Torticollis: Difference between revisions
No edit summary |
CSV import |
||
| Line 1: | Line 1: | ||
{{SI}} | |||
{{Infobox medical condition | |||
| name = Torticollis | |||
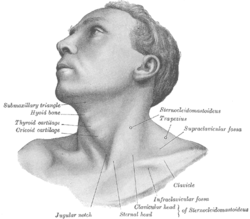
| image = [[File:Gray1194.png|250px]] | |||
| caption = Illustration of the muscles involved in torticollis | |||
| field = [[Neurology]], [[Orthopedics]] | |||
| synonyms = Wry neck, loxia | |||
| symptoms = [[Neck pain]], [[head tilt]], limited range of motion in the neck | |||
| complications = [[Chronic pain]], [[cervical spine]] issues | |||
| onset = Can be [[congenital]] or [[acquired]] | |||
| duration = Varies, can be [[acute]] or [[chronic]] | |||
| causes = [[Muscle spasm]], [[trauma]], [[infection]], [[genetic]] factors | |||
| risks = [[Family history]], [[muscle injury]], [[nerve damage]] | |||
| diagnosis = [[Physical examination]], [[imaging studies]] | |||
| differential = [[Cervical dystonia]], [[spasmodic torticollis]], [[congenital muscular torticollis]] | |||
| treatment = [[Physical therapy]], [[medication]], [[surgery]] | |||
| medication = [[Muscle relaxants]], [[analgesics]], [[botulinum toxin]] | |||
| frequency = Common | |||
| deaths = Rare | |||
}} | |||
[[Torticollis]], often known as wry neck, is a medical condition characterized by an abnormal, asymmetrical head or neck position. It typically presents as a noticeable tilt of the head to one side, due to the contraction or shortening of the sternocleidomastoid muscle located on that side of the neck. | [[Torticollis]], often known as wry neck, is a medical condition characterized by an abnormal, asymmetrical head or neck position. It typically presents as a noticeable tilt of the head to one side, due to the contraction or shortening of the sternocleidomastoid muscle located on that side of the neck. | ||
== Classification == | == Classification == | ||
Torticollis can be broadly classified into two categories: | Torticollis can be broadly classified into two categories: | ||
* [[Congenital torticollis]]: This is present at birth and may be due to malpositioning in the womb or birth trauma, causing damage to the neck muscles. | * [[Congenital torticollis]]: This is present at birth and may be due to malpositioning in the womb or birth trauma, causing damage to the neck muscles. | ||
* Acquired torticollis: This appears later in life due to various conditions affecting the neck muscles, nerves, or vertebrae, including injury, [[infections]], or certain medications. | * Acquired torticollis: This appears later in life due to various conditions affecting the neck muscles, nerves, or vertebrae, including injury, [[infections]], or certain medications. | ||
== Pathophysiology == | == Pathophysiology == | ||
In torticollis, the [[sternocleidomastoid muscle]], which extends along the side of the neck from the back of the ear to the collarbone, contracts or shortens. This may be due to genetic or environmental factors in congenital cases, or a response to injury or other medical conditions in acquired cases. | In torticollis, the [[sternocleidomastoid muscle]], which extends along the side of the neck from the back of the ear to the collarbone, contracts or shortens. This may be due to genetic or environmental factors in congenital cases, or a response to injury or other medical conditions in acquired cases. | ||
== Symptoms == | == Symptoms == | ||
The most apparent symptom of torticollis is a tilt of the head to one side, with the chin pointing to the opposite side. Other symptoms can include: | The most apparent symptom of torticollis is a tilt of the head to one side, with the chin pointing to the opposite side. Other symptoms can include: | ||
| Line 16: | Line 33: | ||
* In babies, preference for looking in one direction | * In babies, preference for looking in one direction | ||
== Diagnosis == | == Diagnosis == | ||
Diagnosis of torticollis primarily involves a physical examination, which assesses the head tilt and range of neck movements. In some cases, imaging tests such as [[MRI]] or [[CT scan]]s might be recommended to rule out other conditions or identify underlying causes. | Diagnosis of torticollis primarily involves a physical examination, which assesses the head tilt and range of neck movements. In some cases, imaging tests such as [[MRI]] or [[CT scan]]s might be recommended to rule out other conditions or identify underlying causes. | ||
== Treatment == | == Treatment == | ||
Treatment strategies for torticollis depend on the cause and severity of the condition: | Treatment strategies for torticollis depend on the cause and severity of the condition: | ||
| Line 24: | Line 39: | ||
* Medication: Some cases might require muscle relaxants or botulinum toxin injections to relieve muscle tension. | * Medication: Some cases might require muscle relaxants or botulinum toxin injections to relieve muscle tension. | ||
* Surgery: If conservative treatments are ineffective, particularly in congenital torticollis, surgical release or lengthening of the sternocleidomastoid muscle may be necessary. | * Surgery: If conservative treatments are ineffective, particularly in congenital torticollis, surgical release or lengthening of the sternocleidomastoid muscle may be necessary. | ||
