Pyruvate kinase deficiency: Difference between revisions
No edit summary Tag: visualeditor-wikitext |
CSV import |
||
| Line 1: | Line 1: | ||
{{SI}} | |||
{{Infobox medical condition | |||
| name = Pyruvate kinase deficiency | |||
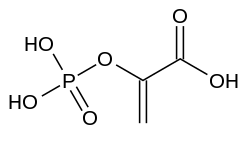
| image = [[File:Phosphoenolpyruvic_acid.svg|200px]] | |||
| caption = Phosphoenolpyruvic acid, a substrate of pyruvate kinase | |||
| field = [[Hematology]] | |||
| symptoms = [[Hemolytic anemia]], [[jaundice]], [[fatigue]], [[splenomegaly]] | |||
| complications = [[Gallstones]], [[iron overload]], [[heart failure]] | |||
| onset = [[Neonatal]] or [[childhood]] | |||
| duration = Lifelong | |||
| causes = [[Genetic mutation]] in the [[PKLR]] gene | |||
| risks = [[Autosomal recessive]] inheritance | |||
| diagnosis = [[Blood test]], [[genetic testing]] | |||
| differential = [[Hereditary spherocytosis]], [[G6PD deficiency]], [[thalassemia]] | |||
| treatment = [[Blood transfusion]], [[splenectomy]], [[folic acid]] supplementation | |||
| medication = None specific | |||
| prognosis = Variable, depending on severity | |||
| frequency = 1 in 20,000 people | |||
}} | |||
'''Other Names:''' Pyruvate kinase deficiency of red cells; Pyruvate kinase deficiency of erythrocytes; PK deficiency | '''Other Names:''' Pyruvate kinase deficiency of red cells; Pyruvate kinase deficiency of erythrocytes; PK deficiency | ||
Pyruvate kinase deficiency is a genetic blood disorder characterized by low levels of an enzyme called [[pyruvate kinase]], which is used by [[red blood cells]]. Without pyruvate kinase, red blood cells break down too easily, resulting in low levels of these cells ([[hemolytic anemia]]). | Pyruvate kinase deficiency is a genetic blood disorder characterized by low levels of an enzyme called [[pyruvate kinase]], which is used by [[red blood cells]]. Without pyruvate kinase, red blood cells break down too easily, resulting in low levels of these cells ([[hemolytic anemia]]). | ||
[[File:Pyruvate kinase.png|thumb]] | [[File:Pyruvate kinase.png|left|thumb]] | ||
<youtube> | <youtube> | ||
title='''{{PAGENAME}}''' | title='''{{PAGENAME}}''' | ||
| Line 13: | Line 31: | ||
height=600 | height=600 | ||
</youtube> | </youtube> | ||
== '''Epidemiology''' == | == '''Epidemiology''' == | ||
Pyruvate kinase deficiency is the most common inherited cause of nonspherocytic hemolytic anemia. More than 500 affected families have been identified, and studies suggest that the disorder may be underdiagnosed because mild cases may not be identified. | Pyruvate kinase deficiency is the most common inherited cause of nonspherocytic hemolytic anemia. More than 500 affected families have been identified, and studies suggest that the disorder may be underdiagnosed because mild cases may not be identified. | ||
Pyruvate kinase deficiency is found in all ethnic groups. Its prevalence has been estimated at 1 in 20,000 people of European descent. It is more common in the Old Order Amish population of Pennsylvania. | Pyruvate kinase deficiency is found in all ethnic groups. Its prevalence has been estimated at 1 in 20,000 people of European descent. It is more common in the Old Order Amish population of Pennsylvania. | ||
== '''Cause''' == | == '''Cause''' == | ||
[[File:Glycolysis regul muscle.png|thumb]] | [[File:Glycolysis regul muscle.png|left|thumb]] | ||
Pyruvate kinase deficiency is caused by mutations in the '''PKLR gene'''. The PKLR gene is active in the liver and in red blood cells, where it provides instructions for making an enzyme called [[pyruvate kinase]]. The pyruvate kinase enzyme is involved in a critical energy-producing process known as [[glycolysis]]. During glycolysis, the simple sugar glucose is broken down to produce [[adenosine triphosphate]] (ATP), the cell's main energy source. | Pyruvate kinase deficiency is caused by mutations in the '''PKLR gene'''. The PKLR gene is active in the liver and in red blood cells, where it provides instructions for making an enzyme called [[pyruvate kinase]]. The pyruvate kinase enzyme is involved in a critical energy-producing process known as [[glycolysis]]. During glycolysis, the simple sugar glucose is broken down to produce [[adenosine triphosphate]] (ATP), the cell's main energy source. | ||
