Activated PI3K delta syndrome: Difference between revisions
CSV import |
CSV import |
||
| (One intermediate revision by the same user not shown) | |||
| Line 1: | Line 1: | ||
== Activated PI3K Delta Syndrome == | |||
{{Infobox medical condition | |||
| name = Activated PI3K delta syndrome | |||
| image =[[File:Autosomal_dominant_-_en.svg|200px]] | |||
| caption = [[Autosomal dominant]] pattern | |||
| synonyms = APDS, PASLI disease | |||
| pronounce = | |||
| specialty = [[Immunology]] | |||
| symptoms = [[Recurrent infections]], [[lymphoproliferation]], [[autoimmunity]] | |||
| complications = [[Bronchiectasis]], [[lymphoma]] | |||
| onset = Childhood | |||
| duration = Lifelong | |||
| types = APDS1, APDS2 | |||
| causes = [[Genetic mutation]] in [[PIK3CD]] or [[PIK3R1]] | |||
| risks = Family history | |||
| diagnosis = [[Genetic testing]], [[clinical evaluation]] | |||
| differential = [[Common variable immunodeficiency]], [[X-linked agammaglobulinemia]] | |||
| prevention = None | |||
| treatment = [[Immunoglobulin replacement therapy]], [[mTOR inhibitors]], [[hematopoietic stem cell transplantation]] | |||
| medication = [[Sirolimus]], [[antibiotics]] | |||
| prognosis = Variable, depends on severity and treatment | |||
| frequency = Rare | |||
| deaths = | |||
}} | |||
== Activated PI3K Delta Syndrome == | |||
[[File:Autosomal_dominant_-_en.svg|thumb|right|Diagram of autosomal dominant inheritance]] | [[File:Autosomal_dominant_-_en.svg|thumb|right|Diagram of autosomal dominant inheritance]] | ||
| Line 37: | Line 61: | ||
[[Category:Immunodeficiency disorders]] | [[Category:Immunodeficiency disorders]] | ||
[[Category:Genetic disorders]] | [[Category:Genetic disorders]] | ||
<gallery> | |||
File:Autosomal_dominant_-_en.svg|Autosomal dominant inheritance pattern | |||
File:PI3kinase.png|Structure of PI3 kinase | |||
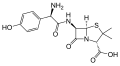
File:Amoxicillin.svg|Chemical structure of Amoxicillin | |||
</gallery> | |||
Latest revision as of 04:21, 4 April 2025
| Activated PI3K delta syndrome | |
|---|---|

| |
| Synonyms | APDS, PASLI disease |
| Pronounce | |
| Specialty | Immunology |
| Symptoms | Recurrent infections, lymphoproliferation, autoimmunity |
| Complications | Bronchiectasis, lymphoma |
| Onset | Childhood |
| Duration | Lifelong |
| Types | APDS1, APDS2 |
| Causes | Genetic mutation in PIK3CD or PIK3R1 |
| Risks | Family history |
| Diagnosis | Genetic testing, clinical evaluation |
| Differential diagnosis | Common variable immunodeficiency, X-linked agammaglobulinemia |
| Prevention | None |
| Treatment | Immunoglobulin replacement therapy, mTOR inhibitors, hematopoietic stem cell transplantation |
| Medication | Sirolimus, antibiotics |
| Prognosis | Variable, depends on severity and treatment |
| Frequency | Rare |
| Deaths | |
== Activated PI3K Delta Syndrome ==


Activated PI3K Delta Syndrome (APDS) is a rare primary immunodeficiency disorder characterized by mutations in the PIK3CD gene, which encodes the p110_ catalytic subunit of phosphoinositide 3-kinase (PI3K). This condition leads to immune dysregulation, recurrent infections, and increased susceptibility to lymphoproliferative disorders.
Pathophysiology[edit]
APDS is caused by gain-of-function mutations in the PIK3CD gene, resulting in hyperactivation of the PI3K delta pathway. This hyperactivation affects the development and function of B cells, T cells, and natural killer cells, leading to immune system dysfunction. The PI3K delta pathway is crucial for the regulation of immune cell signaling, and its dysregulation can result in impaired immune responses and increased risk of autoimmunity.
Clinical Features[edit]
Patients with APDS typically present with recurrent sinopulmonary infections, lymphadenopathy, and hepatosplenomegaly. They may also develop autoimmune disorders and have an increased risk of lymphoma. The condition is often diagnosed in childhood, but symptoms can vary widely among individuals.
Diagnosis[edit]
Diagnosis of APDS involves genetic testing to identify mutations in the PIK3CD gene. Immunological assessments may reveal abnormalities in B and T cell populations, as well as impaired antibody responses. Clinical evaluation of recurrent infections and lymphoproliferative symptoms is also essential for diagnosis.
Treatment[edit]
Management of APDS includes the use of antibiotics to prevent and treat infections, such as amoxicillin. Immunoglobulin replacement therapy may be necessary for patients with significant antibody deficiencies. Targeted therapies, such as PI3K inhibitors, are being investigated as potential treatments to address the underlying immune dysregulation.
Related Pages[edit]
Gallery[edit]
-
Structure of amoxicillin
-
Autosomal dominant inheritance pattern
-
Structure of PI3 kinase
-
Chemical structure of Amoxicillin