Back pain: Difference between revisions
No edit summary |
CSV import |
||
| Line 1: | Line 1: | ||
{{SI}} | |||
{{Infobox medical condition | |||
| name = Back pain | |||
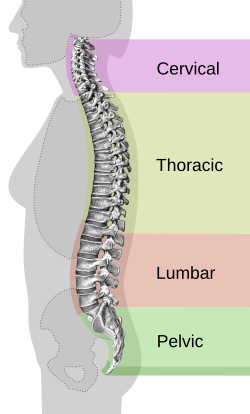
| image = [[File:Spinal_column_curvature-en.svg|250px]] | |||
| caption = Diagram of the [[spinal column]] | |||
| field = [[Orthopedics]], [[Rheumatology]], [[Neurology]] | |||
| symptoms = [[Pain]] in the [[back]], [[muscle]] ache, [[shooting pain]], [[limited range of motion]] | |||
| complications = [[Chronic pain]], [[disability]] | |||
| onset = Can be [[acute]] or [[chronic]] | |||
| duration = Varies from days to years | |||
| causes = [[Muscle strain]], [[herniated disc]], [[arthritis]], [[osteoporosis]], [[scoliosis]] | |||
| risks = [[Age]], [[lack of exercise]], [[obesity]], [[smoking]], [[occupational hazards]] | |||
| diagnosis = [[Physical examination]], [[imaging studies]] such as [[X-ray]], [[CT scan]], [[MRI]] | |||
| differential = [[Kidney stones]], [[infections]], [[cancer]] | |||
| treatment = [[Physical therapy]], [[medication]], [[surgery]] | |||
| medication = [[NSAIDs]], [[muscle relaxants]], [[opioids]] | |||
| frequency = Affects about 80% of people at some point in their lives | |||
| deaths = Rarely directly fatal | |||
}} | |||
{{SI}} | {{SI}} | ||
'''Back pain''' is a widespread [[musculoskeletal disorder]] that affects approximately 80% of individuals at some point in their lives. It can present as a dull, constant ache or a sudden, sharp sensation. [[Acute pain]] typically lasts a few days to several weeks, while [[chronic pain]] persists for more than three months. | '''Back pain''' is a widespread [[musculoskeletal disorder]] that affects approximately 80% of individuals at some point in their lives. It can present as a dull, constant ache or a sudden, sharp sensation. [[Acute pain]] typically lasts a few days to several weeks, while [[chronic pain]] persists for more than three months. | ||
[[File:Dolor espalda.png|left|thumb|Back pain can range from mild to debilitating]] | |||
[[File:Dolor espalda.png|thumb|Back pain can range from mild to debilitating]] | |||
Although most cases of back pain resolve over time, recovery may be gradual. Over-the-counter [[analgesics]] and short periods of rest can provide temporary relief. However, extended bed rest beyond one or two days may worsen symptoms. | Although most cases of back pain resolve over time, recovery may be gradual. Over-the-counter [[analgesics]] and short periods of rest can provide temporary relief. However, extended bed rest beyond one or two days may worsen symptoms. | ||
Medical attention is advised if severe back pain does not improve within three days or follows a [[spinal injury]], [[fall]], or lifting a heavy object. The causes and treatments for back pain vary widely and may involve medications, [[physical therapy]], [[complementary and alternative medicine]], and in some cases, [[spinal surgery]]. | Medical attention is advised if severe back pain does not improve within three days or follows a [[spinal injury]], [[fall]], or lifting a heavy object. The causes and treatments for back pain vary widely and may involve medications, [[physical therapy]], [[complementary and alternative medicine]], and in some cases, [[spinal surgery]]. | ||
== Epidemiology == | == Epidemiology == | ||
* Back pain affects nearly 8 in 10 people at some point in life. | * Back pain affects nearly 8 in 10 people at some point in life. | ||
* It is one of the most common reasons for missed work and doctor visits. | * It is one of the most common reasons for missed work and doctor visits. | ||
* Chronic back pain is more common in adults over the age of 30. | * Chronic back pain is more common in adults over the age of 30. | ||
== Risk Factors == | == Risk Factors == | ||