PKLR gene mutations result in '''reduced pyruvate kinase enzyme function''', causing a '''shortage of ATP in red blood cells''' and increased levels of other molecules produced earlier in the glycolysis process. The abnormal red blood cells are gathered up by the spleen and destroyed, causing [[hemolytic anemia]] and an enlarged spleen. A shortage of red blood cells to carry oxygen throughout the body leads to fatigue, pallor, and shortness of breath. Iron and a molecule called [[bilirubin]] are released when red blood cells are destroyed, resulting in an excess of these substances circulating in the blood. Excess bilirubin in the blood causes [[jaundice]] and increases the risk of developing gallstones. | PKLR gene mutations result in '''reduced pyruvate kinase enzyme function''', causing a '''shortage of ATP in red blood cells''' and increased levels of other molecules produced earlier in the glycolysis process. The abnormal red blood cells are gathered up by the spleen and destroyed, causing [[hemolytic anemia]] and an enlarged spleen. A shortage of red blood cells to carry oxygen throughout the body leads to fatigue, pallor, and shortness of breath. Iron and a molecule called [[bilirubin]] are released when red blood cells are destroyed, resulting in an excess of these substances circulating in the blood. Excess bilirubin in the blood causes [[jaundice]] and increases the risk of developing gallstones. | ||
Pyruvate kinase deficiency may also occur as an effect of other blood diseases, such as [[leukemia]]. These cases are called secondary pyruvate kinase deficiency and are not inherited. | Pyruvate kinase deficiency may also occur as an effect of other blood diseases, such as [[leukemia]]. These cases are called secondary pyruvate kinase deficiency and are not inherited. | ||
== '''Inheritance''' == | |||
This condition is inherited in an [[autosomal recessive]] pattern, which means both copies of the gene in each cell have mutations. The parents of an individual with an autosomal recessive condition each carry one copy of the mutated gene, but they typically do not show signs and symptoms of the condition. | This condition is inherited in an [[autosomal recessive]] pattern, which means both copies of the gene in each cell have mutations. The parents of an individual with an autosomal recessive condition each carry one copy of the mutated gene, but they typically do not show signs and symptoms of the condition. | ||
== '''Signs and symptoms''' == | == '''Signs and symptoms''' == | ||
People with this disorder have a condition known as chronic [[hemolytic anemia]], in which red blood cells are broken down (undergo [[hemolysis]]) prematurely, resulting in a shortage of red blood cells ([[anemia]]). Specifically, pyruvate kinase deficiency is a common cause of a type of [[inherited hemolytic anemia]] called hereditary nonspherocytic hemolytic anemia. In hereditary nonspherocytic hemolytic anemia, the red blood cells do not assume a spherical shape as they do in some other forms of [[hemolytic anemia]]. | People with this disorder have a condition known as chronic [[hemolytic anemia]], in which red blood cells are broken down (undergo [[hemolysis]]) prematurely, resulting in a shortage of red blood cells ([[anemia]]). Specifically, pyruvate kinase deficiency is a common cause of a type of [[inherited hemolytic anemia]] called hereditary nonspherocytic hemolytic anemia. In hereditary nonspherocytic hemolytic anemia, the red blood cells do not assume a spherical shape as they do in some other forms of [[hemolytic anemia]]. | ||
Chronic hemolytic anemia can lead to unusually pale skin (pallor), yellowing of the eyes and skin ([[jaundice]), extreme tiredness (fatigue), shortness of breath ([[dyspnea]]), and a rapid heart rate ([[tachycardia]]). An enlarged spleen ([[splenomegaly]]), an excess of iron in the blood, and small pebble-like deposits in the gallbladder or bile ducts ([[gallstones]]) are also common in this disorder. | Chronic hemolytic anemia can lead to unusually pale skin (pallor), yellowing of the eyes and skin ([[jaundice]), extreme tiredness (fatigue), shortness of breath ([[dyspnea]]), and a rapid heart rate ([[tachycardia]]). An enlarged spleen ([[splenomegaly]]), an excess of iron in the blood, and small pebble-like deposits in the gallbladder or bile ducts ([[gallstones]]) are also common in this disorder. | ||
