Bonnet–Dechaume–Blanc syndrome: Difference between revisions
CSV import Tag: Removed redirect |
CSV import |
||
| Line 1: | Line 1: | ||
{{SI}} | |||
{{Infobox medical condition | |||
| name = Bonnet–Dechaume–Blanc syndrome | |||
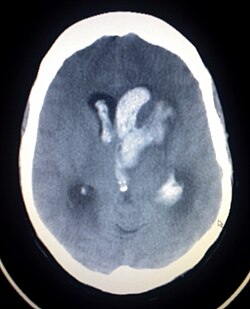
| image = [[File:Intracerebral_hemorrage_(CT_scan).jpg|250px]] | |||
| caption = CT scan showing [[intracerebral hemorrhage]], a possible complication of Bonnet–Dechaume–Blanc syndrome | |||
| synonyms = Wyburn-Mason syndrome | |||
| specialty = [[Neurology]], [[Ophthalmology]] | |||
| symptoms = [[Arteriovenous malformation]]s in the [[retina]], [[midbrain]], and [[facial skin]] | |||
| complications = [[Intracerebral hemorrhage]], [[seizures]], [[vision loss]] | |||
| onset = [[Congenital]] | |||
| duration = [[Lifelong]] | |||
| causes = [[Genetic mutation]] | |||
| risks = [[Family history]] | |||
| diagnosis = [[Clinical examination]], [[MRI]], [[CT scan]] | |||
| differential = [[Sturge-Weber syndrome]], [[Von Hippel-Lindau disease]] | |||
| treatment = [[Surgical intervention]], [[radiotherapy]], [[laser therapy]] | |||
| prognosis = Variable, depending on severity and complications | |||
| frequency = Rare | |||
}} | |||
{{Short description|A rare congenital disorder affecting the eyes and brain}} | {{Short description|A rare congenital disorder affecting the eyes and brain}} | ||
'''Bonnet–Dechaume–Blanc syndrome''' (BDBS), also known as '''Wyburn-Mason syndrome''', is a rare congenital disorder characterized by arteriovenous malformations (AVMs) that primarily affect the [[retina]] and the [[brain]]. This condition is part of the [[phakomatoses]] group of disorders, which are neurocutaneous syndromes involving the [[central nervous system]] and the skin. | '''Bonnet–Dechaume–Blanc syndrome''' (BDBS), also known as '''Wyburn-Mason syndrome''', is a rare congenital disorder characterized by arteriovenous malformations (AVMs) that primarily affect the [[retina]] and the [[brain]]. This condition is part of the [[phakomatoses]] group of disorders, which are neurocutaneous syndromes involving the [[central nervous system]] and the skin. | ||
==Presentation== | ==Presentation== | ||
BDBS is typically identified by the presence of AVMs in the [[retina]] and the [[cerebral]] vasculature. These malformations can lead to a variety of symptoms depending on their size and location. | BDBS is typically identified by the presence of AVMs in the [[retina]] and the [[cerebral]] vasculature. These malformations can lead to a variety of symptoms depending on their size and location. | ||
===Ocular Manifestations=== | ===Ocular Manifestations=== | ||
[[File:406907P-PA-OCULAR.jpg|Ocular manifestations of BDBS|thumb | [[File:406907P-PA-OCULAR.jpg|Ocular manifestations of BDBS|left|thumb]] | ||
The ocular manifestations of BDBS include retinal AVMs, which can be detected through [[ophthalmoscopy]] or [[fluorescein angiography]]. These AVMs may cause visual disturbances such as decreased [[visual acuity]], [[visual field]] defects, or even [[retinal detachment]]. | The ocular manifestations of BDBS include retinal AVMs, which can be detected through [[ophthalmoscopy]] or [[fluorescein angiography]]. These AVMs may cause visual disturbances such as decreased [[visual acuity]], [[visual field]] defects, or even [[retinal detachment]]. | ||
===Neurological Manifestations=== | ===Neurological Manifestations=== | ||
[[File:Intracerebral_hemorrage_(CT_scan).jpg|Intracerebral hemorrhage in BDBS|thumb | [[File:Intracerebral_hemorrage_(CT_scan).jpg|Intracerebral hemorrhage in BDBS|left|thumb]] | ||
Neurologically, patients may present with symptoms due to cerebral AVMs, such as [[headaches]], [[seizures]], or [[intracerebral hemorrhage]]. The location of the AVMs in the brain can lead to specific neurological deficits, including [[hemiparesis]] or [[aphasia]]. | Neurologically, patients may present with symptoms due to cerebral AVMs, such as [[headaches]], [[seizures]], or [[intracerebral hemorrhage]]. The location of the AVMs in the brain can lead to specific neurological deficits, including [[hemiparesis]] or [[aphasia]]. | ||
===Visual Field Defects=== | ===Visual Field Defects=== | ||
[[File:Visual_field_homonymous_hemianopia.png|Visual field defect in BDBS|thumb | [[File:Visual_field_homonymous_hemianopia.png|Visual field defect in BDBS|left|thumb]] | ||
Patients with BDBS may experience visual field defects such as [[homonymous hemianopia]], which is a loss of half of the field of view on the same side in both eyes. This occurs due to the involvement of the visual pathways in the brain. | Patients with BDBS may experience visual field defects such as [[homonymous hemianopia]], which is a loss of half of the field of view on the same side in both eyes. This occurs due to the involvement of the visual pathways in the brain. | ||
==Pathophysiology== | ==Pathophysiology== | ||
The exact cause of BDBS is not well understood, but it is believed to result from developmental anomalies in the embryonic vasculature. The AVMs are thought to arise from a failure of the normal regression of embryonic vascular connections, leading to direct arterial-to-venous shunts without intervening capillaries. | The exact cause of BDBS is not well understood, but it is believed to result from developmental anomalies in the embryonic vasculature. The AVMs are thought to arise from a failure of the normal regression of embryonic vascular connections, leading to direct arterial-to-venous shunts without intervening capillaries. | ||
==Diagnosis== | ==Diagnosis== | ||
Diagnosis of BDBS is primarily clinical, supported by imaging studies. [[Magnetic resonance imaging]] (MRI) and [[computed tomography]] (CT) scans can reveal cerebral AVMs, while [[fluorescein angiography]] is used to visualize retinal AVMs. | Diagnosis of BDBS is primarily clinical, supported by imaging studies. [[Magnetic resonance imaging]] (MRI) and [[computed tomography]] (CT) scans can reveal cerebral AVMs, while [[fluorescein angiography]] is used to visualize retinal AVMs. | ||
[[File:Fluorescein_angiography.jpg|Fluorescein angiography showing retinal AVMs|left|thumb]] | |||
[[File:Fluorescein_angiography.jpg|Fluorescein angiography showing retinal AVMs|thumb | |||
==Management== | ==Management== | ||
There is no cure for BDBS, and management is primarily symptomatic and supportive. Treatment options may include: | There is no cure for BDBS, and management is primarily symptomatic and supportive. Treatment options may include: | ||
* '''Laser photocoagulation''' or '''cryotherapy''' for retinal AVMs to prevent complications such as retinal detachment. | * '''Laser photocoagulation''' or '''cryotherapy''' for retinal AVMs to prevent complications such as retinal detachment. | ||
* '''Surgical intervention''' or '''endovascular therapy''' for cerebral AVMs to reduce the risk of hemorrhage. | * '''Surgical intervention''' or '''endovascular therapy''' for cerebral AVMs to reduce the risk of hemorrhage. | ||
* '''Anticonvulsants''' for seizure management. | * '''Anticonvulsants''' for seizure management. | ||
==Prognosis== | ==Prognosis== | ||
The prognosis of BDBS varies depending on the severity and location of the AVMs. Early detection and management of complications can improve outcomes, but the condition can lead to significant morbidity due to visual and neurological impairments. | The prognosis of BDBS varies depending on the severity and location of the AVMs. Early detection and management of complications can improve outcomes, but the condition can lead to significant morbidity due to visual and neurological impairments. | ||
==See also== | |||
== | |||
* [[Arteriovenous malformation]] | * [[Arteriovenous malformation]] | ||
* [[Phakomatoses]] | * [[Phakomatoses]] | ||
* [[Retinal detachment]] | * [[Retinal detachment]] | ||
* [[Intracerebral hemorrhage]] | * [[Intracerebral hemorrhage]] | ||
[[Category:Congenital disorders]] | [[Category:Congenital disorders]] | ||
[[Category:Rare diseases]] | [[Category:Rare diseases]] | ||
[[Category:Neurocutaneous conditions]] | [[Category:Neurocutaneous conditions]] | ||
Latest revision as of 19:10, 4 April 2025

