Granuloma: Difference between revisions
No edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
{{Infobox medical condition (new) | |||
[[ | | name = Granuloma | ||
[[ | | synonyms = Granulomatous inflammation | ||
= | | image = Granuloma mac.jpg | ||
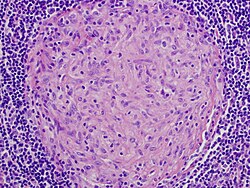
| caption = Microscopic view of a granuloma | |||
| pronounce = | |||
| specialty = [[Pathology]], [[Immunology]], [[Infectious diseases]] | |||
| symptoms = Often asymptomatic, may cause local swelling or systemic effects depending on the underlying cause | |||
| complications = Tissue damage, fibrosis, organ dysfunction, chronic inflammation | |||
| onset = Gradual | |||
| duration = Chronic | |||
| types = [[Caseating granuloma]], [[Non-caseating granuloma]], [[Foreign body granuloma]], [[Immune granuloma]] | |||
| causes = Chronic infections, autoimmune disorders, foreign body reactions, persistent irritants | |||
| risks = Exposure to [[tuberculosis]], [[fungal infections]], [[sarcoidosis]], environmental pollutants | |||
| diagnosis = [[Histopathology]], [[Biopsy]], [[Imaging studies]], [[Microbiological tests]] | |||
| differential = [[Neoplasm]], [[Abscess]], [[Fibrosis]] | |||
| prevention = Avoid exposure to known infectious agents and persistent irritants | |||
| treatment = Treat underlying cause; [[antibiotics]], [[immunosuppressants]], [[surgical excision]] in some cases | |||
| medication = [[Corticosteroids]], [[Anti-tuberculosis drugs]], [[Antifungal medications]] | |||
| prognosis = Depends on the underlying disease; often resolves if the cause is treated | |||
| frequency = Common in infectious and inflammatory diseases | |||
| deaths = Rare, except in severe systemic conditions | |||
}} | |||
'''Granuloma''' is a specialized form of chronic inflammation characterized by the formation of compact, often microscopic, nodular lesions composed of immune cells. These structures primarily consist of macrophages, lymphocytes, epithelioid cells, and multinucleated giant cells. Granulomas serve as a defensive immune mechanism, isolating foreign substances, pathogens, or irritants that the body is unable to eliminate. They commonly occur in response to persistent infections, chronic inflammatory conditions, autoimmune diseases, and foreign material exposure. | |||
Granulomas are commonly observed in diseases such as [[tuberculosis]], [[sarcoidosis]], [[leprosy]], [[fungal infections]], and chronic granulomatous disease. | |||
[[File:Tropical Diseases - Fig 94.png|thumb|Granuloma in tropical diseases]] | |||
== Pathophysiology == | |||
Granulomas form when the immune system attempts to wall off substances that it perceives as foreign but cannot eliminate. These substances include: | |||
* Infectious agents – [[Mycobacterium tuberculosis]], [[Histoplasma capsulatum]], [[Cryptococcus neoformans]], [[Leprosy]] bacilli | |||
* Environmental irritants – Silica dust, beryllium, talc, asbestos | |||
* Foreign bodies – Medical implants, sutures, injected substances | |||
* Autoimmune disorders – [[Sarcoidosis]], [[Crohn’s disease]], [[Rheumatoid arthritis]] | |||
The formation of a granuloma follows these steps: | |||
1. Chronic antigen exposure – The immune system encounters a persistent irritant or pathogen. | |||
2. Macrophage activation – Macrophages attempt to engulf and digest the irritant but fail. | |||
3. T-cell recruitment – Helper T lymphocytes (CD4+) release cytokines like [[interferon-gamma]] and [[tumor necrosis factor-alpha]] (TNF-α), which activate more macrophages. | |||
4. Formation of epithelioid cells – Macrophages enlarge and fuse, forming multinucleated giant cells (e.g., Langhans giant cells). | |||
5. Fibrosis and encapsulation – Over time, fibroblasts deposit collagen, forming a fibrous capsule around the granuloma. | |||
==See Also== | Granulomas can be classified based on their morphology: | ||
* Caseating granulomas – Contain necrotic tissue, often seen in tuberculosis. | |||
* Non-caseating granulomas – Do not contain necrosis, commonly seen in sarcoidosis and Crohn's disease. | |||
* Foreign body granulomas – Form around exogenous materials like talc, sutures, or implants. | |||
== Clinical Manifestations == | |||
Granulomas can be asymptomatic or cause a variety of symptoms depending on their size, location, and underlying cause. | |||
=== Localized Symptoms === | |||
* Lung granulomas (e.g., [[tuberculosis]], [[sarcoidosis]]) – Cough, dyspnea, chest pain | |||
* Liver granulomas (e.g., [[histoplasmosis]], [[schistosomiasis]]) – Hepatomegaly, jaundice | |||
* Skin granulomas (e.g., [[leprosy]], [[foreign body reaction]]) – Nodules, ulceration | |||
* Gastrointestinal granulomas (e.g., [[Crohn’s disease]]) – Abdominal pain, diarrhea, bowel obstruction | |||
* Lymph node granulomas – Lymphadenopathy, systemic symptoms | |||