[[File:Depiction of a person suffering from back pain.png|thumb|Postural habits can contribute to back pain]] | [[File:Depiction of a person suffering from back pain.png|left|thumb|Postural habits can contribute to back pain]] | ||
Back pain can affect anyone, but certain factors increase susceptibility: | Back pain can affect anyone, but certain factors increase susceptibility: | ||
* '''[[Age]]''': Risk increases with age, especially between 30 and 50 years. | * '''[[Age]]''': Risk increases with age, especially between 30 and 50 years. | ||
| Line 25: | Line 39: | ||
* '''[[Stress]]''': Increases [[muscle tension]] and perception of pain. | * '''[[Stress]]''': Increases [[muscle tension]] and perception of pain. | ||
* '''[[Diseases]]''': [[Arthritis]], [[osteoporosis]], and [[metastatic cancer]] can all contribute to spinal pain. | * '''[[Diseases]]''': [[Arthritis]], [[osteoporosis]], and [[metastatic cancer]] can all contribute to spinal pain. | ||
== Classification == | == Classification == | ||
Back pain is broadly categorized into: | Back pain is broadly categorized into: | ||
* '''Acute back pain''': Sudden onset, usually resolving within six weeks. | * '''Acute back pain''': Sudden onset, usually resolving within six weeks. | ||
* '''Chronic back pain''': Lasting more than three months, may arise gradually or abruptly. | * '''Chronic back pain''': Lasting more than three months, may arise gradually or abruptly. | ||
== Causes == | == Causes == | ||
Back pain may result from a range of mechanical, traumatic, or pathological conditions: | Back pain may result from a range of mechanical, traumatic, or pathological conditions: | ||
=== Mechanical Causes === | === Mechanical Causes === | ||
* [[Herniated disc]] or [[degenerative disc disease]] | * [[Herniated disc]] or [[degenerative disc disease]] | ||
| Line 40: | Line 51: | ||
* [[Spondylolisthesis]] | * [[Spondylolisthesis]] | ||
* [[Facet joint]] dysfunction | * [[Facet joint]] dysfunction | ||
=== Injuries === | === Injuries === | ||
* [[Ligament sprains]] or [[muscle strains]] | * [[Ligament sprains]] or [[muscle strains]] | ||
* [[Vertebral fractures]], often related to [[osteoporosis]] | * [[Vertebral fractures]], often related to [[osteoporosis]] | ||
* [[Whiplash]] or trauma from accidents | * [[Whiplash]] or trauma from accidents | ||
=== Medical Conditions === | === Medical Conditions === | ||
* [[Arthritis]], including [[rheumatoid arthritis]] and [[osteoarthritis]] | * [[Arthritis]], including [[rheumatoid arthritis]] and [[osteoarthritis]] | ||
| Line 52: | Line 61: | ||
* [[Spinal infections]] or [[tumors]] | * [[Spinal infections]] or [[tumors]] | ||
* [[Pregnancy]]-related musculoskeletal stress | * [[Pregnancy]]-related musculoskeletal stress | ||
== Diagnosis == | == Diagnosis == | ||
Evaluation typically involves: | Evaluation typically involves: | ||
| Line 60: | Line 68: | ||
* [[Blood tests]] to rule out infections or inflammatory conditions | * [[Blood tests]] to rule out infections or inflammatory conditions | ||
* [[Nerve conduction studies]] if [[radiculopathy]] is suspected | * [[Nerve conduction studies]] if [[radiculopathy]] is suspected | ||
== Treatment == | == Treatment == | ||
[[File:Spinal_column_curvature-en.svg|thumb|Curvatures of the spine can affect posture and pain]] | [[File:Spinal_column_curvature-en.svg|left|thumb|Curvatures of the spine can affect posture and pain]] | ||
=== Acute Back Pain === | === Acute Back Pain === | ||
* Short-term use of [[NSAIDs]] or [[acetaminophen]] | * Short-term use of [[NSAIDs]] or [[acetaminophen]] | ||
* Gentle movement and modified activity | * Gentle movement and modified activity | ||
* Avoidance of prolonged bed rest | * Avoidance of prolonged bed rest | ||
=== Chronic Back Pain === | === Chronic Back Pain === | ||
[[File:Lower back pain.jpg|thumb|Lower back pain is common and may persist]] | [[File:Lower back pain.jpg|left|thumb|Lower back pain is common and may persist]] | ||
* [[Physical therapy]] and guided exercises | * [[Physical therapy]] and guided exercises | ||
