Primary hyperparathyroidism: Difference between revisions
CSV import |
CSV import |
||
| Line 1: | Line 1: | ||
{{SI}} | |||
{{Infobox medical condition | |||
| name = Primary hyperparathyroidism | |||
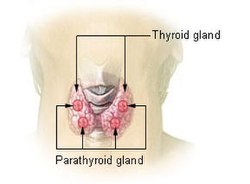
| image = [[File:Illu_thyroid_parathyroid.jpg|250px]] | |||
| caption = Diagram showing the location of the [[parathyroid glands]] | |||
| field = [[Endocrinology]] | |||
| symptoms = [[Hypercalcemia]], [[osteoporosis]], [[kidney stones]], [[depression (mood)|depression]], [[fatigue (medical)|fatigue]] | |||
| complications = [[Osteitis fibrosa cystica]], [[peptic ulcer disease]], [[pancreatitis]] | |||
| onset = Typically [[middle age]] | |||
| duration = Long-term | |||
| causes = [[Parathyroid adenoma]], [[parathyroid hyperplasia]], [[parathyroid carcinoma]] | |||
| risks = [[Radiation therapy]], [[genetic disorders]] such as [[Multiple endocrine neoplasia]] | |||
| diagnosis = [[Blood test]] showing elevated [[calcium]] and [[parathyroid hormone]] levels | |||
| differential = [[Familial hypocalciuric hypercalcemia]], [[tertiary hyperparathyroidism]] | |||
| treatment = [[Surgery]], [[medication]] | |||
| medication = [[Bisphosphonates]], [[calcimimetics]] | |||
| prognosis = Generally good with treatment | |||
| frequency = 1-7 per 1,000 people | |||
| deaths = Rare | |||
}} | |||
Other Names: Hyperparathyroidism, primary | Other Names: Hyperparathyroidism, primary | ||
Primary hyperparathyroidism is a disorder of the parathyroid glands, four pea-sized glands located on or near the thyroid gland in the neck. | Primary hyperparathyroidism is a disorder of the parathyroid glands, four pea-sized glands located on or near the thyroid gland in the neck. “Primary” means this disorder begins in the parathyroid glands, rather than resulting from another health problem such as kidney failure. Hyperfunction of the parathyroid glands resulting in the overproduction of parathyroid hormone. It is caused by parathyroid [[adenoma]], [[parathyroid hyperplasia]], [[parathyroid carcinoma]], and [[multiple endocrine neoplasia]]. It is associated with [[hypercalcemia]] and [[hypophosphatemia]]. | ||
Too much PTH causes calcium levels in your blood to rise too high, which can lead to health problems such as bone thinning and kidney stones. Doctors usually catch primary hyperparathyroidism early through routine blood tests, before serious problems occur. | Too much PTH causes calcium levels in your blood to rise too high, which can lead to health problems such as bone thinning and kidney stones. Doctors usually catch primary hyperparathyroidism early through routine blood tests, before serious problems occur. | ||
<youtube> | <youtube> | ||
title='''{{PAGENAME}}''' | title='''{{PAGENAME}}''' | ||
| Line 15: | Line 32: | ||
height=600 | height=600 | ||
</youtube> | </youtube> | ||
== '''Cause''' == | == '''Cause''' == | ||
In about 8 out of 10 people with primary hyperparathyroidism, a benign, or noncancerous, tumor called an [[adenoma]] has formed in one of the parathyroid glands. The tumor causes the gland to become overactive. In most other cases, extra PTH comes from two or more adenomas or from [[hyperplasia]], a condition in which all four parathyroid glands are enlarged. People with rare inherited conditions that affect the parathyroid glands, such as multiple endocrine neoplasia type 1 or familial hypocalciuric hypercalcemia NIH external link, are more likely to have more than one gland affected. | In about 8 out of 10 people with primary hyperparathyroidism, a benign, or noncancerous, tumor called an [[adenoma]] has formed in one of the parathyroid glands. The tumor causes the gland to become overactive. In most other cases, extra PTH comes from two or more adenomas or from [[hyperplasia]], a condition in which all four parathyroid glands are enlarged. People with rare inherited conditions that affect the parathyroid glands, such as multiple endocrine neoplasia type 1 or familial hypocalciuric hypercalcemia NIH external link, are more likely to have more than one gland affected. | ||
Rarely, primary hyperparathyroidism is caused by cancer of a [[parathyroid gland]]. | Rarely, primary hyperparathyroidism is caused by cancer of a [[parathyroid gland]]. | ||
== '''Riskfactors''' == | == '''Riskfactors''' == | ||
Primary hyperparathyroidism most often affects people between age 50 and 60. Women are affected 3 to 4 times more often than men.The disorder was more common in African Americans, followed by Caucasians, in one large study performed in North America. | Primary hyperparathyroidism most often affects people between age 50 and 60. Women are affected 3 to 4 times more often than men.The disorder was more common in African Americans, followed by Caucasians, in one large study performed in North America. | ||