=== Systemic Symptoms === | |||
* Fever | |||
* Fatigue | |||
* Weight loss | |||
* Night sweats | |||
* Joint pain (associated with sarcoidosis and autoimmune diseases) | |||
== Diagnosis == | |||
The definitive diagnosis of a granuloma requires histopathological examination. The diagnostic workup includes: | |||
* Histology – Biopsy with identification of epithelioid histiocytes, multinucleated giant cells, and lymphocytic infiltration. | |||
* Acid-Fast Stain – Detects Mycobacterium tuberculosis in caseating granulomas. | |||
* Fungal Stains (GMS, PAS) – Identify fungal infections like histoplasmosis. | |||
* Imaging Studies – [[Chest X-ray]] and [[CT scan]] can reveal pulmonary granulomas. | |||
* Serologic and PCR tests – Used to identify underlying infectious causes. | |||
* Blood tests – Elevated angiotensin-converting enzyme (ACE) in sarcoidosis. | |||
== Treatment == | |||
Treatment depends on the underlying cause of granuloma formation: | |||
* Infectious Granulomas | |||
* Tuberculosis – Anti-tubercular therapy (e.g., isoniazid, rifampin, ethambutol, pyrazinamide) | |||
* Fungal granulomas – Antifungal therapy (e.g., amphotericin B, itraconazole) | |||
* Leprosy – Dapsone, rifampin, clofazimine | |||
* Autoimmune and Idiopathic Granulomas | |||
* Corticosteroids – Used in sarcoidosis, Crohn’s disease, and Wegener’s granulomatosis. | |||
* Immunosuppressants – Methotrexate, azathioprine for autoimmune conditions. | |||
* Foreign Body Granulomas | |||
* Surgical removal – Necessary when granulomas cause obstruction or severe symptoms. | |||
* Steroid injections – Reduce inflammation in skin and soft tissue granulomas. | |||
== Prognosis == | |||
The prognosis of granulomas varies depending on the underlying condition: | |||
* Tuberculosis granulomas – Can resolve with proper antibiotic therapy but may lead to fibrosis or lung cavitations if untreated. | |||
* Sarcoidosis granulomas – Often resolve spontaneously but can progress to chronic fibrosis. | |||
* Fungal granulomas – Require prolonged antifungal treatment; relapse is possible. | |||
* Foreign body granulomas – Usually persist until the irritant is removed. | |||
== See Also == | |||
* [[Inflammation]] | |||
* [[Chronic granulomatous disease]] | |||
* [[Tuberculosis]] | |||
* [[Sarcoidosis]] | |||
* [[Histoplasmosis]] | |||
* [[Immune response]] | * [[Immune response]] | ||
{{Inflammation}} | {{Inflammation}} | ||
{{ | {{Medical resources | ||
| ICD10 = D76.3 | |||
| ICD9 = | |||
| OMIM = | |||
| MedlinePlus = | |||
| eMedicineSubj = | |||
| eMedicineTopic = | |||
| MeshID = D006099 | |||
}} | |||
[[Category:Anatomical pathology]] | [[Category:Anatomical pathology]] | ||
[[Category:Inflammations]] | [[Category:Inflammations]] | ||
[[Category:Pathology]] | [[Category:Pathology]] | ||
[[Category:Immunology]] | [[Category:Immunology]] | ||
[[Category:Pulmonary disorders]] | |||
{{stub}} | |||
Latest revision as of 19:27, 19 March 2025
| Granuloma | |
|---|---|
| |
| Synonyms | Granulomatous inflammation |
| Pronounce | |
| Field | N/A |
| Symptoms | Often asymptomatic, may cause local swelling or systemic effects depending on the underlying cause |
| Complications | Tissue damage, fibrosis, organ dysfunction, chronic inflammation |
| Onset | Gradual |
| Duration | Chronic |
| Types | Caseating granuloma, Non-caseating granuloma, Foreign body granuloma, Immune granuloma |
| Causes | Chronic infections, autoimmune disorders, foreign body reactions, persistent irritants |
| Risks | Exposure to tuberculosis, fungal infections, sarcoidosis, environmental pollutants |
| Diagnosis | Histopathology, Biopsy, Imaging studies, Microbiological tests |
| Differential diagnosis | Neoplasm, Abscess, Fibrosis |
| Prevention | Avoid exposure to known infectious agents and persistent irritants |
| Treatment | Treat underlying cause; antibiotics, immunosuppressants, surgical excision in some cases |
| Medication | Corticosteroids, Anti-tuberculosis drugs, Antifungal medications |
| Prognosis | Depends on the underlying disease; often resolves if the cause is treated |
| Frequency | Common in infectious and inflammatory diseases |
| Deaths | Rare, except in severe systemic conditions |
Granuloma is a specialized form of chronic inflammation characterized by the formation of compact, often microscopic, nodular lesions composed of immune cells. These structures primarily consist of macrophages, lymphocytes, epithelioid cells, and multinucleated giant cells. Granulomas serve as a defensive immune mechanism, isolating foreign substances, pathogens, or irritants that the body is unable to eliminate. They commonly occur in response to persistent infections, chronic inflammatory conditions, autoimmune diseases, and foreign material exposure.