* Hot/cold packs | * Hot/cold packs | ||
| Line 80: | Line 85: | ||
** [[Acupuncture]] | ** [[Acupuncture]] | ||
** [[TENS (Transcutaneous electrical nerve stimulation)]] | ** [[TENS (Transcutaneous electrical nerve stimulation)]] | ||
=== Surgical Options === | === Surgical Options === | ||
Only considered in specific cases: | Only considered in specific cases: | ||
| Line 87: | Line 91: | ||
* '''[[Spinal fusion]]''': Fusing vertebrae to prevent movement | * '''[[Spinal fusion]]''': Fusing vertebrae to prevent movement | ||
* '''[[Artificial disc replacement]]''': Inserting a synthetic disc | * '''[[Artificial disc replacement]]''': Inserting a synthetic disc | ||
== Prevention == | == Prevention == | ||
* Regular [[exercise]], especially [[core strengthening]] | * Regular [[exercise]], especially [[core strengthening]] | ||
| Line 95: | Line 98: | ||
* Lifting with the legs, not the back | * Lifting with the legs, not the back | ||
* Avoiding [[smoking]] and managing stress | * Avoiding [[smoking]] and managing stress | ||
== When to Seek Medical Attention == | == When to Seek Medical Attention == | ||
Consult a healthcare provider if you experience: | Consult a healthcare provider if you experience: | ||
| Line 102: | Line 104: | ||
* Difficulty [[urinating]] or loss of [[bladder control]] | * Difficulty [[urinating]] or loss of [[bladder control]] | ||
* Fever, unintended [[weight loss]], or history of [[cancer]] | * Fever, unintended [[weight loss]], or history of [[cancer]] | ||
== Living With Back Pain == | == Living With Back Pain == | ||
* Use of hot or cold therapy as needed | * Use of hot or cold therapy as needed | ||
| Line 108: | Line 109: | ||
* Avoid high-impact activities if you have existing [[disc disease]] | * Avoid high-impact activities if you have existing [[disc disease]] | ||
* Follow a multidisciplinary approach for chronic conditions | * Follow a multidisciplinary approach for chronic conditions | ||
== External Links == | == External Links == | ||
* [https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Low-Back-Pain-Fact-Sheet NIH: Low Back Pain Fact Sheet] | * [https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Low-Back-Pain-Fact-Sheet NIH: Low Back Pain Fact Sheet] | ||
Latest revision as of 19:50, 4 April 2025

Editor-In-Chief: Prab R Tumpati, MD
Obesity, Sleep & Internal medicine
Founder, WikiMD Wellnesspedia &
W8MD's medical weight loss NYC, sleep center NYC
Philadelphia medical weight loss and Philadelphia sleep clinics
| Back pain | |
|---|---|
| |
| Synonyms | N/A |
| Pronounce | N/A |
| Specialty | N/A |
| Symptoms | Pain in the back, muscle ache, shooting pain, limited range of motion |
| Complications | Chronic pain, disability |
| Onset | Can be acute or chronic |
| Duration | Varies from days to years |
| Types | N/A |
| Causes | Muscle strain, herniated disc, arthritis, osteoporosis, scoliosis |
| Risks | Age, lack of exercise, obesity, smoking, occupational hazards |
| Diagnosis | Physical examination, imaging studies such as X-ray, CT scan, MRI |
| Differential diagnosis | Kidney stones, infections, cancer |
| Prevention | N/A |
| Treatment | Physical therapy, medication, surgery |
| Medication | NSAIDs, muscle relaxants, opioids |
| Prognosis | N/A |
| Frequency | Affects about 80% of people at some point in their lives |
| Deaths | Rarely directly fatal |

Editor-In-Chief: Prab R Tumpati, MD
Obesity, Sleep & Internal medicine
Founder, WikiMD Wellnesspedia &
W8MD's medical weight loss NYC, sleep center NYC
Philadelphia medical weight loss and Philadelphia sleep clinics
Back pain is a widespread musculoskeletal disorder that affects approximately 80% of individuals at some point in their lives. It can present as a dull, constant ache or a sudden, sharp sensation. Acute pain typically lasts a few days to several weeks, while chronic pain persists for more than three months.

