Poikiloderma vasculare atrophicans: Difference between revisions
CSV import |
CSV import |
||
| Line 1: | Line 1: | ||
{{SI}} | |||
{{Infobox medical condition | |||
| name = Poikiloderma vasculare atrophicans | |||
| image = [[File:Poikiloderma_vasculare_atrophicans_2.JPG|250px]] | |||
| caption = Poikiloderma vasculare atrophicans on the skin | |||
| synonyms = | |||
| pronounce = | |||
| specialty = [[Dermatology]] | |||
| symptoms = [[Skin atrophy]], [[telangiectasia]], [[hyperpigmentation]], [[hypopigmentation]] | |||
| complications = | |||
| onset = | |||
| duration = | |||
| types = | |||
| causes = | |||
| risks = | |||
| diagnosis = [[Clinical diagnosis]], [[skin biopsy]] | |||
| differential = [[Poikiloderma of Civatte]], [[scleroderma]], [[lupus erythematosus]] | |||
| prevention = | |||
| treatment = | |||
| medication = | |||
| prognosis = | |||
| frequency = | |||
| deaths = | |||
}} | |||
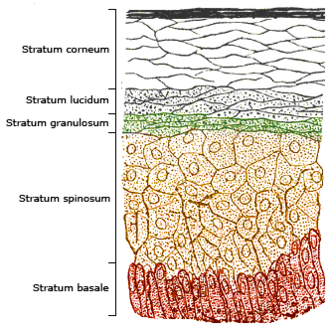
[[File:Skinlayers.png|Diagram of skin layers|left|thumb]] | |||
[[File:Illu_skin02.jpg|Illustration of skin structure|left|thumb]] | |||
'''Poikiloderma vasculare atrophicans''' ('''PVA''') is a rare [[dermatological]] condition characterized by [[skin atrophy]], [[telangiectasia]], and [[hyperpigmentation]]. It is a form of [[poikiloderma]], a group of conditions that involve changes in skin color and texture. | '''Poikiloderma vasculare atrophicans''' ('''PVA''') is a rare [[dermatological]] condition characterized by [[skin atrophy]], [[telangiectasia]], and [[hyperpigmentation]]. It is a form of [[poikiloderma]], a group of conditions that involve changes in skin color and texture. | ||
==Etiology== | ==Etiology== | ||
The exact cause of PVA is unknown. However, it is believed to be associated with various underlying conditions such as [[cutaneous T-cell lymphoma]], [[dermatomyositis]], and [[scleroderma]]. Some researchers suggest that it may be an autoimmune response, but this theory is not universally accepted. | The exact cause of PVA is unknown. However, it is believed to be associated with various underlying conditions such as [[cutaneous T-cell lymphoma]], [[dermatomyositis]], and [[scleroderma]]. Some researchers suggest that it may be an autoimmune response, but this theory is not universally accepted. | ||
==Symptoms== | ==Symptoms== | ||
The primary symptoms of PVA include changes in skin color (hyperpigmentation and hypopigmentation), skin atrophy, and telangiectasia. These changes typically occur on the neck, chest, and limbs. The skin may also become dry and scaly. In some cases, patients may experience itching or discomfort. | The primary symptoms of PVA include changes in skin color (hyperpigmentation and hypopigmentation), skin atrophy, and telangiectasia. These changes typically occur on the neck, chest, and limbs. The skin may also become dry and scaly. In some cases, patients may experience itching or discomfort. | ||
==Diagnosis== | ==Diagnosis== | ||
Diagnosis of PVA is primarily based on clinical examination and the patient's medical history. [[Dermoscopy]] and [[skin biopsy]] may be used to confirm the diagnosis and rule out other conditions. | Diagnosis of PVA is primarily based on clinical examination and the patient's medical history. [[Dermoscopy]] and [[skin biopsy]] may be used to confirm the diagnosis and rule out other conditions. | ||
==Treatment== | ==Treatment== | ||
There is currently no cure for PVA. Treatment is primarily aimed at managing symptoms and preventing complications. This may include the use of [[topical corticosteroids]], [[photoprotection]], and [[emollients]]. In severe cases, [[immunomodulatory therapy]] may be considered. | There is currently no cure for PVA. Treatment is primarily aimed at managing symptoms and preventing complications. This may include the use of [[topical corticosteroids]], [[photoprotection]], and [[emollients]]. In severe cases, [[immunomodulatory therapy]] may be considered. | ||
==Prognosis== | ==Prognosis== | ||
The prognosis for PVA varies depending on the underlying cause and the severity of the condition. With appropriate management, most patients can lead a normal life. However, the condition can cause significant cosmetic concerns and may impact the patient's quality of life. | The prognosis for PVA varies depending on the underlying cause and the severity of the condition. With appropriate management, most patients can lead a normal life. However, the condition can cause significant cosmetic concerns and may impact the patient's quality of life. | ||
==See also== | ==See also== | ||
* [[Cutaneous T-cell lymphoma]] | * [[Cutaneous T-cell lymphoma]] | ||
| Line 26: | Line 41: | ||
* [[Scleroderma]] | * [[Scleroderma]] | ||
* [[Poikiloderma]] | * [[Poikiloderma]] | ||
[[Category:Dermatology]] | [[Category:Dermatology]] | ||
[[Category:Rare diseases]] | [[Category:Rare diseases]] | ||
| Line 32: | Line 46: | ||
{{dermatology-stub}} | {{dermatology-stub}} | ||
{{rare-diseases-stub}} | {{rare-diseases-stub}} | ||
Latest revision as of 22:00, 9 April 2025

