Mammoplasia: Difference between revisions
m 1 revision imported |
CSV import |
||
| Line 57: | Line 57: | ||
[[Category:Breast diseases]] | [[Category:Breast diseases]] | ||
[[Category:Medical terminology]] | [[Category:Medical terminology]] | ||
<gallery> | |||
File:Breast_changes_during_pregnancy_1.png|Breast changes during pregnancy | |||
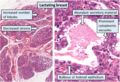
File:Histology_of_lactating_breast,_annotated.png|Histology of lactating breast, annotated | |||
</gallery> | |||
Revision as of 01:10, 18 February 2025
| Mammoplasia | |
|---|---|

| |
| Synonyms | |
| Pronounce | |
| Field | |
| Symptoms | |
| Complications | |
| Onset | |
| Duration | |
| Types | |
| Causes | |
| Risks | |
| Diagnosis | |
| Differential diagnosis | |
| Prevention | |
| Treatment | |
| Medication | |
| Prognosis | |
| Frequency | |
| Deaths | |
Mammoplasia is the normal or spontaneous enlargement of human breasts.<ref name="Nathanson1946">,
Present Concepts of Benign Breast Disease, New England Journal of Medicine, 1946, Vol. 235(Issue: 15), pp. 548–553, DOI: 10.1056/NEJM194610102351505,</ref> Mammoplasia occurs normally during puberty and pregnancy in women, as well as during certain periods of the menstrual cycle.<ref name="JatoiKaufmann2010">, Management of Breast Diseases. online version, Springer Science & Business Media, ISBN 978-3-540-69743-5, Pages: 21–,</ref><ref name="ArunNarendra2012">, Progress in Obstetrics and Gynecology--3. online version, Jaypee Brothers Medical Publishers Pvt. Ltd., ISBN 978-93-5090-575-3, Pages: 393–394,</ref><ref name="PescovitzEugster2004">, Pediatric Endocrinology: Mechanisms, Manifestations, and Management. online version, Lippincott Williams & Wilkins, 2004, ISBN 978-0-7817-4059-3, Pages: 349–,</ref> When it occurs in males, it is called gynecomastia and is considered to be pathological.<ref name="PescovitzEugster2004" /> When it occurs in females and is extremely excessive, it is called macromastia (also known as gigantomastia or breast hypertrophy) and is similarly considered to be pathological.<ref name="CoranCaldamone2012">, Pediatric Surgery. online version, Elsevier Health Sciences, ISBN 978-0-323-09161-9, Pages: 773–,</ref><ref name="Dabbs2012">{{{last}}}, David J. Dabbs, Breast Pathology. online version, Elsevier Health Sciences, 2012, ISBN 978-1-4377-0604-8, Pages: 19–,</ref><ref name="LaverySanfilippo2012">, Pediatric and Adolescent Obstetrics and Gynecology. online version, Springer Science & Business Media, ISBN 978-1-4612-5064-7, Pages: 99–,</ref> Mammoplasia may be due to breast engorgement, which is temporary enlargement of the breasts caused by the production and storage of breast milk in association with lactation and/or galactorrhea (excessive or inappropriate production of milk).<ref name="TALWARSRIVASTAVA2002">, TEXTBOOK OF BIOCHEMISTRY AND HUMAN BIOLOGY. online version, PHI Learning Pvt. Ltd., ISBN 978-81-203-1965-3, Pages: 959–,</ref> Mastodynia (breast tenderness/pain) frequently co-occurs with mammoplasia.<ref name="Zink1988">{{{last}}}, Christoph Zink, Dictionary of Obstetrics and Gynecology. online version, Walter de Gruyter, ISBN 978-3-11-085727-6, Pages: 152–,</ref><ref name="SeegenschmiedtMakoski2009">, Radiotherapy for Non-Malignant Disorders. online version, Springer Science & Business Media, ISBN 978-3-540-68943-0, Pages: 719–,</ref>
During the luteal phase (latter half) of the menstrual cycle, due to increased mammary blood flow and/or premenstrual fluid retention caused by high circulating concentrations of estrogen and/or progesterone, the breasts temporarily increase in size, and this is experienced by women as fullness, heaviness, swollenness, and a tingling sensation.<ref name="LawrenceLawrence2015">,
Breastfeeding: A Guide for the Medical Profession. online version, Elsevier Health Sciences, ISBN 978-0-323-35776-0,</ref><ref name="pmid1192144">, Changes in breast volume during normal menstrual cycle and after oral contraceptives, Br Med J, 1975, Vol. 4(Issue: 5995), pp. 494–6, DOI: 10.1136/bmj.4.5995.494, PMID: 1192144, PMC: 1675650,</ref>
