== Epidemiology == | |||
MMMTs are rare, accounting for 2-5% of all uterine cancers. They are predominantly diagnosed in postmenopausal women, with an average age of onset around 66 years. Risk factors for MMMTs overlap with those for other uterine malignancies, including obesity, exogenous estrogen therapy, and nulliparity. Radiation therapy and the use of tamoxifen have also been identified as potential risk factors for the development of MMMT. | |||
== Diagnosis == | |||
Diagnosis of MMMT is based on clinical presentation, imaging studies, and histopathological examination. Patients may present with symptoms such as abnormal vaginal bleeding, abdominal pain, or a pelvic mass. Imaging modalities such as ultrasound, CT, or MRI may be used to assess the extent of the tumor. A definitive diagnosis is made through biopsy and histological evaluation, which reveals the characteristic mixture of carcinoma and sarcoma. | |||
== Differential Diagnosis == | |||
The differential diagnosis for MMMT includes other uterine malignancies, particularly endometrial carcinoma, ovarian carcinoma, and other types of uterine sarcomas. Histological evaluation is crucial for distinguishing MMMT from these other entities. | |||
== Prevention == | |||
There is no known prevention for MMMTs, but early detection and regular gynecological screening can improve outcomes. Women at high risk, such as those with a history of radiation therapy or estrogen therapy, should be monitored more closely for uterine malignancies. | |||
== See also == | |||
* [[Uterine cancer]] | |||
* [[Carcinosarcoma]] | |||
* [[Endometrial carcinoma]] | |||
* [[Ovarian carcinoma]] | |||
* [[Gynecological malignancies]] | |||
== External links == | == External links == | ||
{{Medical resources | {{Medical resources | ||
| DiseasesDB = 34517 | |||
| ICD10 = C57.9 | |||
| ICD9 = 182.0 | |||
| OMIM = | |||
| MedlinePlus = | |||
| eMedicineSubj = | |||
| eMedicineTopic = | |||
| MeshID = | |||
}} | }} | ||
{{ | {{Cancer}} | ||
{{Female genital neoplasia}} | {{Female genital neoplasia}} | ||
{{DEFAULTSORT:Mixed Müllerian Tumor}} | |||
{{DEFAULTSORT:Mixed | |||
[[Category:Gynaecological neoplasia]] | [[Category:Gynaecological neoplasia]] | ||
[[Category:Uterine diseases]] | |||
[[Category:Malignant tumors]] | |||
[[Category:Cancer]] | |||
[[Category:Rare diseases]] | |||
Latest revision as of 21:40, 2 April 2025
Malignant tumor of the uterus, containing both carcinoma and sarcoma components
| Mixed Müllerian tumor | |
|---|---|
| |
| Synonyms | Malignant mixed mesodermal tumor (MMMT) |
| Pronounce | N/A |
| Field | Oncology, gynecology |
| Symptoms | Abdominal pain, vaginal bleeding, pelvic mass, and possible gastrointestinal or urinary tract involvement due to metastasis |
| Complications | Peritoneal dissemination, metastasis to lymph nodes, lung, and other organs |
| Onset | Typically postmenopausal or in older women, though it can occur at any age |
| Duration | Chronic; may progress to advanced stages if untreated |
| Types | Homologous, heterologous |
| Causes | Genetic mutations, hormonal factors, environmental exposures (e.g., radiation, tamoxifen) |
| Risks | Obesity, exogenous estrogen therapies, nulliparity, tamoxifen therapy, pelvic irradiation |
| Diagnosis | Histopathological examination, imaging (ultrasound, CT, MRI), biopsy |
| Differential diagnosis | Endometrial carcinoma, ovarian carcinoma, other uterine sarcomas |
| Prevention | No known prevention; early detection and regular gynecological screening |
| Treatment | Surgery (hysterectomy), chemotherapy (e.g., Ifosfamide), radiation therapy |
| Medication | Chemotherapy agents (Ifosfamide, Cisplatin, Carboplatin), hormonal therapy |
| Prognosis | Poor prognosis with low survival rates, influenced by stage and grade of the carcinoma |
| Frequency | Rare; accounts for 2-5% of all uterine cancers |
| Deaths | High mortality due to aggressive nature and late-stage diagnosis |
Mixed Müllerian tumor (MMMT), also known as malignant mixed mesodermal tumor, is a rare and aggressive cancer of the uterus that contains both epithelial (carcinomatous) and mesenchymal (sarcomatous) components. These tumors are often diagnosed in postmenopausal women and have a poor prognosis due to their aggressive nature.
