Adenoma: Difference between revisions
No edit summary |
CSV import |
||
| Line 1: | Line 1: | ||
{{Infobox medical condition | |||
| name = Adenoma | |||
| image =[[File:Tubular_adenoma_2_intermed_mag.jpg]] | |||
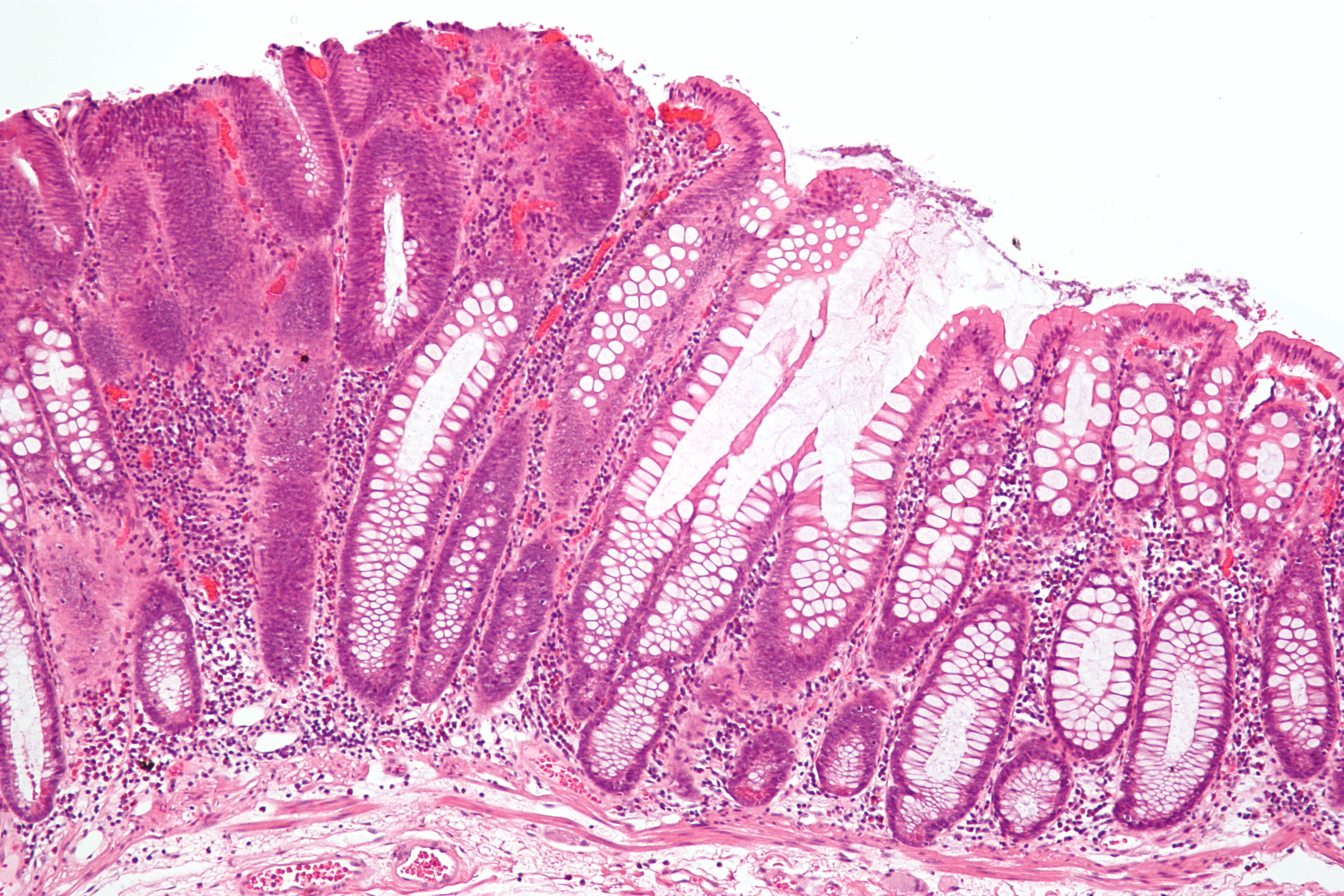
| caption = Micrograph of a [[tubular adenoma]] | |||
| field = [[Oncology]] | |||
| synonyms = | |||
| symptoms = Often asymptomatic, may cause [[hormonal imbalance]] if functional | |||
| complications = Potential progression to [[adenocarcinoma]] | |||
| onset = Varies depending on type and location | |||
| duration = Indeterminate, may remain stable or progress | |||
| types = [[Tubular adenoma]], [[villous adenoma]], [[tubulovillous adenoma]] | |||
| causes = [[Genetic mutations]], [[environmental factors]] | |||
| risks = [[Age]], [[family history]], [[diet]], [[smoking]] | |||
| diagnosis = [[Biopsy]], [[endoscopy]], [[imaging studies]] | |||
| differential = [[Hyperplasia]], [[adenocarcinoma]], [[polyp]] | |||
| prevention = Regular [[screening]], healthy [[diet]], avoiding [[smoking]] | |||
| treatment = [[Surgical removal]], [[endoscopic resection]] | |||
| medication = None specific, may use [[hormonal therapy]] if functional | |||
| prognosis = Generally good if benign, risk of malignancy varies | |||
| frequency = Common, varies by type and location | |||
| deaths = Rare, unless progresses to malignancy | |||
}} | |||
{{Short description|Benign glandular tumors with potential malignant transformation}} {{Infobox medical condition (new) | name = Adenoma | synonyms = Adenomatous tumor | image = Histopathology of adrenocortical adenoma.jpg | alt = Histopathology of adrenocortical adenoma | caption = Histopathology of an adrenocortical adenoma | pronounce = | field = [[Oncology]], [[Pathology]], [[Endocrinology]], [[Gastroenterology]] | symptoms = Often asymptomatic; may cause hormonal imbalance, obstruction, pain | complications = Malignant transformation, bleeding, organ dysfunction | onset = Variable; often detected in adults | duration = Chronic (often lifelong surveillance required) | types = Colorectal, pituitary, thyroid, adrenal, hepatic, renal, sebaceous | causes = Genetic mutations, hormonal imbalance, environmental factors | risks = Age, genetics, obesity, hormonal therapy, radiation exposure | diagnosis = Clinical evaluation, imaging, laboratory tests, biopsy | differential = Hyperplastic polyps, adenocarcinoma, neuroendocrine tumors | prevention = Lifestyle modifications, genetic screening | treatment = Surveillance, endoscopic removal, surgical excision, medical therapy | medication = Hormone suppressants, antithyroid medications, dopamine agonists | prognosis = Generally good; dependent on type, size, and malignant risk | frequency = Common (colorectal adenomas); other types vary | deaths = Rare, usually due to malignant transformation or complications }} | {{Short description|Benign glandular tumors with potential malignant transformation}} {{Infobox medical condition (new) | name = Adenoma | synonyms = Adenomatous tumor | image = Histopathology of adrenocortical adenoma.jpg | alt = Histopathology of adrenocortical adenoma | caption = Histopathology of an