Although most cases of back pain resolve over time, recovery may be gradual. Over-the-counter analgesics and short periods of rest can provide temporary relief. However, extended bed rest beyond one or two days may worsen symptoms. Medical attention is advised if severe back pain does not improve within three days or follows a spinal injury, fall, or lifting a heavy object. The causes and treatments for back pain vary widely and may involve medications, physical therapy, complementary and alternative medicine, and in some cases, spinal surgery.
Epidemiology[edit]
- Back pain affects nearly 8 in 10 people at some point in life.
- It is one of the most common reasons for missed work and doctor visits.
- Chronic back pain is more common in adults over the age of 30.
Risk Factors[edit]

Back pain can affect anyone, but certain factors increase susceptibility:
- Age: Risk increases with age, especially between 30 and 50 years.
- Physical fitness: Weak core and back muscles contribute to instability and pain.
- Obesity: Excess body weight places strain on the spine.
- Genetics: Some spinal conditions have a hereditary component.
- Race and ethnicity: African American women are more likely to develop spondylolisthesis.
- Occupational hazards: Jobs involving heavy lifting, twisting, or prolonged sitting can cause back problems.
- Smoking: Contributes to decreased blood supply and delayed healing.
- Stress: Increases muscle tension and perception of pain.
- Diseases: Arthritis, osteoporosis, and metastatic cancer can all contribute to spinal pain.
Classification[edit]
Back pain is broadly categorized into:
- Acute back pain: Sudden onset, usually resolving within six weeks.
- Chronic back pain: Lasting more than three months, may arise gradually or abruptly.
Causes[edit]
Back pain may result from a range of mechanical, traumatic, or pathological conditions:
Mechanical Causes[edit]
- Herniated disc or degenerative disc disease
- Spinal stenosis
- Scoliosis or abnormal spinal curvature
- Spondylolisthesis
- Facet joint dysfunction
Injuries[edit]
- Ligament sprains or muscle strains
- Vertebral fractures, often related to osteoporosis
- Whiplash or trauma from accidents
Medical Conditions[edit]
- Arthritis, including rheumatoid arthritis and osteoarthritis
- Kidney stones or urinary tract infections
- Endometriosis or fibromyalgia
- Spinal infections or tumors
- Pregnancy-related musculoskeletal stress
Diagnosis[edit]
Evaluation typically involves:
- Medical history and physical examination
- X-rays to assess bone abnormalities
- MRI or CT scan for soft tissue or nerve issues
- Blood tests to rule out infections or inflammatory conditions
- Nerve conduction studies if radiculopathy is suspected
Treatment[edit]
Acute Back Pain[edit]
- Short-term use of NSAIDs or acetaminophen
- Gentle movement and modified activity
- Avoidance of prolonged bed rest
Chronic Back Pain[edit]
- Physical therapy and guided exercises
- Hot/cold packs
- Muscle relaxants or low-dose antidepressants
- Corticosteroid injections
- Behavioral therapy to address posture and coping
- Complementary approaches:
Surgical Options[edit]
Only considered in specific cases:
- Discectomy: Removing part of a herniated disc
- Laminectomy: Removing bone to relieve nerve pressure
- Spinal fusion: Fusing vertebrae to prevent movement
- Artificial disc replacement: Inserting a synthetic disc
Prevention[edit]
- Regular exercise, especially core strengthening
- Maintaining a healthy weight
- Good posture
- Ergonomic furniture and workspaces
- Lifting with the legs, not the back
- Avoiding smoking and managing stress
When to Seek Medical Attention[edit]
Consult a healthcare provider if you experience:
- Persistent pain despite rest and medication
- Neurological symptoms like numbness or weakness
- Difficulty urinating or loss of bladder control
- Fever, unintended weight loss, or history of cancer
Living With Back Pain[edit]
- Use of hot or cold therapy as needed
- Structured exercise programs such as flexion, extension, and aerobic routines
- Avoid high-impact activities if you have existing disc disease
- Follow a multidisciplinary approach for chronic conditions
External Links[edit]
| Pain | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| Spinal disease | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|