== '''Complications''' == | == '''Complications''' == | ||
Primary hyperparathyroidism most often affects the bones and kidneys, although it also may play a part in other health problems. | Primary hyperparathyroidism most often affects the bones and kidneys, although it also may play a part in other health problems. | ||
'''Weakened bones''' | '''Weakened bones''' | ||
High PTH levels trigger the bones to release more [[calcium]] than normal into the blood. The loss of calcium from the bones may weaken them. | High PTH levels trigger the bones to release more [[calcium]] than normal into the blood. The loss of calcium from the bones may weaken them. | ||
'''Kidney stones''' | '''Kidney stones''' | ||
The small intestine may absorb more calcium from food, adding to high levels of calcium in your blood. Extra calcium that | The small intestine may absorb more calcium from food, adding to high levels of calcium in your blood. Extra calcium that isn’t used by your bones and muscles goes to your kidneys and is flushed out in urine. Too much calcium in your urine can cause kidney stones. | ||
'''Other complications''' | '''Other complications''' | ||
High blood calcium levels might play a part in other problems, such as heart disease, high blood pressure, and trouble concentrating. However, more research is needed to better understand how primary hyperparathyroidism affects the heart, blood vessels, and brain. | High blood calcium levels might play a part in other problems, such as heart disease, high blood pressure, and trouble concentrating. However, more research is needed to better understand how primary hyperparathyroidism affects the heart, blood vessels, and brain. | ||
== '''Symptoms''' == | == '''Symptoms''' == | ||
Most people with primary hyperparathyroidism have no symptoms. When symptoms appear, | Most people with primary hyperparathyroidism have no symptoms. When symptoms appear, they’re often mild and similar to those of many other disorders. Symptoms include | ||
* muscle weakness | * muscle weakness | ||
* fatigue | * fatigue | ||
* depression NIH external link | * depression NIH external link | ||
* aches and pains in bones and joints. | * aches and pains in bones and joints. | ||
People with more severe disease may have | People with more severe disease may have | ||
* loss of appetite | * loss of appetite | ||
| Line 50: | Line 58: | ||
* confusion | * confusion | ||
* increased thirst and urination | * increased thirst and urination | ||
== '''Diagnosis''' == | == '''Diagnosis''' == | ||
Doctors diagnose primary hyperparathyroidism when a blood test shows high blood [[calcium]] and [[PTH]] levels. Sometimes PTH levels are in the upper portion of the normal range, when they should drop to low-normal or below normal in response to high calcium levels. Other conditions can cause high calcium, but elevated PTH is the only source in primary hyperparathyroidism. | Doctors diagnose primary hyperparathyroidism when a blood test shows high blood [[calcium]] and [[PTH]] levels. Sometimes PTH levels are in the upper portion of the normal range, when they should drop to low-normal or below normal in response to high calcium levels. Other conditions can cause high calcium, but elevated PTH is the only source in primary hyperparathyroidism. | ||
Routine blood tests can detect high blood calcium levels. High blood calcium may cause health care professionals to suspect hyperparathyroidism, even before symptoms appear. | Routine blood tests can detect high blood calcium levels. High blood calcium may cause health care professionals to suspect hyperparathyroidism, even before symptoms appear. | ||
Once doctors diagnose hyperparathyroidism, a 24-hour urine collection can help find the cause. This test measures certain chemicals, such as calcium and [[creatinine]], a waste product that healthy kidneys remove. Results of the test may help tell primary hyperparathyroidism from hyperparathyroidism caused by a kidney disorder. The test can also rule out familial hypocalciuric [[hypercalcemia]], a rare genetic disorder, as a cause. | Once doctors diagnose hyperparathyroidism, a 24-hour urine collection can help find the cause. This test measures certain chemicals, such as calcium and [[creatinine]], a waste product that healthy kidneys remove. Results of the test may help tell primary hyperparathyroidism from hyperparathyroidism caused by a kidney disorder. The test can also rule out familial hypocalciuric [[hypercalcemia]], a rare genetic disorder, as a cause. | ||
Once doctors diagnose primary hyperparathyroidism, they may use other tests to look for bone weakness, kidney problems, and low levels of vitamin D. | Once doctors diagnose primary hyperparathyroidism, they may use other tests to look for bone weakness, kidney problems, and low levels of vitamin D. | ||
