Muir–Torre syndrome: Difference between revisions
CSV import |
No edit summary |
||
| Line 3: | Line 3: | ||
| synonyms = MTS | | synonyms = MTS | ||
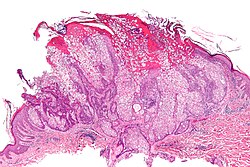
| image = Sebaceous adenoma - low mag.jpg | | image = Sebaceous adenoma - low mag.jpg | ||
| caption = [[Micrograph]] of a [[sebaceous adenoma]], | | caption = [[Micrograph]] of a [[sebaceous adenoma]], commonly associated with Muir–Torre syndrome. [[H&E stain]]. | ||
| pronounce = | | pronounce = | ||
| field = | | field = [[Oncology]], [[Dermatology]], [[Genetics]] | ||
| symptoms = | | symptoms = Sebaceous tumors, internal malignancies | ||
| complications = | | complications = Colorectal cancer, genitourinary cancers | ||
| onset = | | onset = Usually adulthood | ||
| duration = | | duration = Lifelong | ||
| types = | | types = | ||
| causes = | | causes = Genetic mutations in [[MLH1]], [[MSH2]], [[MSH6]] genes | ||
| risks = | | risks = Family history of Lynch syndrome | ||
| diagnosis = | | diagnosis = Clinical presentation, genetic testing, immunohistochemistry | ||
| differential = | | differential = Sporadic sebaceous tumors, other hereditary cancer syndromes | ||
| prevention = | | prevention = Regular screening, genetic counseling | ||
| treatment = | | treatment = Surgical excision, regular cancer surveillance | ||
| medication = | | medication = | ||
| prognosis = | | prognosis = Good with early detection and management | ||
| frequency = | | frequency = Rare | ||
| deaths = | | deaths = Usually related to complications from malignancies | ||
}} | }} | ||
'''Muir–Torre syndrome''' is a rare hereditary | '''Muir–Torre syndrome''' ('''MTS''') is a rare, hereditary [[autosomal dominant]] [[cancer syndrome]], considered a subtype of [[Lynch syndrome]] (Hereditary Non-Polyposis Colorectal Cancer, [[HNPCC]]). Individuals with this syndrome have an increased susceptibility to cancers of the colon, genitourinary tract, and distinct skin lesions, including [[keratoacanthoma]]s and sebaceous tumors such as [[sebaceous adenoma]], sebaceous epithelioma, and [[sebaceous carcinoma]]. | ||
== Symptoms == | == Signs and Symptoms == | ||
Characteristic features include: | |||
* Presence of at least one sebaceous gland tumor (adenoma, epithelioma, or carcinoma) | |||
* Occurrence of at least one internal malignancy, commonly colorectal or genitourinary cancers | |||
== Genetics == | |||
Muir–Torre syndrome is caused primarily by mutations in the [[MLH1]], [[MSH2]], and more recently identified [[MSH6]] genes. These genes are critical for the [[DNA mismatch repair]] pathway. Mutations result in defective DNA repair mechanisms, increasing the risk of developing cancers. | |||
== Diagnosis == | |||
Diagnosis typically involves: | |||
* Clinical evaluation of sebaceous skin tumors and internal malignancies | |||
* Genetic testing for mutations in DNA mismatch repair genes | |||
* Immunohistochemical analysis for mismatch repair proteins | |||
* Application of the [[Amsterdam criteria]], widely used to diagnose Lynch syndrome and Muir–Torre syndrome, which include: | |||
** At least three relatives affected by Lynch-associated cancers (colorectal, endometrial, small bowel, ureter, renal pelvis) | |||
** Cancer affecting at least two successive generations | |||
** At least one individual diagnosed before age 50 | |||
** Exclusion of familial adenomatous polyposis | |||
The Mayo Muir–Torre risk score was developed to enhance diagnostic accuracy, distinguishing true cases from sporadic sebaceous tumors. | |||
== Management == | |||
Treatment strategies involve: | |||
* Surgical removal of skin lesions | |||
* Regular screening and surveillance for internal malignancies (colonoscopies, genitourinary screenings) | |||
* Genetic counseling for patients and their families | |||
== Prognosis == | |||
With appropriate management and regular surveillance, the prognosis for individuals with Muir–Torre syndrome can be favorable. Early detection and treatment of malignancies significantly improve outcomes. | |||
== Prevention == | |||
Preventive measures focus on: | |||
* Early genetic screening and counseling for at-risk families | |||
* Frequent surveillance for early detection of malignancies | |||
Muir–Torre syndrome remains a rare condition, requiring multidisciplinary care involving dermatologists, geneticists, oncologists, and surgeons. | |||
== Eponym == | == Eponym == | ||
It is named for EG Muir and D Torre. A British physician, Muir noted a patient with many keratoacanthomas who went on to develop several internal malignancies at a young age. Torre presented his findings at a meeting of the New York Dermatologic Society. | It is named for EG Muir and D Torre. A British physician, Muir noted a patient with many keratoacanthomas who went on to develop several internal malignancies at a young age. Torre presented his findings at a meeting of the New York Dermatologic Society. | ||