Editor-In-Chief: Prab R Tumpati, MD
Obesity, Sleep & Internal medicine
Founder, WikiMD Wellnesspedia &
W8MD medical weight loss NYC and sleep center NYC
| Bonnet–Dechaume–Blanc syndrome | |
|---|---|
| |
| Synonyms | Wyburn-Mason syndrome |
| Pronounce | N/A |
| Specialty | Neurology, Ophthalmology |
| Symptoms | Arteriovenous malformations in the retina, midbrain, and facial skin |
| Complications | Intracerebral hemorrhage, seizures, vision loss |
| Onset | Congenital |
| Duration | Lifelong |
| Types | N/A |
| Causes | Genetic mutation |
| Risks | Family history |
| Diagnosis | Clinical examination, MRI, CT scan |
| Differential diagnosis | Sturge-Weber syndrome, Von Hippel-Lindau disease |
| Prevention | N/A |
| Treatment | Surgical intervention, radiotherapy, laser therapy |
| Medication | N/A |
| Prognosis | Variable, depending on severity and complications |
| Frequency | Rare |
| Deaths | N/A |
A rare congenital disorder affecting the eyes and brain
Bonnet–Dechaume–Blanc syndrome (BDBS), also known as Wyburn-Mason syndrome, is a rare congenital disorder characterized by arteriovenous malformations (AVMs) that primarily affect the retina and the brain. This condition is part of the phakomatoses group of disorders, which are neurocutaneous syndromes involving the central nervous system and the skin.
Presentation[edit]
BDBS is typically identified by the presence of AVMs in the retina and the cerebral vasculature. These malformations can lead to a variety of symptoms depending on their size and location.
Ocular Manifestations[edit]