* Bone mineral density test | * Bone mineral density test | ||
* [[Kidney imaging tests]] | * [[Kidney imaging tests]] | ||
* Vitamin D blood test:Health care professionals test for [[vitamin D]] levels because low levels are common in people with primary hyperparathyroidism. In patients with primary hyperparathyroidism, the low vitamin D level can further stimulate the parathyroid glands to make even more parathyroid hormone. Also, a very low vitamin D level may cause a secondary form of hyperparathyroidism, which resolves when vitamin D levels are returned to normal. | * Vitamin D blood test:Health care professionals test for [[vitamin D]] levels because low levels are common in people with primary hyperparathyroidism. In patients with primary hyperparathyroidism, the low vitamin D level can further stimulate the parathyroid glands to make even more parathyroid hormone. Also, a very low vitamin D level may cause a secondary form of hyperparathyroidism, which resolves when vitamin D levels are returned to normal. | ||
== '''Treatment''' == | == '''Treatment''' == | ||
Doctors most often recommend parathyroid surgery, particularly if the patient meets one or more of the guidelines noted below. | Doctors most often recommend parathyroid surgery, particularly if the patient meets one or more of the guidelines noted below. | ||
| Line 68: | Line 73: | ||
* A fracture resulting from relatively little force, such as a fall from a standing or sitting position (a fragility fracture) | * A fracture resulting from relatively little force, such as a fall from a standing or sitting position (a fragility fracture) | ||
* Age < 50. | * Age < 50. | ||
'''Surgery''' | '''Surgery''' | ||
Surgery to remove the overactive [[parathyroid gland]] or glands is the only sure way to cure primary hyperparathyroidism. | Surgery to remove the overactive [[parathyroid gland]] or glands is the only sure way to cure primary hyperparathyroidism. | ||
Surgeons use two main types of operations to remove the overactive gland or glands. | Surgeons use two main types of operations to remove the overactive gland or glands. | ||
Minimally invasive [[parathyroidectomy]]. Also called focused parathyroidectomy, surgeons use this type of surgery when they think only one of the parathyroid glands is overactive. Guided by a tumor-imaging test, your surgeon will make a small incision, or cut, in your neck to remove the gland. The small incision means you will probably have less pain and a faster recovery than people who have more invasive surgery. You can go home the same day. Your doctor may use regional or general anesthesia NIH external link during the surgery. | Minimally invasive [[parathyroidectomy]]. Also called focused parathyroidectomy, surgeons use this type of surgery when they think only one of the parathyroid glands is overactive. Guided by a tumor-imaging test, your surgeon will make a small incision, or cut, in your neck to remove the gland. The small incision means you will probably have less pain and a faster recovery than people who have more invasive surgery. You can go home the same day. Your doctor may use regional or general anesthesia NIH external link during the surgery. | ||
Bilateral neck exploration. This type of surgery uses a larger incision that lets the surgeon find and look at all four parathyroid glands and remove the overactive ones. If you have bilateral neck exploration, you will probably have general anesthesia and may need to stay in the hospital overnight. | Bilateral neck exploration. This type of surgery uses a larger incision that lets the surgeon find and look at all four parathyroid glands and remove the overactive ones. If you have bilateral neck exploration, you will probably have general anesthesia and may need to stay in the hospital overnight. | ||
[[Cinacalcet]] is a medicine that decreases the amount of PTH the parathyroid glands make and lowers calcium levels in the blood. Doctors may prescribe cinacalcet to treat very high calcium levels in people with primary hyperparathyroidism who | [[Cinacalcet]] is a medicine that decreases the amount of PTH the parathyroid glands make and lowers calcium levels in the blood. Doctors may prescribe cinacalcet to treat very high calcium levels in people with primary hyperparathyroidism who can’t have surgery. | ||
Cinacalcet does not improve bone density. If you have bone loss, your doctor may prescribe [[alendronate]] NIH external link or other medications to help increase bone density. | Cinacalcet does not improve bone density. If you have bone loss, your doctor may prescribe [[alendronate]] NIH external link or other medications to help increase bone density. | ||
