Trimethylaminuria: Difference between revisions
CSV import |
No edit summary |
||
| Line 1: | Line 1: | ||
{{Short description|A metabolic disorder affecting the breakdown of trimethylamine}} | {{Short description|A metabolic disorder affecting the breakdown of trimethylamine}} | ||
[[File:Autorecessive.svg|thumb|right|Diagram showing autosomal recessive inheritance.]] | |||
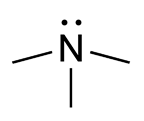
[[File:Trimethylamine_chemical_structure.png|thumb|right|Chemical structure of trimethylamine.]] | |||
'''Trimethylaminuria''' is a [[metabolic disorder]] in which an individual is unable to convert [[trimethylamine]] into [[trimethylamine N-oxide]]. This condition has existed for centuries but has only gained scientific recognition and support in the past 30 years. | |||
== What is Trimethylamine? == | |||
[[Trimethylamine]] is the compound responsible for the strong [[fish odor]]. In contrast, [[trimethylamine N-oxide]] is odorless. | |||
== What are the symptoms of trimethylaminuria? == | |||
In individuals with trimethylaminuria, trimethylamine accumulates in the body and is released through [[sweat]], [[urine]], [[reproductive fluids]], and [[breath]], causing a strong [[fishy odor]]. The severity of the odor varies among individuals. Despite this symptom, affected individuals are typically [[healthy]]. | |||
The condition appears to be more common in [[women]] than in [[men]], possibly due to the influence of [[sex hormones]] such as [[progesterone]] and [[estrogen]]. Symptoms often worsen around [[puberty]], [[menstruation]], after taking [[oral contraceptives]], and around [[menopause]]. | |||
The | |||
== | == What causes trimethylaminuria? == | ||
Trimethylaminuria | Trimethylaminuria results from an impaired version of the enzyme [[flavin-containing monooxygenase 3]] (FMO3), which converts [[trimethylamine]] into [[trimethylamine N-oxide]]. The [[FMO3 gene]] codes for this enzyme. Mutations in the FMO3 gene are linked to the condition, although the full range of the enzyme’s functions remains unknown. | ||
== | == Is trimethylaminuria inherited? == | ||
Yes, trimethylaminuria is inherited in an [[autosomal recessive]] pattern, requiring two non-functioning copies of the [[FMO3 gene]] for symptoms to appear. Carriers, who have only one altered gene, typically do not exhibit symptoms, though some may experience mild, temporary episodes of fish-like odor. Genetic mutations, [[stress]], and [[diet]] may influence the severity and onset of symptoms. | |||
[[ | == How is trimethylaminuria diagnosed? == | ||
A [[urine test]] is used to diagnose trimethylaminuria by measuring the levels of [[trimethylamine]] and [[trimethylamine N-oxide]]. The [[TMA challenge test]] involves administering trimethylamine and analyzing its excretion levels. [[Genetic testing]] can also identify mutations in the [[FMO3 gene]]. | |||
== How is trimethylaminuria treated? == | |||
There is no cure for trimethylaminuria, but individuals can manage symptoms through: | |||
* Avoiding foods high in [[trimethylamine]] and its precursors, such as: | |||
* [[Milk]] from wheat-fed cows | |||
* [[Eggs]] | |||
* [[Liver]] | |||
* [[Kidney]] | |||
* [[Peas]] | |||
* [[Beans]] | |||
* [[Peanuts]] | |||
* [[Soy products]] | |||
* [[Brassicas]] (e.g., [[Brussels sprouts]], [[broccoli]], [[cabbage]], [[cauliflower]]) | |||
* [[Lecithin]] and [[fish oil supplements]] | |||
* [[Seafood]] (e.g., [[fish]], [[cephalopods]], [[crustaceans]]) | |||
* Taking low-dose [[antibiotics]] to reduce gut bacteria that produce trimethylamine. | |||
* Using [[laxatives]] to decrease intestinal transit time and limit trimethylamine production. | |||
* Taking supplements such as: | |||
* [[Activated charcoal]] (750 mg twice daily for ten days) | |||
* [[Copper chlorophyllin]] (60 mg three times per day after meals for three weeks) | |||
* [[Riboflavin]] (30-40 mg, 3-5 times daily with food) to enhance residual [[FMO3 enzyme]] activity. | |||
* Using [[moderate pH soaps]] (pH 5.5-6.5) to retain trimethylamine in a less volatile form for removal by washing. | |||
* Avoiding factors that promote [[sweating]] (e.g., [[exercise]], [[stress]], and emotional distress). | |||
Enzyme replacement therapy with [[FMO3 enzyme]] is not currently an option. | |||
== What laboratories offer testing for trimethylaminuria? == | |||
The following laboratories offer diagnostic testing for trimethylaminuria: | |||
* '''Children's Hospital Colorado Biochemical Genetics Lab''' | |||
* Phone: 720-777-6711 | |||
* Contact: Lab Client Services | |||
* Email: [[Mailto:LabClientServices@childrenscolorado.org|LabClientServices@childrenscolorado.org]] | |||
* '''Monell Chemical Senses Center, University of Pennsylvania''' | |||
* Phone: 215-898-4713 | |||
* Contact: [[George Preti]], Ph.D. | |||
* Email: [[Mailto:preti@monell.org|preti@monell.org]] | |||
* Note: This laboratory may have a long waiting list. | |||
== | == Clinical Research on Trimethylaminuria == | ||
Currently, the [[National Human Genome Research Institute]] (NHGRI) is not conducting studies on trimethylaminuria. | |||
For research opportunities: | |||
* [[ClinicalTrials.gov]] | |||
* NHGRI Clinical Studies | |||
* Clinical Research FAQs | |||
== | == Additional Resources for Trimethylaminuria == | ||
Trimethylaminuria | * [[Genetics Home Reference: Trimethylaminuria]] | ||
* [[Online Mendelian Inheritance in Man (OMIM)]] | |||
* [[Effects of dietary supplements on urinary excretion of trimethylamine]] | |||
* [[Trimethylaminuria information from the Genetics and Rare Diseases Information Center]] | |||
* [[Finding Reliable Health Information Online]] | |||
==Related | == Related Pages == | ||
* [[Metabolic disorder]] | * [[Metabolic disorder]] | ||
* [[Genetic disorder]] | * [[Genetic disorder]] | ||
* [[Body odor]] | * [[Body odor]] | ||
[[Category:Metabolic disorders]] | [[Category:Metabolic disorders]] | ||
[[Category:Rare diseases]] | [[Category:Rare diseases]] | ||
{{genetics}} | |||
{{stub}} | |||
Revision as of 21:16, 9 February 2025
A metabolic disorder affecting the breakdown of trimethylamine

Trimethylaminuria is a metabolic disorder in which an individual is unable to convert trimethylamine into trimethylamine N-oxide. This condition has existed for centuries but has only gained scientific recognition and support in the past 30 years.