adrenocortical adenoma | pronounce = | field = [[Oncology]], [[Pathology]], [[Endocrinology]], [[Gastroenterology]] | symptoms = Often asymptomatic; may cause hormonal imbalance, obstruction, pain | complications = Malignant transformation, bleeding, organ dysfunction | onset = Variable; often detected in adults | duration = Chronic (often lifelong surveillance required) | types = Colorectal, pituitary, thyroid, adrenal, hepatic, renal, sebaceous | causes = Genetic mutations, hormonal imbalance, environmental factors | risks = Age, genetics, obesity, hormonal therapy, radiation exposure | diagnosis = Clinical evaluation, imaging, laboratory tests, biopsy | differential = Hyperplastic polyps, adenocarcinoma, neuroendocrine tumors | prevention = Lifestyle modifications, genetic screening | treatment = Surveillance, endoscopic removal, surgical excision, medical therapy | medication = Hormone suppressants, antithyroid medications, dopamine agonists | prognosis = Generally good; dependent on type, size, and malignant risk | frequency = Common (colorectal adenomas); other types vary | deaths = Rare, usually due to malignant transformation or complications }} | ||
'''Adenoma''' is a type of [[benign tumor]] originating from [[glandular epithelial cells]]. Although adenomas themselves are benign, some possess the potential to progress into malignant tumors ([[adenocarcinoma]]). They commonly affect various glandular organs, including the [[colon]], [[pituitary gland]], [[thyroid gland]], [[adrenal gland]], [[liver]], and [[kidney]]. Understanding their characteristics, potential complications, and management strategies is vital for early detection and treatment. | '''Adenoma''' is a type of [[benign tumor]] originating from [[glandular epithelial cells]]. Although adenomas themselves are benign, some possess the potential to progress into malignant tumors ([[adenocarcinoma]]). They commonly affect various glandular organs, including the [[colon]], [[pituitary gland]], [[thyroid gland]], [[adrenal gland]], [[liver]], and [[kidney]]. Understanding their characteristics, potential complications, and management strategies is vital for early detection and treatment. | ||
| Line 9: | Line 32: | ||
The frequency and clinical significance of adenomas vary by organ: | The frequency and clinical significance of adenomas vary by organ: | ||
* '''Colorectal adenomas''': Common in adults >50 years; precursors to colorectal cancer. | * '''Colorectal adenomas''': Common in adults >50 years; precursors to colorectal cancer. | ||
* '''Pituitary adenomas''': Account for | * '''Pituitary adenomas''': Account for 10–15% of intracranial tumors. | ||
* '''Thyroid adenomas''': Frequent in women; detected as thyroid nodules. | * '''Thyroid adenomas''': Frequent in women; detected as thyroid nodules. | ||
* '''Hepatic adenomas''': Rare; linked to oral contraceptive use. | * '''Hepatic adenomas''': Rare; linked to oral contraceptive use. | ||
== Clinical Significance == | == Clinical Significance == | ||
Adenomas can significantly impact health due to: | Adenomas can significantly impact health due to: | ||