In people with pyruvate kinase deficiency, hemolytic anemia and associated complications may range from mild to severe. Some affected individuals have few or no symptoms. Severe cases can be life-threatening in infancy, and such affected individuals may require regular blood transfusions to survive. The symptoms of this disorder may get worse during an infection or pregnancy. | In people with pyruvate kinase deficiency, hemolytic anemia and associated complications may range from mild to severe. Some affected individuals have few or no symptoms. Severe cases can be life-threatening in infancy, and such affected individuals may require regular blood transfusions to survive. The symptoms of this disorder may get worse during an infection or pregnancy. | ||
For most diseases, symptoms will vary from person to person. People with the same disease may not have all the symptoms listed. | |||
For most diseases, symptoms will vary from person to person. People with the same disease may not have all the symptoms listed. | |||
80%-99% of people have these symptoms | 80%-99% of people have these symptoms | ||
* Chronic [[hemolytic anemia]] | * Chronic [[hemolytic anemia]] | ||
| Line 45: | Line 52: | ||
* Reticulocytosis(Increased immature red blood cells) | * Reticulocytosis(Increased immature red blood cells) | ||
* Splenomegaly(Increased spleen size) | * Splenomegaly(Increased spleen size) | ||
* Unconjugated [[hyperbilirubinemia]] | * Unconjugated [[hyperbilirubinemia]] | ||
30%-79% of people have these symptoms | 30%-79% of people have these symptoms | ||
* [[Congenital]] hemolytic anemia | * [[Congenital]] hemolytic anemia | ||
* [[Hydrops fetalis]] | * [[Hydrops fetalis]] | ||
* Increased serum [[ferritin]](Elevated serum ferritin) | * Increased serum [[ferritin]](Elevated serum ferritin) | ||
* Increased serum iron | * Increased serum iron | ||
* Prolonged neonatal [[jaundice]](Prolonged yellowing of skin in newborn) | * Prolonged neonatal [[jaundice]](Prolonged yellowing of skin in newborn) | ||
5%-29% of people have these symptoms | 5%-29% of people have these symptoms | ||
* [[Anisocytosis]](Unequal size of red blood cells) | * [[Anisocytosis]](Unequal size of red blood cells) | ||
| Line 60: | Line 65: | ||
* [[Nonimmune hydrops fetalis]] | * [[Nonimmune hydrops fetalis]] | ||
* [[Poikilocytosis]] | * [[Poikilocytosis]] | ||
== '''Diagnosis''' == | == '''Diagnosis''' == | ||
The health care provider will perform a physical exam and ask about and check for symptoms such as an enlarged spleen. If PKD is suspected, tests that will likely be ordered include: | The health care provider will perform a physical exam and ask about and check for symptoms such as an enlarged spleen. If PKD is suspected, tests that will likely be ordered include: | ||
| Line 70: | Line 74: | ||
* [[Pyruvate kinase]] activity | * [[Pyruvate kinase]] activity | ||
* Stool [[urobilinogen]] | * Stool [[urobilinogen]] | ||
== '''Treatment''' == | == '''Treatment''' == | ||
Mild cases require no treatment. People with severe anemia may need [[blood transfusions]]. In newborns with dangerous levels of [[jaundice]], a health care provider may recommend an exchange transfusion. Surgical removal of the spleen ([[splenectomy]]) may also be necessary to help reduce the destruction of red blood cells. However, this does not help in all cases. With small children, this is delayed as long as possible to allow the immune system to mature. Other treatment is symptomatic and supportive. Someone who had a splenectomy should receive the [[pneumococcal vaccine]] at recommended intervals. They also should receive preventive [[antibiotics]] until age 5. | Mild cases require no treatment. People with severe anemia may need [[blood transfusions]]. In newborns with dangerous levels of [[jaundice]], a health care provider may recommend an exchange transfusion. Surgical removal of the spleen ([[splenectomy]]) may also be necessary to help reduce the destruction of red blood cells. However, this does not help in all cases. With small children, this is delayed as long as possible to allow the immune system to mature. Other treatment is symptomatic and supportive. Someone who had a splenectomy should receive the [[pneumococcal vaccine]] at recommended intervals. They also should receive preventive [[antibiotics]] until age 5. | ||
