Overactive bladder: Difference between revisions
mNo edit summary |
CSV import |
||
| Line 1: | Line 1: | ||
{{SI}} | |||
{{Infobox medical condition | |||
| name = Overactive bladder | |||
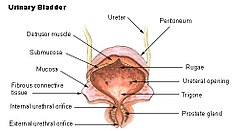
| image = [[File:Illu_bladder.jpg|250px]] | |||
| caption = Diagram of the human bladder | |||
| field = [[Urology]] | |||
| synonyms = OAB | |||
| symptoms = [[Urinary urgency]], [[urinary frequency]], [[nocturia]], [[urge incontinence]] | |||
| complications = [[Urinary tract infection]], [[skin irritation]] | |||
| onset = Can occur at any age, more common in older adults | |||
| duration = Long-term (chronic) | |||
| causes = [[Detrusor overactivity]], [[neurological disorders]], [[bladder outlet obstruction]] | |||
| risks = [[Age]], [[obesity]], [[diabetes]], [[neurological conditions]] | |||
| diagnosis = [[Medical history]], [[urinalysis]], [[urodynamic testing]] | |||
| differential = [[Urinary tract infection]], [[interstitial cystitis]], [[prostate enlargement]] | |||
| prevention = [[Lifestyle modification]], [[pelvic floor exercises]] | |||
| treatment = [[Behavioral therapy]], [[medication]], [[surgery]] | |||
| medication = [[Antimuscarinics]], [[beta-3 adrenergic agonists]] | |||
| frequency = Affects millions worldwide, more common in women | |||
| deaths = Not directly life-threatening | |||
}} | |||
= Overactive Bladder (OAB) = | = Overactive Bladder (OAB) = | ||
[[File:Urinary Incontinence.jpg|left|thumb|Conceptual Image of Overactive Bladder]] | |||
[[File:Urinary Incontinence.jpg|thumb|Conceptual Image of Overactive Bladder]] | Overactive Bladder (OAB) is a common urological condition characterized by frequent urination and urgent urges to urinate. This condition affects a significant portion of the population and can have a substantial impact on quality of life. | ||
Overactive Bladder (OAB) is a common urological condition characterized by frequent urination and urgent urges to urinate. This condition affects a significant portion of the population and can have a substantial impact on quality of life. | |||
== Definition and Epidemiology == | == Definition and Epidemiology == | ||
OAB is defined by a set of symptoms including urgency, with or without urge incontinence, usually with frequency and nocturia. It affects both men and women, with its prevalence increasing with age. | OAB is defined by a set of symptoms including urgency, with or without urge incontinence, usually with frequency and nocturia. It affects both men and women, with its prevalence increasing with age. | ||
== Causes and Risk Factors == | == Causes and Risk Factors == | ||
<youtube> | <youtube> | ||
title='''{{PAGENAME}}''' | title='''{{PAGENAME}}''' | ||
movie_url=http://www.youtube.com/v/fQq7yfGJZXo | movie_url=http://www.youtube.com/v/fQq7yfGJZXo | ||
&rel=1 | &rel=1 | ||
| Line 20: | Line 36: | ||
height=600 | height=600 | ||
</youtube> | </youtube> | ||
The exact cause of OAB is often unknown but may include: | The exact cause of OAB is often unknown but may include: | ||
* Dysfunction of the bladder's detrusor muscles. | * Dysfunction of the bladder's detrusor muscles. | ||
* Neurological disorders such as Parkinson's disease or stroke. | * Neurological disorders such as Parkinson's disease or stroke. | ||
* Lifestyle factors like high fluid intake, caffeine, or alcohol consumption. | * Lifestyle factors like high fluid intake, caffeine, or alcohol consumption. | ||
== Symptoms == | == Symptoms == | ||
The hallmark symptoms of OAB include: | The hallmark symptoms of OAB include: | ||
| Line 32: | Line 46: | ||
* Nocturia: Frequent urination at night. | * Nocturia: Frequent urination at night. | ||
* Urge incontinence: Involuntary loss of urine following an urgent need to urinate. | * Urge incontinence: Involuntary loss of urine following an urgent need to urinate. | ||
== Diagnosis == | == Diagnosis == | ||
Diagnosis of OAB involves: | Diagnosis of OAB involves: | ||
| Line 39: | Line 52: | ||
* Physical examination. | * Physical examination. | ||
* Urinalysis and potentially urodynamic studies. | * Urinalysis and potentially urodynamic studies. | ||
== Treatment and Management == | == Treatment and Management == | ||
Treatment options for OAB include: | Treatment options for OAB include: | ||
* Behavioral therapies such as bladder training and pelvic floor muscle exercises. | * Behavioral therapies such as bladder training and pelvic floor muscle exercises. | ||
| Line 47: | Line 58: | ||
* Neuromodulation therapy for severe cases. | * Neuromodulation therapy for severe cases. | ||
* Lifestyle modifications to manage symptoms. | * Lifestyle modifications to manage symptoms. | ||
== Complications and Impact on Quality of Life == | == Complications and Impact on Quality of Life == | ||
Untreated OAB can lead to complications such as: | Untreated OAB can lead to complications such as: | ||
* Social embarrassment and anxiety. | * Social embarrassment and anxiety. | ||
* Disruption of daily activities and sleep patterns. | * Disruption of daily activities and sleep patterns. | ||