* '''Hormonal imbalance''': Functional adenomas can cause endocrine disorders (e.g., | * '''Hormonal imbalance''': Functional adenomas can cause endocrine disorders (e.g., Cushing’s syndrome, hyperthyroidism). | ||
* '''Obstruction''': Large adenomas in the colon may cause bowel obstruction. | * '''Obstruction''': Large adenomas in the colon may cause bowel obstruction. | ||
* '''Malignant potential''': Particularly colorectal adenomas that can transform into colorectal cancer. | * '''Malignant potential''': Particularly colorectal adenomas that can transform into colorectal cancer. | ||
| Line 41: | Line 64: | ||
[[File:Histopathology of adrenocortical adenoma.jpg|alt=Histopathology of adrenocortical adenoma|thumb|Histopathology of adrenocortical adenoma]] | [[File:Histopathology of adrenocortical adenoma.jpg|alt=Histopathology of adrenocortical adenoma|thumb|Histopathology of adrenocortical adenoma]] | ||
Occur in adrenal cortex; may produce hormones (e.g., cortisol or aldosterone): | Occur in adrenal cortex; may produce hormones (e.g., cortisol or aldosterone): | ||
* Functioning adenomas ([[ | * Functioning adenomas ([[Cushing’s syndrome]], [[Conn’s syndrome]]) | ||
=== Hepatic Adenomas === | === Hepatic Adenomas === | ||
Benign liver tumors associated with oral contraceptive use; risk of hemorrhage or malignant transformation. | Benign liver tumors associated with oral contraceptive use; risk of hemorrhage or malignant transformation. | ||
| Line 60: | Line 83: | ||
* '''Pituitary adenomas''': Vision changes, hormonal imbalance | * '''Pituitary adenomas''': Vision changes, hormonal imbalance | ||
* '''Thyroid adenomas''': Hyperthyroidism, neck lump | * '''Thyroid adenomas''': Hyperthyroidism, neck lump | ||
* '''Adrenal adenomas''': | * '''Adrenal adenomas''': Cushing’s or Conn’s syndrome | ||
* '''Hepatic adenomas''': Abdominal pain, risk of bleeding | * '''Hepatic adenomas''': Abdominal pain, risk of bleeding | ||
* '''Renal adenomas''': Usually asymptomatic | * '''Renal adenomas''': Usually asymptomatic | ||
| Line 96: | Line 119: | ||
* [[Multiple endocrine neoplasia]] | * [[Multiple endocrine neoplasia]] | ||
== External links == | == External links == | ||
[https://www.cancer.org American Cancer Society | [https://www.cancer.org American Cancer Society – Adenomas] | ||
[https://rarediseases.info.nih.gov Genetic and Rare Diseases Information Center (GARD)] | [https://rarediseases.info.nih.gov Genetic and Rare Diseases Information Center (GARD)] | ||
{{Tumors}} {{Endocrine disorders}} [[Category:Benign tumors]] [[Category:Gastrointestinal disorders]] [[Category:Endocrinology]] [[Category:Oncology]] [[Category:Hepatology]] [[Category:Neuroscience]] [[Category:Anatomical pathology]] [[Category:Glandular and epithelial neoplasia]] {{stub}} | {{Tumors}} {{Endocrine disorders}} [[Category:Benign tumors]] [[Category:Gastrointestinal disorders]] [[Category:Endocrinology]] [[Category:Oncology]] [[Category:Hepatology]] [[Category:Neuroscience]] [[Category:Anatomical pathology]] [[Category:Glandular and epithelial neoplasia]] {{stub}} | ||
Latest revision as of 05:08, 4 April 2025
| Adenoma | |
|---|---|
| |
| Synonyms | |
| Pronounce | N/A |
| Specialty | N/A |