The medication(s) listed below have been approved by the Food and Drug Administration (FDA) as orphan products for treatment of this condition. | The medication(s) listed below have been approved by the Food and Drug Administration (FDA) as orphan products for treatment of this condition. | ||
* '''[[Cinacalcet]]''' (Brand name: | * '''[[Cinacalcet]]''' (Brand name: Sensipar®) Treatment of hypercalcemia in adult patients with primary hyperparathyroidism for whom parathyroidectomy would be indicated on the basis of serum calcium levels, but who are unable to undergo parathyroidectomy. | ||
== '''Epidemiology''' == | == '''Epidemiology''' == | ||
In the United States, about 100,000 people develop primary hyperparathyroidism each year.1 Primary hyperparathyroidism is one of the most common hormonal disorders. | In the United States, about 100,000 people develop primary hyperparathyroidism each year.1 Primary hyperparathyroidism is one of the most common hormonal disorders. | ||
{{DEFAULTSORT:Primary Hyperparathyroidism}} | {{DEFAULTSORT:Primary Hyperparathyroidism}} | ||
[[Category:Parathyroid disorders]] | [[Category:Parathyroid disorders]] | ||
{{rarediseases}} | {{rarediseases}} | ||
{{stub}} | {{stub}} | ||
Latest revision as of 22:17, 6 April 2025

Editor-In-Chief: Prab R Tumpati, MD
Obesity, Sleep & Internal medicine
Founder, WikiMD Wellnesspedia &
W8MD medical weight loss NYC and sleep center NYC
| Primary hyperparathyroidism | |
|---|---|
| |
| Synonyms | N/A |
| Pronounce | N/A |
| Specialty | N/A |
| Symptoms | Hypercalcemia, osteoporosis, kidney stones, depression, fatigue |
| Complications | Osteitis fibrosa cystica, peptic ulcer disease, pancreatitis |
| Onset | Typically middle age |
| Duration | Long-term |
| Types | N/A |
| Causes | Parathyroid adenoma, parathyroid hyperplasia, parathyroid carcinoma |
| Risks | Radiation therapy, genetic disorders such as Multiple endocrine neoplasia |
| Diagnosis | Blood test showing elevated calcium and parathyroid hormone levels |
| Differential diagnosis | Familial hypocalciuric hypercalcemia, tertiary hyperparathyroidism |
| Prevention | N/A |
| Treatment | Surgery, medication |
| Medication | Bisphosphonates, calcimimetics |
| Prognosis | Generally good with treatment |
| Frequency | 1-7 per 1,000 people |
| Deaths | Rare |
Other Names: Hyperparathyroidism, primary
Primary hyperparathyroidism is a disorder of the parathyroid glands, four pea-sized glands located on or near the thyroid gland in the neck. “Primary” means this disorder begins in the parathyroid glands, rather than resulting from another health problem such as kidney failure. Hyperfunction of the parathyroid glands resulting in the overproduction of parathyroid hormone. It is caused by parathyroid adenoma, parathyroid hyperplasia, parathyroid carcinoma, and multiple endocrine neoplasia. It is associated with hypercalcemia and hypophosphatemia.
Too much PTH causes calcium levels in your blood to rise too high, which can lead to health problems such as bone thinning and kidney stones. Doctors usually catch primary hyperparathyroidism early through routine blood tests, before serious problems occur.
Cause[edit]
In about 8 out of 10 people with primary hyperparathyroidism, a benign, or noncancerous, tumor called an adenoma has formed in one of the parathyroid glands. The tumor causes the gland to become overactive. In most other cases, extra PTH comes from two or more adenomas or from hyperplasia, a condition in which all four parathyroid glands are enlarged. People with rare inherited conditions that affect the parathyroid glands, such as multiple endocrine neoplasia type 1 or familial hypocalciuric hypercalcemia NIH external link, are more likely to have more than one gland affected. Rarely, primary hyperparathyroidism is caused by cancer of a parathyroid gland.
Riskfactors[edit]
Primary hyperparathyroidism most often affects people between age 50 and 60. Women are affected 3 to 4 times more often than men.The disorder was more common in African Americans, followed by Caucasians, in one large study performed in North America.
Complications[edit]
Primary hyperparathyroidism most often affects the bones and kidneys, although it also may play a part in other health problems. Weakened bones High PTH levels trigger the bones to release more calcium than normal into the blood. The loss of calcium from the bones may weaken them. Kidney stones The small intestine may absorb more calcium from food, adding to high levels of calcium in your blood. Extra calcium that isn’t used by your bones and muscles goes to your kidneys and is flushed out in urine. Too much calcium in your urine can cause kidney stones. Other complications High blood calcium levels might play a part in other problems, such as heart disease, high blood pressure, and trouble concentrating. However, more research is needed to better understand how primary hyperparathyroidism affects the heart, blood vessels, and brain.