== '''Prognosis''' == | == '''Prognosis''' == | ||
The outcome varies. Some people have few or no symptoms. Others have severe symptoms. Treatment can usually make symptoms less severe. | The outcome varies. Some people have few or no symptoms. Others have severe symptoms. Treatment can usually make symptoms less severe. | ||
'''Possible Complications''' | '''Possible Complications''' | ||
Gallstones are a common problem. They are made of too much bilirubin, which is produced during hemolytic anemia. Severe pneumococcal disease is a possible complication after splenectomy. | Gallstones are a common problem. They are made of too much bilirubin, which is produced during hemolytic anemia. Severe pneumococcal disease is a possible complication after splenectomy. | ||
{{Diseases of RBCs}} | {{Diseases of RBCs}} | ||
{{Inborn errors of carbohydrate metabolism}} | {{Inborn errors of carbohydrate metabolism}} | ||
{{DEFAULTSORT:Pyruvate Kinase Deficiency}} | {{DEFAULTSORT:Pyruvate Kinase Deficiency}} | ||
[[Category:Inborn errors of carbohydrate metabolism]] | [[Category:Inborn errors of carbohydrate metabolism]] | ||
Latest revision as of 20:18, 8 April 2025

Editor-In-Chief: Prab R Tumpati, MD
Obesity, Sleep & Internal medicine
Founder, WikiMD Wellnesspedia &
W8MD medical weight loss NYC and sleep center NYC
| Pyruvate kinase deficiency | |
|---|---|
| |
| Synonyms | N/A |
| Pronounce | N/A |
| Specialty | N/A |
| Symptoms | Hemolytic anemia, jaundice, fatigue, splenomegaly |
| Complications | Gallstones, iron overload, heart failure |
| Onset | Neonatal or childhood |
| Duration | Lifelong |
| Types | N/A |
| Causes | Genetic mutation in the PKLR gene |
| Risks | Autosomal recessive inheritance |
| Diagnosis | Blood test, genetic testing |
| Differential diagnosis | Hereditary spherocytosis, G6PD deficiency, thalassemia |
| Prevention | N/A |
| Treatment | Blood transfusion, splenectomy, folic acid supplementation |
| Medication | None specific |
| Prognosis | Variable, depending on severity |
| Frequency | 1 in 20,000 people |
| Deaths | N/A |
Other Names: Pyruvate kinase deficiency of red cells; Pyruvate kinase deficiency of erythrocytes; PK deficiency
Pyruvate kinase deficiency is a genetic blood disorder characterized by low levels of an enzyme called pyruvate kinase, which is used by red blood cells. Without pyruvate kinase, red blood cells break down too easily, resulting in low levels of these cells (hemolytic anemia).

Epidemiology[edit]
Pyruvate kinase deficiency is the most common inherited cause of nonspherocytic hemolytic anemia. More than 500 affected families have been identified, and studies suggest that the disorder may be underdiagnosed because mild cases may not be identified. Pyruvate kinase deficiency is found in all ethnic groups. Its prevalence has been estimated at 1 in 20,000 people of European descent. It is more common in the Old Order Amish population of Pennsylvania.
Cause[edit]

Pyruvate kinase deficiency is caused by mutations in the PKLR gene. The PKLR gene is active in the liver and in red blood cells, where it provides instructions for making an enzyme called pyruvate kinase. The pyruvate kinase enzyme is involved in a critical energy-producing process known as glycolysis. During glycolysis, the simple sugar glucose is broken down to produce adenosine triphosphate (ATP), the cell's main energy source. PKLR gene mutations result in reduced pyruvate kinase enzyme function, causing a shortage of ATP in red blood cells and increased levels of other molecules produced earlier in the glycolysis process. The abnormal red blood cells are gathered up by the spleen and destroyed, causing hemolytic anemia and an enlarged spleen. A shortage of red blood cells to carry oxygen throughout the body leads to fatigue, pallor, and shortness of breath. Iron and a molecule called bilirubin are released when red blood cells are destroyed, resulting in an excess of these substances circulating in the blood. Excess bilirubin in the blood causes jaundice and increases the risk of developing gallstones. Pyruvate kinase deficiency may also occur as an effect of other blood diseases, such as leukemia. These cases are called secondary pyruvate kinase deficiency and are not inherited.