| Symptoms | Often asymptomatic, may cause hormonal imbalance if functional |
| Complications | Potential progression to adenocarcinoma |
| Onset | Varies depending on type and location |
| Duration | Indeterminate, may remain stable or progress |
| Types | Tubular adenoma, villous adenoma, tubulovillous adenoma |
| Causes | Genetic mutations, environmental factors |
| Risks | Age, family history, diet, smoking |
| Diagnosis | Biopsy, endoscopy, imaging studies |
| Differential diagnosis | Hyperplasia, adenocarcinoma, polyp |
| Prevention | Regular screening, healthy diet, avoiding smoking |
| Treatment | Surgical removal, endoscopic resection |
| Medication | None specific, may use hormonal therapy if functional |
| Prognosis | Generally good if benign, risk of malignancy varies |
| Frequency | Common, varies by type and location |
| Deaths | Rare, unless progresses to malignancy |
Benign glandular tumors with potential malignant transformation
| Adenoma | |
|---|---|

| |
| Synonyms | Adenomatous tumor |
| Pronounce | |
| Field | Oncology, Pathology, Endocrinology, Gastroenterology |
| Symptoms | Often asymptomatic; may cause hormonal imbalance, obstruction, pain |
| Complications | Malignant transformation, bleeding, organ dysfunction |
| Onset | Variable; often detected in adults |
| Duration | Chronic (often lifelong surveillance required) |
| Types | Colorectal, pituitary, thyroid, adrenal, hepatic, renal, sebaceous |
| Causes | Genetic mutations, hormonal imbalance, environmental factors |
| Risks | Age, genetics, obesity, hormonal therapy, radiation exposure |
| Diagnosis | Clinical evaluation, imaging, laboratory tests, biopsy |
| Differential diagnosis | Hyperplastic polyps, adenocarcinoma, neuroendocrine tumors |
| Prevention | Lifestyle modifications, genetic screening |
| Treatment | Surveillance, endoscopic removal, surgical excision, medical therapy |
| Medication | Hormone suppressants, antithyroid medications, dopamine agonists |
| Prognosis | Generally good; dependent on type, size, and malignant risk |
| Frequency | Common (colorectal adenomas); other types vary |
| Deaths | Rare, usually due to malignant transformation or complications |
Adenoma is a type of benign tumor originating from glandular epithelial cells. Although adenomas themselves are benign, some possess the potential to progress into malignant tumors (adenocarcinoma). They commonly affect various glandular organs, including the colon, pituitary gland, thyroid gland, adrenal gland, liver, and kidney. Understanding their characteristics, potential complications, and management strategies is vital for early detection and treatment.
Definition and Characteristics[edit]
An adenoma arises from glandular epithelial tissue, forming a well-defined, localized mass. Despite their benign nature, adenomas can cause complications by:
- Compressing nearby structures (mass effect)
- Producing excess hormones (functional adenomas)
- Potentially transforming into malignant adenocarcinoma (notably colorectal adenomas)
Epidemiology[edit]
The frequency and clinical significance of adenomas vary by organ:
- Colorectal adenomas: Common in adults >50 years; precursors to colorectal cancer.