Symptoms[edit]
Most people with primary hyperparathyroidism have no symptoms. When symptoms appear, they’re often mild and similar to those of many other disorders. Symptoms include
- muscle weakness
- fatigue
- depression NIH external link
- aches and pains in bones and joints.
People with more severe disease may have
- loss of appetite
- nausea
- vomiting
- constipation
- confusion
- increased thirst and urination
Diagnosis[edit]
Doctors diagnose primary hyperparathyroidism when a blood test shows high blood calcium and PTH levels. Sometimes PTH levels are in the upper portion of the normal range, when they should drop to low-normal or below normal in response to high calcium levels. Other conditions can cause high calcium, but elevated PTH is the only source in primary hyperparathyroidism. Routine blood tests can detect high blood calcium levels. High blood calcium may cause health care professionals to suspect hyperparathyroidism, even before symptoms appear. Once doctors diagnose hyperparathyroidism, a 24-hour urine collection can help find the cause. This test measures certain chemicals, such as calcium and creatinine, a waste product that healthy kidneys remove. Results of the test may help tell primary hyperparathyroidism from hyperparathyroidism caused by a kidney disorder. The test can also rule out familial hypocalciuric hypercalcemia, a rare genetic disorder, as a cause. Once doctors diagnose primary hyperparathyroidism, they may use other tests to look for bone weakness, kidney problems, and low levels of vitamin D.
- Bone mineral density test
- Kidney imaging tests
- Vitamin D blood test:Health care professionals test for vitamin D levels because low levels are common in people with primary hyperparathyroidism. In patients with primary hyperparathyroidism, the low vitamin D level can further stimulate the parathyroid glands to make even more parathyroid hormone. Also, a very low vitamin D level may cause a secondary form of hyperparathyroidism, which resolves when vitamin D levels are returned to normal.
Treatment[edit]
Doctors most often recommend parathyroid surgery, particularly if the patient meets one or more of the guidelines noted below.
- Blood calcium > 1 mg/dL above normal
- Bone density by DXA < -2.5 at any site (lumbar spine, hip, or forearm)
- History of kidney stones or evidence of kidney stones or calcifications in the kidney by imaging (e.g., X-ray, ultrasound, CT scan). Evidence for stone risk by 24-hour urine with excessive calcium and other stone risk factors.
- A fracture resulting from relatively little force, such as a fall from a standing or sitting position (a fragility fracture)
- Age < 50.
Surgery Surgery to remove the overactive parathyroid gland or glands is the only sure way to cure primary hyperparathyroidism. Surgeons use two main types of operations to remove the overactive gland or glands. Minimally invasive parathyroidectomy. Also called focused parathyroidectomy, surgeons use this type of surgery when they think only one of the parathyroid glands is overactive. Guided by a tumor-imaging test, your surgeon will make a small incision, or cut, in your neck to remove the gland. The small incision means you will probably have less pain and a faster recovery than people who have more invasive surgery. You can go home the same day. Your doctor may use regional or general anesthesia NIH external link during the surgery. Bilateral neck exploration. This type of surgery uses a larger incision that lets the surgeon find and look at all four parathyroid glands and remove the overactive ones. If you have bilateral neck exploration, you will probably have general anesthesia and may need to stay in the hospital overnight. Cinacalcet is a medicine that decreases the amount of PTH the parathyroid glands make and lowers calcium levels in the blood. Doctors may prescribe cinacalcet to treat very high calcium levels in people with primary hyperparathyroidism who can’t have surgery. Cinacalcet does not improve bone density. If you have bone loss, your doctor may prescribe alendronate NIH external link or other medications to help increase bone density. The medication(s) listed below have been approved by the Food and Drug Administration (FDA) as orphan products for treatment of this condition.
- Cinacalcet (Brand name: Sensipar®) Treatment of hypercalcemia in adult patients with primary hyperparathyroidism for whom parathyroidectomy would be indicated on the basis of serum calcium levels, but who are unable to undergo parathyroidectomy.
Epidemiology[edit]
In the United States, about 100,000 people develop primary hyperparathyroidism each year.1 Primary hyperparathyroidism is one of the most common hormonal disorders.
NIH genetic and rare disease info[edit]
Primary hyperparathyroidism is a rare disease.
| Rare and genetic diseases | ||||||
|---|---|---|---|---|---|---|
|
Rare diseases - Primary hyperparathyroidism
|