The ocular manifestations of BDBS include retinal AVMs, which can be detected through ophthalmoscopy or fluorescein angiography. These AVMs may cause visual disturbances such as decreased visual acuity, visual field defects, or even retinal detachment.
Neurological Manifestations[edit]

Neurologically, patients may present with symptoms due to cerebral AVMs, such as headaches, seizures, or intracerebral hemorrhage. The location of the AVMs in the brain can lead to specific neurological deficits, including hemiparesis or aphasia.
Visual Field Defects[edit]

Patients with BDBS may experience visual field defects such as homonymous hemianopia, which is a loss of half of the field of view on the same side in both eyes. This occurs due to the involvement of the visual pathways in the brain.
Pathophysiology[edit]
The exact cause of BDBS is not well understood, but it is believed to result from developmental anomalies in the embryonic vasculature. The AVMs are thought to arise from a failure of the normal regression of embryonic vascular connections, leading to direct arterial-to-venous shunts without intervening capillaries.
Diagnosis[edit]
Diagnosis of BDBS is primarily clinical, supported by imaging studies. Magnetic resonance imaging (MRI) and computed tomography (CT) scans can reveal cerebral AVMs, while fluorescein angiography is used to visualize retinal AVMs.

Management[edit]
There is no cure for BDBS, and management is primarily symptomatic and supportive. Treatment options may include:
- Laser photocoagulation or cryotherapy for retinal AVMs to prevent complications such as retinal detachment.
- Surgical intervention or endovascular therapy for cerebral AVMs to reduce the risk of hemorrhage.
- Anticonvulsants for seizure management.
Prognosis[edit]
The prognosis of BDBS varies depending on the severity and location of the AVMs. Early detection and management of complications can improve outcomes, but the condition can lead to significant morbidity due to visual and neurological impairments.