Mammoplasia can be an effect or side effect of various drugs, including estrogens,<ref name="JatoiKaufmann2010" /><ref name="Lewis1998">{{{last}}},
Robert Alan Lewis, Lewis' Dictionary of Toxicology. online version, CRC Press, ISBN 978-1-56670-223-2, Pages: 470–,</ref> antiandrogens such as spironolactone,<ref name="Aronson2009">{{{last}}}, Jeffrey K. Aronson, Meyler's Side Effects of Cardiovascular Drugs. online version, Elsevier, ISBN 978-0-08-093289-7, Pages: 255–,</ref> cyproterone acetate,<ref name="Martin2015">{{{last}}}, Elizabeth Martin, Concise Medical Dictionary. online version, Oxford University Press, ISBN 978-0-19-968781-7, Pages: 189–,</ref> bicalutamide,<ref name="WalshWorthington2010">, Dr. Patrick Walsh's Guide to Surviving Prostate Cancer, Second Edition. online version, Grand Central Publishing, ISBN 978-1-4555-0016-1, Pages: 258–,</ref><ref name="Simon2004">{{{last}}}, Harvey B. Simon, The Harvard Medical School Guide to Men's Health: Lessons from the Harvard Men's Health Studies. online version, Simon and Schuster, ISBN 978-0-684-87182-0, Pages: 403–,</ref> and finasteride,<ref>{{{last}}}, Jeffrey K. Aronson, Meyler's Side Effects of Endocrine and Metabolic Drugs. online version, Elsevier, ISBN 978-0-08-093292-7, Pages: 155–,</ref><ref name="BurchumRosenthal2014">, Lehne's Pharmacology for Nursing Care. online version, Elsevier Health Sciences, ISBN 978-0-323-34026-7, Pages: 802–,</ref> growth hormone,<ref name="Kaur2003">{{{last}}}, Sat Dharam Kaur, The Complete Natural Medicine Guide to Breast Cancer: A Practical Manual for Understanding, Prevention & Care. online version, R. Rose, 2003, ISBN 978-0-7788-0083-5,</ref><ref name="SouzaCollett-Solberg2011">, Adverse effects of growth hormone replacement therapy in children, Arquivos Brasileiros de Endocrinologia & Metabologia, 2011, Vol. 55(Issue: 8), pp. 559–565, DOI: 10.1590/S0004-27302011000800009,</ref> and drugs that elevate prolactin levels such as D2 receptor antagonists like antipsychotics (e.g., risperidone), metoclopramide, and domperidone<ref name="pmid18473017">, Pharmacological causes of hyperprolactinemia, Ther Clin Risk Manag, 2007, Vol. 3(Issue: 5), pp. 929–51, PMID: 18473017, PMC: 2376090,</ref><ref name="MadhusoodananParida2010">, Hyperprolactinemia associated with psychotropics-a review, Human Psychopharmacology: Clinical and Experimental, 2010, Vol. 25(Issue: 4), pp. 281–297, DOI: 10.1002/hup.1116, PMID: 20521318,</ref> and certain antidepressants like selective serotonin reuptake inhibitors (SSRIs) and tricyclic antidepressants (TCAs).<ref name="MadhusoodananParida2010" /><ref name="LiebermanTasman2006">, Handbook of Psychiatric Drugs. online version, John Wiley & Sons, ISBN 978-0-470-02821-6, Pages: 75–,</ref><ref name="KaufmanPodolsky2013">, Antidepressant-Selective Gynecomastia, Annals of Pharmacotherapy, 2013, Vol. 47(Issue: 1), pp. e6, DOI: 10.1345/aph.1R491, PMID: 23324513,</ref> The risk appears to be less with serotonin-norepinephrine reuptake inhibitors (SNRIs) like venlafaxine.<ref name="pmid9479619" /> The "atypical" antidepressants mirtazapine and bupropion do not increase prolactin levels (bupropion may actually decrease prolactin levels), and hence there may be no risk with these agents.<ref name="pmid18473017" /> Other drugs that have been associated with mammoplasia include D-penicillamine, bucillamine, neothetazone, ciclosporin, indinavir, marijuana, and cimetidine.<ref name="Dabbs2012"/><ref name="DanceyKhan2008">, Gigantomastia – a classification and review of the literature, Journal of Plastic, Reconstructive & Aesthetic Surgery, 2008, Vol. 61(Issue: 5), pp. 493–502, DOI: 10.1016/j.bjps.2007.10.041, PMID: 18054304,</ref>