Editor-In-Chief: Prab R Tumpati, MD
Obesity, Sleep & Internal medicine
Founder, WikiMD Wellnesspedia &
W8MD medical weight loss NYC and sleep center NYC
| Poikiloderma vasculare atrophicans | |
|---|---|

| |
| Synonyms | |
| Pronounce | |
| Specialty | Dermatology |
| Symptoms | Skin atrophy, telangiectasia, hyperpigmentation, hypopigmentation |
| Complications | |
| Onset | |
| Duration | |
| Types | |
| Causes | |
| Risks | |
| Diagnosis | Clinical diagnosis, skin biopsy |
| Differential diagnosis | Poikiloderma of Civatte, scleroderma, lupus erythematosus |
| Prevention | |
| Treatment | |
| Medication | |
| Prognosis | |
| Frequency | |
| Deaths | |

Poikiloderma vasculare atrophicans (PVA) is a rare dermatological condition characterized by skin atrophy, telangiectasia, and hyperpigmentation. It is a form of poikiloderma, a group of conditions that involve changes in skin color and texture.
Etiology[edit]
The exact cause of PVA is unknown. However, it is believed to be associated with various underlying conditions such as cutaneous T-cell lymphoma, dermatomyositis, and scleroderma. Some researchers suggest that it may be an autoimmune response, but this theory is not universally accepted.
Symptoms[edit]
The primary symptoms of PVA include changes in skin color (hyperpigmentation and hypopigmentation), skin atrophy, and telangiectasia. These changes typically occur on the neck, chest, and limbs. The skin may also become dry and scaly. In some cases, patients may experience itching or discomfort.
Diagnosis[edit]
Diagnosis of PVA is primarily based on clinical examination and the patient's medical history. Dermoscopy and skin biopsy may be used to confirm the diagnosis and rule out other conditions.
Treatment[edit]
There is currently no cure for PVA. Treatment is primarily aimed at managing symptoms and preventing complications. This may include the use of topical corticosteroids, photoprotection, and emollients. In severe cases, immunomodulatory therapy may be considered.
Prognosis[edit]
The prognosis for PVA varies depending on the underlying cause and the severity of the condition. With appropriate management, most patients can lead a normal life. However, the condition can cause significant cosmetic concerns and may impact the patient's quality of life.
See also[edit]

This article is a dermatology stub. You can help WikiMD by expanding it!
This rare disease-related article is a stub. You can help WikiMD by expanding it.