- Pituitary adenomas: Account for 10–15% of intracranial tumors.
- Thyroid adenomas: Frequent in women; detected as thyroid nodules.
- Hepatic adenomas: Rare; linked to oral contraceptive use.
Clinical Significance[edit]
Adenomas can significantly impact health due to:
- Hormonal imbalance: Functional adenomas can cause endocrine disorders (e.g., Cushing’s syndrome, hyperthyroidism).
- Obstruction: Large adenomas in the colon may cause bowel obstruction.
- Malignant potential: Particularly colorectal adenomas that can transform into colorectal cancer.
- Early identification and management are essential to reduce morbidity.
Types of Adenomas[edit]
Adenomas vary by anatomical location and behavior:
Colorectal Adenomas[edit]

Common precursors to colorectal cancer; subtypes include:
Pituitary Adenomas[edit]
Arise in the pituitary gland; subtypes include:
- Prolactinoma
- Growth hormone-secreting adenoma
- ACTH-secreting adenoma
- Non-functioning adenomas
Thyroid Adenomas[edit]

Often solitary nodules arising from follicular cells; subtypes include:
Adrenal Adenomas[edit]

Occur in adrenal cortex; may produce hormones (e.g., cortisol or aldosterone):
- Functioning adenomas (Cushing’s syndrome, Conn’s syndrome)
Hepatic Adenomas[edit]
Benign liver tumors associated with oral contraceptive use; risk of hemorrhage or malignant transformation.
Renal Adenomas[edit]
Small benign kidney tumors; usually incidental findings.
Sebaceous Adenomas[edit]
Associated with sebaceous glands; linked to Muir-Torre syndrome.
Causes and Risk Factors[edit]

Adenomas develop due to genetic mutations, hormonal disturbances, and environmental factors:
- Genetic conditions (e.g., Familial adenomatous polyposis, Multiple endocrine neoplasia)
- Hormonal imbalances (pituitary, thyroid, adrenal adenomas)
- Diet and obesity (colorectal adenomas)
- Oral contraceptives (hepatic adenomas)
- Radiation exposure (thyroid adenomas)
Symptoms and Complications[edit]
Symptoms depend on adenoma location and hormone secretion:
- Colorectal adenomas: Rectal bleeding, bowel habit changes
- Pituitary adenomas: Vision changes, hormonal imbalance
- Thyroid adenomas: Hyperthyroidism, neck lump
- Adrenal adenomas: Cushing’s or Conn’s syndrome
- Hepatic adenomas: Abdominal pain, risk of bleeding
- Renal adenomas: Usually asymptomatic
Complications include malignant transformation, organ obstruction, hormonal disturbances, and bleeding.
Diagnosis[edit]

Diagnosis involves:
- Clinical evaluation: History, physical exam
- Imaging: Colonoscopy, ultrasound, MRI, CT
- Laboratory tests: Hormone levels, tumor markers
- Histopathology: Biopsy confirms diagnosis
Treatment and Management[edit]
Treatment varies by adenoma type and risk factors:
- Observation: Small, asymptomatic adenomas
- Endoscopic removal: Colorectal polyps
- Surgical excision: Large or high-risk adenomas
- Medical therapy: Hormone-suppressing medications for pituitary and adrenal adenomas
Long-term monitoring is often required due to recurrence risk.
Prognosis[edit]
Prognosis depends on adenoma type and malignant potential:
- Generally favorable with early detection and treatment
- High-risk adenomas require ongoing surveillance to prevent cancer progression
Prevention[edit]
Preventive strategies include lifestyle modifications, regular screenings (colonoscopy), genetic counseling, and hormonal regulation.
Gallery[edit]
-
Traditional serrated adenoma histopathology
-
Adenoma-carcinoma progression diagram
See also[edit]
External links[edit]
American Cancer Society – Adenomas Genetic and Rare Diseases Information Center (GARD)
| Overview of tumors, cancer and oncology | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| Endocrine disorders | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
This endocrine disorder-related article is a stub.
|