A 1997 study found an association between the SSRIs and mammoplasia in 23 (39%) of its 59 female participants.<ref name="pmid9479619">,
Breast enlargement during chronic antidepressant therapy, J Affect Disord, 1997, Vol. 46(Issue: 2), pp. 151–6, DOI: 10.1016/s0165-0327(97)00086-4, PMID: 9479619,</ref> Studies have also found associations between SSRIs and galactorrhea.<ref name="LiebermanTasman2006"/><ref name="pmid20527996">, Antidepressant-induced hyperprolactinaemia: incidence, mechanisms and management, CNS Drugs, 2010, Vol. 24(Issue: 7), pp. 563–74, DOI: 10.2165/11533140-000000000-00000, PMID: 20527996,</ref><ref name="MondalSaha2013">, A new logical insight and putative mechanism behind fluoxetine-induced amenorrhea, hyperprolactinemia and galactorrhea in a case series, Therapeutic Advances in Psychopharmacology, 2013, Vol. 3(Issue: 6), pp. 322–334, DOI: 10.1177/2045125313490305, PMID: 24294485, PMC: 3840809,</ref><ref name="Sadock2013">{{{last}}}, Benjamin Sadock, Kaplan & Sadock's Pocket Handbook of Psychiatric Drug Treatment. online version, Lippincott Williams & Wilkins, ISBN 978-1-4698-5538-7, Pages: 312–,</ref> These side effects seem to be due to hyperprolactinemia (elevated prolactin levels) induced by these drugs, an effect that appears to be caused by serotonin-mediated inhibition of tuberoinfundibular dopaminergic neurons that inhibit prolactin secretion.<ref name="pmid9479619" /><ref name="pmid20527996" /><ref name="MondalSaha2013" /> It is noteworthy that the mammoplasia these drugs can cause has been found to be highly correlated with concomitant weight gain (in the 1997 study, 83% of those who experienced weight gain also experienced mammoplasia, while only 30% of those who did not experience weight gain experienced mammoplasia).<ref name="pmid9479619" /> The mammoplasia associated with SSRIs is reported to be reversible with drug discontinuation.<ref name="Sadock2013" /> SSRIs have notably been associated with a modestly increased risk of breast cancer.<ref name="pmid25934397">, Anti-depressant therapy and cancer risk: A nested case-control study, Eur Neuropsychopharmacol, 2015, Vol. 25(Issue: 8), pp. 1147–57, DOI: 10.1016/j.euroneuro.2015.04.010, PMID: 25934397,</ref> This is in accordance with higher prolactin levels being associated with increased breast cancer risk.<ref name="HankinsonWillett1999">, Plasma Prolactin Levels and Subsequent Risk of Breast Cancer in Postmenopausal Women, JNCI Journal of the National Cancer Institute, 1999, Vol. 91(Issue: 7), pp. 629–634, DOI: 10.1093/jnci/91.7.629, PMID: 10203283,</ref><ref name="Tworoger2004">, Plasma Prolactin Concentrations and Risk of Postmenopausal Breast Cancer, Cancer Research, 2004, Vol. 64(Issue: 18), pp. 6814–6819, DOI: 10.1158/0008-5472.CAN-04-1870, PMID: 15375001,</ref>
In puberty induction in hypogonadal girls and in feminizing hormone therapy in transgender women, as well as hormonal breast enhancement in women with breast hypoplasia or small breasts, mammoplasia is a desired effect.<ref name="pmid18174716">,
Introduction and management of puberty in girls, Horm. Res., 2007, Vol. 68 Suppl 5(Issue: 5), pp. 80–3, DOI: 10.1159/000110584, PMID: 18174716,</ref><ref name="GöretzlehnerLauritzen2012">, Praktische Hormontherapie in der Gynäkologie. online version, Walter de Gruyter, ISBN 978-3-11-024568-4, Pages: 385–,</ref><ref name="ManselFodstad2007">, Metastasis of Breast Cancer. online version, Springer Science & Business Media, ISBN 978-1-4020-5866-0, Pages: 217–,</ref><ref name="pmid9610425">, Hormonal breast augmentation: prognostic relevance of insulin-like growth factor-I, Gynecol. Endocrinol., 1998, Vol. 12(Issue: 2), pp. 123–7, DOI: 10.3109/09513599809024960, PMID: 9610425,</ref>
See also
References
<references group="" responsive="1"></references>
External links
| Breast disease | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
-
Breast changes during pregnancy
-
Histology of lactating breast, annotated