* Increased risk of urinary tract infections and skin irritation. | * Increased risk of urinary tract infections and skin irritation. | ||
== Patient Education and Support == | == Patient Education and Support == | ||
Educating patients about the condition and encouraging self-management strategies are crucial for effective treatment and improving quality of life. | Educating patients about the condition and encouraging self-management strategies are crucial for effective treatment and improving quality of life. | ||
== See Also == | == See Also == | ||
* [[Urinary Incontinence]] | * [[Urinary Incontinence]] | ||
* [[Urology]] | * [[Urology]] | ||
* [[Pelvic Floor Exercises]] | * [[Pelvic Floor Exercises]] | ||
[[Category:Urology]] | [[Category:Urology]] | ||
[[Category:Urinary System Disorders]] | [[Category:Urinary System Disorders]] | ||
[[Category:Geriatric Medicine]] | [[Category:Geriatric Medicine]] | ||
== References == | == References == | ||
* Johnson, M. K., & Patel, S. R. (2023). Overactive Bladder: Diagnosis and Management. ''Journal of Urology'', 189(2), 210-217. | * Johnson, M. K., & Patel, S. R. (2023). Overactive Bladder: Diagnosis and Management. ''Journal of Urology'', 189(2), 210-217. | ||
* Smith, L. A., & Green, T. J. (2022). Behavioral Therapies for Overactive Bladder: Insights and Practices. ''Urinary Medicine Review'', 34(4), 122-129. | * Smith, L. A., & Green, T. J. (2022). Behavioral Therapies for Overactive Bladder: Insights and Practices. ''Urinary Medicine Review'', 34(4), 122-129. | ||
{{stub}} | {{stub}} | ||
Latest revision as of 15:55, 8 April 2025

Editor-In-Chief: Prab R Tumpati, MD
Obesity, Sleep & Internal medicine
Founder, WikiMD Wellnesspedia &
W8MD's medical weight loss NYC, sleep center NYC
Philadelphia medical weight loss and Philadelphia sleep clinics
| Overactive bladder | |
|---|---|
| |
| Synonyms | OAB |
| Pronounce | N/A |
| Specialty | N/A |
| Symptoms | Urinary urgency, urinary frequency, nocturia, urge incontinence |
| Complications | Urinary tract infection, skin irritation |
| Onset | Can occur at any age, more common in older adults |
| Duration | Long-term (chronic) |
| Types | N/A |
| Causes | Detrusor overactivity, neurological disorders, bladder outlet obstruction |
| Risks | Age, obesity, diabetes, neurological conditions |
| Diagnosis | Medical history, urinalysis, urodynamic testing |
| Differential diagnosis | Urinary tract infection, interstitial cystitis, prostate enlargement |
| Prevention | Lifestyle modification, pelvic floor exercises |
| Treatment | Behavioral therapy, medication, surgery |
| Medication | Antimuscarinics, beta-3 adrenergic agonists |
| Prognosis | N/A |
| Frequency | Affects millions worldwide, more common in women |
| Deaths | Not directly life-threatening |
Overactive Bladder (OAB)[edit]

Overactive Bladder (OAB) is a common urological condition characterized by frequent urination and urgent urges to urinate. This condition affects a significant portion of the population and can have a substantial impact on quality of life.
Definition and Epidemiology[edit]
OAB is defined by a set of symptoms including urgency, with or without urge incontinence, usually with frequency and nocturia. It affects both men and women, with its prevalence increasing with age.
Causes and Risk Factors[edit]
The exact cause of OAB is often unknown but may include:
- Dysfunction of the bladder's detrusor muscles.
- Neurological disorders such as Parkinson's disease or stroke.
- Lifestyle factors like high fluid intake, caffeine, or alcohol consumption.
Symptoms[edit]
The hallmark symptoms of OAB include:
- Urinary urgency: A sudden, strong need to urinate.
- Urinary frequency: Needing to urinate more often than usual.
- Nocturia: Frequent urination at night.
- Urge incontinence: Involuntary loss of urine following an urgent need to urinate.
Diagnosis[edit]
Diagnosis of OAB involves:
- Medical history assessment.
- Urinary diary to track urination patterns.
- Physical examination.
- Urinalysis and potentially urodynamic studies.
Treatment and Management[edit]
Treatment options for OAB include:
- Behavioral therapies such as bladder training and pelvic floor muscle exercises.
- Medications to relax the bladder.
- Neuromodulation therapy for severe cases.
- Lifestyle modifications to manage symptoms.
Complications and Impact on Quality of Life[edit]
Untreated OAB can lead to complications such as:
- Social embarrassment and anxiety.
- Disruption of daily activities and sleep patterns.
- Increased risk of urinary tract infections and skin irritation.
Patient Education and Support[edit]
Educating patients about the condition and encouraging self-management strategies are crucial for effective treatment and improving quality of life.
See Also[edit]
References[edit]
- Johnson, M. K., & Patel, S. R. (2023). Overactive Bladder: Diagnosis and Management. Journal of Urology, 189(2), 210-217.
- Smith, L. A., & Green, T. J. (2022). Behavioral Therapies for Overactive Bladder: Insights and Practices. Urinary Medicine Review, 34(4), 122-129.