== See also == | == See also == | ||
* [[List of cutaneous conditions]] | * [[List of cutaneous conditions]] | ||
* [[List of cutaneous conditions associated with increased risk of nonmelanoma skin cancer]] | * [[List of cutaneous conditions associated with increased risk of nonmelanoma skin cancer]] | ||
== External links == | == External links == | ||
| Line 105: | Line 82: | ||
| Orphanet = 587 | | Orphanet = 587 | ||
}} | }} | ||
{{Tumors of skin appendages}} | {{Tumors of skin appendages}} | ||
{{DNA repair-deficiency disorder}} | {{DNA repair-deficiency disorder}} | ||
{{stub}} | |||
{{DEFAULTSORT:Muir-Torre syndrome}} | {{DEFAULTSORT:Muir-Torre syndrome}} | ||
[[Category:Epidermal nevi, neoplasms, and cysts]] | [[Category:Epidermal nevi, neoplasms, and cysts]] | ||
[[Category:DNA replication and repair-deficiency disorders]] | [[Category:DNA replication and repair-deficiency disorders]] | ||
[[Category:Syndromes]] | [[Category:Syndromes]] | ||
Latest revision as of 14:18, 27 March 2025
| Muir–Torre syndrome | |
|---|---|
| |
| Synonyms | MTS |
| Pronounce | |
| Field | Oncology, Dermatology, Genetics |
| Symptoms | Sebaceous tumors, internal malignancies |
| Complications | Colorectal cancer, genitourinary cancers |
| Onset | Usually adulthood |
| Duration | Lifelong |
| Types | |
| Causes | Genetic mutations in MLH1, MSH2, MSH6 genes |
| Risks | Family history of Lynch syndrome |
| Diagnosis | Clinical presentation, genetic testing, immunohistochemistry |
| Differential diagnosis | Sporadic sebaceous tumors, other hereditary cancer syndromes |
| Prevention | Regular screening, genetic counseling |
| Treatment | Surgical excision, regular cancer surveillance |
| Medication | |
| Prognosis | Good with early detection and management |
| Frequency | Rare |
| Deaths | Usually related to complications from malignancies |
Muir–Torre syndrome (MTS) is a rare, hereditary autosomal dominant cancer syndrome, considered a subtype of Lynch syndrome (Hereditary Non-Polyposis Colorectal Cancer, HNPCC). Individuals with this syndrome have an increased susceptibility to cancers of the colon, genitourinary tract, and distinct skin lesions, including keratoacanthomas and sebaceous tumors such as sebaceous adenoma, sebaceous epithelioma, and sebaceous carcinoma.
Signs and Symptoms[edit]
Characteristic features include:
- Presence of at least one sebaceous gland tumor (adenoma, epithelioma, or carcinoma)
- Occurrence of at least one internal malignancy, commonly colorectal or genitourinary cancers
Genetics[edit]
Muir–Torre syndrome is caused primarily by mutations in the MLH1, MSH2, and more recently identified MSH6 genes. These genes are critical for the DNA mismatch repair pathway. Mutations result in defective DNA repair mechanisms, increasing the risk of developing cancers.
Diagnosis[edit]
Diagnosis typically involves:
- Clinical evaluation of sebaceous skin tumors and internal malignancies
- Genetic testing for mutations in DNA mismatch repair genes
- Immunohistochemical analysis for mismatch repair proteins
- Application of the Amsterdam criteria, widely used to diagnose Lynch syndrome and Muir–Torre syndrome, which include:
- At least three relatives affected by Lynch-associated cancers (colorectal, endometrial, small bowel, ureter, renal pelvis)
- Cancer affecting at least two successive generations
- At least one individual diagnosed before age 50
- Exclusion of familial adenomatous polyposis
The Mayo Muir–Torre risk score was developed to enhance diagnostic accuracy, distinguishing true cases from sporadic sebaceous tumors.
Management[edit]
Treatment strategies involve:
- Surgical removal of skin lesions
- Regular screening and surveillance for internal malignancies (colonoscopies, genitourinary screenings)
- Genetic counseling for patients and their families
Prognosis[edit]
With appropriate management and regular surveillance, the prognosis for individuals with Muir–Torre syndrome can be favorable. Early detection and treatment of malignancies significantly improve outcomes.
Prevention[edit]
Preventive measures focus on:
- Early genetic screening and counseling for at-risk families
- Frequent surveillance for early detection of malignancies
Muir–Torre syndrome remains a rare condition, requiring multidisciplinary care involving dermatologists, geneticists, oncologists, and surgeons.
Eponym[edit]
It is named for EG Muir and D Torre. A British physician, Muir noted a patient with many keratoacanthomas who went on to develop several internal malignancies at a young age. Torre presented his findings at a meeting of the New York Dermatologic Society.
See also[edit]
- List of cutaneous conditions
- List of cutaneous conditions associated with increased risk of nonmelanoma skin cancer
External links[edit]
| Tumors and associated structures | ||||||
|---|---|---|---|---|---|---|
|
| Metabolic disease: DNA replication and DNA repair-deficiency disorder | ||||
|---|---|---|---|---|
|