Inheritance[edit]
This condition is inherited in an autosomal recessive pattern, which means both copies of the gene in each cell have mutations. The parents of an individual with an autosomal recessive condition each carry one copy of the mutated gene, but they typically do not show signs and symptoms of the condition.
Signs and symptoms[edit]
People with this disorder have a condition known as chronic hemolytic anemia, in which red blood cells are broken down (undergo hemolysis) prematurely, resulting in a shortage of red blood cells (anemia). Specifically, pyruvate kinase deficiency is a common cause of a type of inherited hemolytic anemia called hereditary nonspherocytic hemolytic anemia. In hereditary nonspherocytic hemolytic anemia, the red blood cells do not assume a spherical shape as they do in some other forms of hemolytic anemia. Chronic hemolytic anemia can lead to unusually pale skin (pallor), yellowing of the eyes and skin ([[jaundice]), extreme tiredness (fatigue), shortness of breath (dyspnea), and a rapid heart rate (tachycardia). An enlarged spleen (splenomegaly), an excess of iron in the blood, and small pebble-like deposits in the gallbladder or bile ducts (gallstones) are also common in this disorder. In people with pyruvate kinase deficiency, hemolytic anemia and associated complications may range from mild to severe. Some affected individuals have few or no symptoms. Severe cases can be life-threatening in infancy, and such affected individuals may require regular blood transfusions to survive. The symptoms of this disorder may get worse during an infection or pregnancy. For most diseases, symptoms will vary from person to person. People with the same disease may not have all the symptoms listed. 80%-99% of people have these symptoms
- Chronic hemolytic anemia
- Reduced red cell pyruvate kinase level
- Reticulocytosis(Increased immature red blood cells)
- Splenomegaly(Increased spleen size)
- Unconjugated hyperbilirubinemia
30%-79% of people have these symptoms
- Congenital hemolytic anemia
- Hydrops fetalis
- Increased serum ferritin(Elevated serum ferritin)
- Increased serum iron
- Prolonged neonatal jaundice(Prolonged yellowing of skin in newborn)
5%-29% of people have these symptoms
- Anisocytosis(Unequal size of red blood cells)
- Elevated transferrin saturation
- Intrauterine growth retardation(Prenatal growth deficiency)
- Nonimmune hydrops fetalis
- Poikilocytosis
Diagnosis[edit]
The health care provider will perform a physical exam and ask about and check for symptoms such as an enlarged spleen. If PKD is suspected, tests that will likely be ordered include:
- Bilirubin in the blood
- CBC
- Genetic testing for mutation in the pyruvate kinase gene
- Haptoglobin blood test
- Osmotic fragility
- Pyruvate kinase activity
- Stool urobilinogen
Treatment[edit]
Mild cases require no treatment. People with severe anemia may need blood transfusions. In newborns with dangerous levels of jaundice, a health care provider may recommend an exchange transfusion. Surgical removal of the spleen (splenectomy) may also be necessary to help reduce the destruction of red blood cells. However, this does not help in all cases. With small children, this is delayed as long as possible to allow the immune system to mature. Other treatment is symptomatic and supportive. Someone who had a splenectomy should receive the pneumococcal vaccine at recommended intervals. They also should receive preventive antibiotics until age 5.
Prognosis[edit]
The outcome varies. Some people have few or no symptoms. Others have severe symptoms. Treatment can usually make symptoms less severe. Possible Complications Gallstones are a common problem. They are made of too much bilirubin, which is produced during hemolytic anemia. Severe pneumococcal disease is a possible complication after splenectomy.
| Diseases of red blood cells | ||||
|---|---|---|---|---|
|
| Inborn error of carbohydrate metabolism: monosaccharide metabolism disorders (E73–E74, 271) Including glycogen storage diseases (GSD) |
||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
NIH genetic and rare disease info[edit]
Pyruvate kinase deficiency is a rare disease.
| Rare and genetic diseases | ||||||
|---|---|---|---|---|---|---|
|
Rare diseases - Pyruvate kinase deficiency
|