Granulomas are commonly observed in diseases such as tuberculosis, sarcoidosis, leprosy, fungal infections, and chronic granulomatous disease.

Pathophysiology[edit]
Granulomas form when the immune system attempts to wall off substances that it perceives as foreign but cannot eliminate. These substances include:
- Infectious agents – Mycobacterium tuberculosis, Histoplasma capsulatum, Cryptococcus neoformans, Leprosy bacilli
- Environmental irritants – Silica dust, beryllium, talc, asbestos
- Foreign bodies – Medical implants, sutures, injected substances
- Autoimmune disorders – Sarcoidosis, Crohn’s disease, Rheumatoid arthritis
The formation of a granuloma follows these steps: 1. Chronic antigen exposure – The immune system encounters a persistent irritant or pathogen. 2. Macrophage activation – Macrophages attempt to engulf and digest the irritant but fail. 3. T-cell recruitment – Helper T lymphocytes (CD4+) release cytokines like interferon-gamma and tumor necrosis factor-alpha (TNF-α), which activate more macrophages. 4. Formation of epithelioid cells – Macrophages enlarge and fuse, forming multinucleated giant cells (e.g., Langhans giant cells). 5. Fibrosis and encapsulation – Over time, fibroblasts deposit collagen, forming a fibrous capsule around the granuloma.
Granulomas can be classified based on their morphology:
- Caseating granulomas – Contain necrotic tissue, often seen in tuberculosis.
- Non-caseating granulomas – Do not contain necrosis, commonly seen in sarcoidosis and Crohn's disease.
- Foreign body granulomas – Form around exogenous materials like talc, sutures, or implants.
Clinical Manifestations[edit]
Granulomas can be asymptomatic or cause a variety of symptoms depending on their size, location, and underlying cause.
Localized Symptoms[edit]
- Lung granulomas (e.g., tuberculosis, sarcoidosis) – Cough, dyspnea, chest pain
- Liver granulomas (e.g., histoplasmosis, schistosomiasis) – Hepatomegaly, jaundice
- Skin granulomas (e.g., leprosy, foreign body reaction) – Nodules, ulceration
- Gastrointestinal granulomas (e.g., Crohn’s disease) – Abdominal pain, diarrhea, bowel obstruction
- Lymph node granulomas – Lymphadenopathy, systemic symptoms
Systemic Symptoms[edit]
- Fever
- Fatigue
- Weight loss
- Night sweats
- Joint pain (associated with sarcoidosis and autoimmune diseases)
Diagnosis[edit]
The definitive diagnosis of a granuloma requires histopathological examination. The diagnostic workup includes:
- Histology – Biopsy with identification of epithelioid histiocytes, multinucleated giant cells, and lymphocytic infiltration.
- Acid-Fast Stain – Detects Mycobacterium tuberculosis in caseating granulomas.
- Fungal Stains (GMS, PAS) – Identify fungal infections like histoplasmosis.
- Imaging Studies – Chest X-ray and CT scan can reveal pulmonary granulomas.
- Serologic and PCR tests – Used to identify underlying infectious causes.
- Blood tests – Elevated angiotensin-converting enzyme (ACE) in sarcoidosis.
Treatment[edit]
Treatment depends on the underlying cause of granuloma formation:
- Infectious Granulomas
- Tuberculosis – Anti-tubercular therapy (e.g., isoniazid, rifampin, ethambutol, pyrazinamide)
- Fungal granulomas – Antifungal therapy (e.g., amphotericin B, itraconazole)
- Leprosy – Dapsone, rifampin, clofazimine
- Autoimmune and Idiopathic Granulomas
- Corticosteroids – Used in sarcoidosis, Crohn’s disease, and Wegener’s granulomatosis.
- Immunosuppressants – Methotrexate, azathioprine for autoimmune conditions.
- Foreign Body Granulomas
- Surgical removal – Necessary when granulomas cause obstruction or severe symptoms.
- Steroid injections – Reduce inflammation in skin and soft tissue granulomas.
Prognosis[edit]
The prognosis of granulomas varies depending on the underlying condition:
- Tuberculosis granulomas – Can resolve with proper antibiotic therapy but may lead to fibrosis or lung cavitations if untreated.
- Sarcoidosis granulomas – Often resolve spontaneously but can progress to chronic fibrosis.
- Fungal granulomas – Require prolonged antifungal treatment; relapse is possible.
- Foreign body granulomas – Usually persist until the irritant is removed.
See Also[edit]
| Inflammation | ||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|