Classification[edit]
MMMT is traditionally classified into two subtypes:
- Homologous MMMT: In which the sarcomatous component consists of tissues normally found in the uterus, such as endometrial, fibrous, and smooth muscle tissues.
- Heterologous MMMT: In which the sarcomatous component consists of tissues not normally found in the uterus, such as cartilage, bone, or skeletal muscle.
The term "malignant mixed Müllerian tumor" was historically used to describe tumors with heterologous sarcomatous components, while "carcinosarcoma" was used to describe those with homologous components. However, "carcinosarcoma" is now the standard term, though "malignant mixed Müllerian tumor" remains widely used, especially in gynecological literature.
Pathophysiology[edit]
The tumor is thought to develop from a single stem cell line, which differentiates into both epithelial and mesenchymal components. The presence of these two distinct tissue types in one tumor mass has led to multiple theories regarding the origin of MMMT. The most accepted theory is the "combination theory," which suggests that the tumor originates from a single precursor cell that differentiates into both tissue types. Other theories include the "collision theory," where separate tumors collide, and the "composition theory," where the carcinoma induces the stroma to produce the sarcomatous component.
In some cases, the epithelial portion of MMMTs behaves more aggressively and is primarily responsible for metastasis, while the sarcomatous component often remains confined to the primary site.
Morphology[edit]
MMMTs tend to be bulkier and fleshier than other forms of uterine tumors, often appearing polypoid and sometimes protruding through the cervical os. On histological examination, MMMTs consist of adenocarcinoma (commonly endometrioid, serous, or clear cell) mixed with malignant mesenchymal elements. The sarcomatous components may also mimic extrauterine tissues such as cartilage, bone, and striated muscle. The tumors are often highly vascular and may invade surrounding tissues, including the serosa and adjacent organs.
Prognosis[edit]
The prognosis for MMMTs is generally poor due to their high malignancy. Survival rates are heavily dependent on the stage at diagnosis, with early-stage MMMTs having a better chance of survival. The 5-year survival rate for stage I MMMTs is around 50%, while the overall 5-year survival rate for all stages is less than 20%. Prognosis is further influenced by the grade of the carcinoma, with serous carcinoma having the worst prognosis.
- Staging of MMMT:
- Stage I: Tumor confined to the corpus uteri.
- Stage II: Tumor involves both the corpus and cervix.
- Stage III: Tumor extends outside the uterus but remains within the lesser pelvis.
- Stage IV: Tumor extends outside the pelvis or involves the bladder or rectum mucosa.
Treatment[edit]
The primary treatment for MMMTs is surgical resection, typically involving a total hysterectomy (removal of the uterus) and bilateral salpingo-oophorectomy (removal of the ovaries and fallopian tubes). Surgical intervention is often followed by adjuvant chemotherapy, with the chemotherapy regimen typically including Ifosfamide and platinum-based agents like Cisplatin or Carboplatin. Radiation therapy may also be used in some cases, particularly in high-risk or advanced-stage MMMTs.
Treatment for MMMT is often aggressive, given the tumor's high metastatic potential. The use of chemotherapy and radiation is controversial, but studies have shown improved outcomes for patients with advanced-stage disease when these treatments are combined.
Epidemiology[edit]
MMMTs are rare, accounting for 2-5% of all uterine cancers. They are predominantly diagnosed in postmenopausal women, with an average age of onset around 66 years. Risk factors for MMMTs overlap with those for other uterine malignancies, including obesity, exogenous estrogen therapy, and nulliparity. Radiation therapy and the use of tamoxifen have also been identified as potential risk factors for the development of MMMT.
Diagnosis[edit]
Diagnosis of MMMT is based on clinical presentation, imaging studies, and histopathological examination. Patients may present with symptoms such as abnormal vaginal bleeding, abdominal pain, or a pelvic mass. Imaging modalities such as ultrasound, CT, or MRI may be used to assess the extent of the tumor. A definitive diagnosis is made through biopsy and histological evaluation, which reveals the characteristic mixture of carcinoma and sarcoma.
Differential Diagnosis[edit]
The differential diagnosis for MMMT includes other uterine malignancies, particularly endometrial carcinoma, ovarian carcinoma, and other types of uterine sarcomas. Histological evaluation is crucial for distinguishing MMMT from these other entities.
Prevention[edit]
There is no known prevention for MMMTs, but early detection and regular gynecological screening can improve outcomes. Women at high risk, such as those with a history of radiation therapy or estrogen therapy, should be monitored more closely for uterine malignancies.
See also[edit]
External links[edit]
| Overview of tumors, cancer and oncology (C00–D48, 140–239) | ||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| Tumors of the female urogenital system | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|