== Prognosis and Complications == | == Prognosis and Complications == | ||
With appropriate treatment, the prognosis for torticollis is generally good, especially in children. However, untreated or severe torticollis can lead to complications such as chronic neck pain, permanent muscle shortening, and psychological impact due to appearance concerns. | With appropriate treatment, the prognosis for torticollis is generally good, especially in children. However, untreated or severe torticollis can lead to complications such as chronic neck pain, permanent muscle shortening, and psychological impact due to appearance concerns. | ||
== References == | == References == | ||
* Cheng JC, Tang SP, Chen TM, Wong MW, Wong EM. The clinical presentation and outcome of treatment of congenital muscular torticollis in infants--a study of 1,086 cases. J Pediatr Surg. 2000;35(7):1091-6. | * Cheng JC, Tang SP, Chen TM, Wong MW, Wong EM. The clinical presentation and outcome of treatment of congenital muscular torticollis in infants--a study of 1,086 cases. J Pediatr Surg. 2000;35(7):1091-6. | ||
Latest revision as of 19:10, 8 April 2025

Editor-In-Chief: Prab R Tumpati, MD
Obesity, Sleep & Internal medicine
Founder, WikiMD Wellnesspedia &
W8MD medical weight loss NYC and sleep center NYC
| Torticollis | |
|---|---|
| |
| Synonyms | Wry neck, loxia |
| Pronounce | N/A |
| Specialty | N/A |
| Symptoms | Neck pain, head tilt, limited range of motion in the neck |
| Complications | Chronic pain, cervical spine issues |
| Onset | Can be congenital or acquired |
| Duration | Varies, can be acute or chronic |
| Types | N/A |
| Causes | Muscle spasm, trauma, infection, genetic factors |
| Risks | Family history, muscle injury, nerve damage |
| Diagnosis | Physical examination, imaging studies |
| Differential diagnosis | Cervical dystonia, spasmodic torticollis, congenital muscular torticollis |
| Prevention | N/A |
| Treatment | Physical therapy, medication, surgery |
| Medication | Muscle relaxants, analgesics, botulinum toxin |
| Prognosis | N/A |
| Frequency | Common |
| Deaths | Rare |
Torticollis, often known as wry neck, is a medical condition characterized by an abnormal, asymmetrical head or neck position. It typically presents as a noticeable tilt of the head to one side, due to the contraction or shortening of the sternocleidomastoid muscle located on that side of the neck.
Classification[edit]
Torticollis can be broadly classified into two categories:
- Congenital torticollis: This is present at birth and may be due to malpositioning in the womb or birth trauma, causing damage to the neck muscles.
- Acquired torticollis: This appears later in life due to various conditions affecting the neck muscles, nerves, or vertebrae, including injury, infections, or certain medications.
Pathophysiology[edit]
In torticollis, the sternocleidomastoid muscle, which extends along the side of the neck from the back of the ear to the collarbone, contracts or shortens. This may be due to genetic or environmental factors in congenital cases, or a response to injury or other medical conditions in acquired cases.
Symptoms[edit]
The most apparent symptom of torticollis is a tilt of the head to one side, with the chin pointing to the opposite side. Other symptoms can include:
- Difficulty turning the head
- Neck pain or stiffness
- Asymmetry of the face and head
- In babies, preference for looking in one direction
Diagnosis[edit]
Diagnosis of torticollis primarily involves a physical examination, which assesses the head tilt and range of neck movements. In some cases, imaging tests such as MRI or CT scans might be recommended to rule out other conditions or identify underlying causes.
Treatment[edit]
Treatment strategies for torticollis depend on the cause and severity of the condition:
- Physical therapy: Stretching exercises help to improve range of motion and strength in the affected muscles.
- Medication: Some cases might require muscle relaxants or botulinum toxin injections to relieve muscle tension.
- Surgery: If conservative treatments are ineffective, particularly in congenital torticollis, surgical release or lengthening of the sternocleidomastoid muscle may be necessary.
Prognosis and Complications[edit]
With appropriate treatment, the prognosis for torticollis is generally good, especially in children. However, untreated or severe torticollis can lead to complications such as chronic neck pain, permanent muscle shortening, and psychological impact due to appearance concerns.
References[edit]
- Cheng JC, Tang SP, Chen TM, Wong MW, Wong EM. The clinical presentation and outcome of treatment of congenital muscular torticollis in infants--a study of 1,086 cases. J Pediatr Surg. 2000;35(7):1091-6.
- Kaplan SL, Coulter C, Sargent B. Physical therapy management of congenital muscular torticollis: a 2018 evidence-based clinical practice guideline from the APTA Academy of Pediatric Physical Therapy. Pediatr Phys Ther. 2018;30(4):240-90.
- Tse DT, Kaste SC, Ragheb J, et al. Isolated congenital hemifacial hyperplasia. Ophthalmology. 1994;101(7):1285-92.
- Simpson GM, Angus JW. A rating scale for extrapyramidal side effects. Acta Psychiatr Scand Suppl. 1970;212:11-9.
|
|
|
| Spinal disease | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|