What is Trimethylamine?
Trimethylamine is the compound responsible for the strong fish odor. In contrast, trimethylamine N-oxide is odorless.
What are the symptoms of trimethylaminuria?
In individuals with trimethylaminuria, trimethylamine accumulates in the body and is released through sweat, urine, reproductive fluids, and breath, causing a strong fishy odor. The severity of the odor varies among individuals. Despite this symptom, affected individuals are typically healthy.
The condition appears to be more common in women than in men, possibly due to the influence of sex hormones such as progesterone and estrogen. Symptoms often worsen around puberty, menstruation, after taking oral contraceptives, and around menopause.
What causes trimethylaminuria?
Trimethylaminuria results from an impaired version of the enzyme flavin-containing monooxygenase 3 (FMO3), which converts trimethylamine into trimethylamine N-oxide. The FMO3 gene codes for this enzyme. Mutations in the FMO3 gene are linked to the condition, although the full range of the enzyme’s functions remains unknown.
Is trimethylaminuria inherited?
Yes, trimethylaminuria is inherited in an autosomal recessive pattern, requiring two non-functioning copies of the FMO3 gene for symptoms to appear. Carriers, who have only one altered gene, typically do not exhibit symptoms, though some may experience mild, temporary episodes of fish-like odor. Genetic mutations, stress, and diet may influence the severity and onset of symptoms.
How is trimethylaminuria diagnosed?
A urine test is used to diagnose trimethylaminuria by measuring the levels of trimethylamine and trimethylamine N-oxide. The TMA challenge test involves administering trimethylamine and analyzing its excretion levels. Genetic testing can also identify mutations in the FMO3 gene.
How is trimethylaminuria treated?
There is no cure for trimethylaminuria, but individuals can manage symptoms through:
- Avoiding foods high in trimethylamine and its precursors, such as:
* Milk from wheat-fed cows * Eggs * Liver * Kidney * Peas * Beans * Peanuts * Soy products * Brassicas (e.g., Brussels sprouts, broccoli, cabbage, cauliflower) * Lecithin and fish oil supplements * Seafood (e.g., fish, cephalopods, crustaceans)
- Taking low-dose antibiotics to reduce gut bacteria that produce trimethylamine.
- Using laxatives to decrease intestinal transit time and limit trimethylamine production.
- Taking supplements such as:
* Activated charcoal (750 mg twice daily for ten days) * Copper chlorophyllin (60 mg three times per day after meals for three weeks) * Riboflavin (30-40 mg, 3-5 times daily with food) to enhance residual FMO3 enzyme activity.
- Using moderate pH soaps (pH 5.5-6.5) to retain trimethylamine in a less volatile form for removal by washing.
- Avoiding factors that promote sweating (e.g., exercise, stress, and emotional distress).
Enzyme replacement therapy with FMO3 enzyme is not currently an option.
What laboratories offer testing for trimethylaminuria?
The following laboratories offer diagnostic testing for trimethylaminuria:
- Children's Hospital Colorado Biochemical Genetics Lab
* Phone: 720-777-6711 * Contact: Lab Client Services * Email: [[1]]
- Monell Chemical Senses Center, University of Pennsylvania
* Phone: 215-898-4713 * Contact: George Preti, Ph.D. * Email: [[2]] * Note: This laboratory may have a long waiting list.
Clinical Research on Trimethylaminuria
Currently, the National Human Genome Research Institute (NHGRI) is not conducting studies on trimethylaminuria.
For research opportunities:
- ClinicalTrials.gov
- NHGRI Clinical Studies
- Clinical Research FAQs
Additional Resources for Trimethylaminuria
- Genetics Home Reference: Trimethylaminuria
- Online Mendelian Inheritance in Man (OMIM)
- Effects of dietary supplements on urinary excretion of trimethylamine
- Trimethylaminuria information from the Genetics and Rare Diseases Information Center
- Finding Reliable Health Information Online
Related Pages
| Genetics | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
* Category
|


