Pseudohypoaldosteronism: Difference between revisions
CSV import Tags: mobile edit mobile web edit |
CSV import |
||
| Line 1: | Line 1: | ||
{{SI}} | |||
{{Infobox medical condition | |||
| name = Pseudohypoaldosteronism | |||
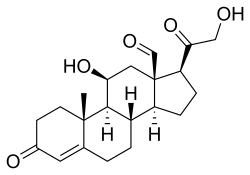
| image = [[File:Aldosterone-2D-skeletal.svg|150px]] | |||
| caption = Skeletal formula of [[aldosterone]] | |||
| field = [[Endocrinology]] | |||
| symptoms = [[Hyponatremia]], [[hyperkalemia]], [[metabolic acidosis]], [[hypotension]] | |||
| complications = [[Dehydration]], [[failure to thrive]] | |||
| onset = [[Neonatal]] | |||
| duration = [[Chronic]] | |||
| types = Type 1 (systemic and renal), Type 2 | |||
| causes = [[Genetic mutation]]s in [[mineralocorticoid receptor]] or [[sodium channel]]s | |||
| risks = Family history of the condition | |||
| diagnosis = [[Blood test]]s, [[urine test]]s, [[genetic testing]] | |||
| differential = [[Congenital adrenal hyperplasia]], [[Addison's disease]], [[Bartter syndrome]] | |||
| treatment = [[Sodium supplementation]], [[potassium restriction]], [[fludrocortisone]] | |||
| medication = [[Fludrocortisone]] | |||
| prognosis = Generally good with treatment | |||
| frequency = Rare | |||
}} | |||
'''Pseudohypoaldosteronism''' (PHA) is a medical condition that involves the [[kidney]]s and the [[aldosterone]] hormone. It is characterized by an apparent state of [[aldosterone]] deficiency, despite having normal or elevated levels of the hormone in the body. There are two types of PHA: Type 1 and Type 2. | '''Pseudohypoaldosteronism''' (PHA) is a medical condition that involves the [[kidney]]s and the [[aldosterone]] hormone. It is characterized by an apparent state of [[aldosterone]] deficiency, despite having normal or elevated levels of the hormone in the body. There are two types of PHA: Type 1 and Type 2. | ||
==Type 1 Pseudohypoaldosteronism== | ==Type 1 Pseudohypoaldosteronism== | ||
Type 1 PHA is further divided into two subtypes: autosomal dominant and autosomal recessive. The autosomal dominant form is also known as PHA1A or renal PHA1, and the autosomal recessive form is known as PHA1B or systemic PHA1. | Type 1 PHA is further divided into two subtypes: autosomal dominant and autosomal recessive. The autosomal dominant form is also known as PHA1A or renal PHA1, and the autosomal recessive form is known as PHA1B or systemic PHA1. | ||
===PHA1A=== | ===PHA1A=== | ||
PHA1A is caused by mutations in the [[mineralocorticoid receptor]] gene (NR3C2). It is characterized by [[salt-wasting]], [[hyperkalemia]], and [[metabolic acidosis]]. Symptoms usually appear in the neonatal period and improve with age. | PHA1A is caused by mutations in the [[mineralocorticoid receptor]] gene (NR3C2). It is characterized by [[salt-wasting]], [[hyperkalemia]], and [[metabolic acidosis]]. Symptoms usually appear in the neonatal period and improve with age. | ||
===PHA1B=== | ===PHA1B=== | ||
PHA1B is caused by mutations in the genes encoding the epithelial sodium channel (ENaC). It is characterized by severe salt-wasting, failure to thrive, and recurrent [[pneumonia]]. Unlike PHA1A, symptoms do not improve with age. | PHA1B is caused by mutations in the genes encoding the epithelial sodium channel (ENaC). It is characterized by severe salt-wasting, failure to thrive, and recurrent [[pneumonia]]. Unlike PHA1A, symptoms do not improve with age. | ||
==Type 2 Pseudohypoaldosteronism== | ==Type 2 Pseudohypoaldosteronism== | ||
Type 2 PHA, also known as Gordon's syndrome, is caused by mutations in the WNK1, WNK4, CUL3, or KLHL3 genes. It is characterized by [[hypertension]], [[hyperkalemia]], and [[metabolic acidosis]]. | Type 2 PHA, also known as Gordon's syndrome, is caused by mutations in the WNK1, WNK4, CUL3, or KLHL3 genes. It is characterized by [[hypertension]], [[hyperkalemia]], and [[metabolic acidosis]]. | ||
==Diagnosis== | ==Diagnosis== | ||
Diagnosis of PHA is based on clinical symptoms, laboratory findings, and genetic testing. Laboratory findings typically show low levels of sodium and high levels of potassium in the blood. Genetic testing can confirm the diagnosis and identify the specific type of PHA. | Diagnosis of PHA is based on clinical symptoms, laboratory findings, and genetic testing. Laboratory findings typically show low levels of sodium and high levels of potassium in the blood. Genetic testing can confirm the diagnosis and identify the specific type of PHA. | ||
==Treatment== | ==Treatment== | ||
Treatment of PHA involves managing the symptoms and preventing complications. This may include a low-potassium diet, medications to lower potassium levels, and in some cases, hormone replacement therapy. | Treatment of PHA involves managing the symptoms and preventing complications. This may include a low-potassium diet, medications to lower potassium levels, and in some cases, hormone replacement therapy. | ||
==See also== | ==See also== | ||
* [[Aldosterone]] | * [[Aldosterone]] | ||
| Line 24: | Line 37: | ||
* [[Hyperkalemia]] | * [[Hyperkalemia]] | ||
* [[Metabolic acidosis]] | * [[Metabolic acidosis]] | ||
[[Category:Endocrine diseases]] | [[Category:Endocrine diseases]] | ||
[[Category:Genetic disorders]] | [[Category:Genetic disorders]] | ||
[[Category:Rare diseases]] | [[Category:Rare diseases]] | ||
{{stub}} | {{stub}} | ||
Latest revision as of 22:12, 6 April 2025

Editor-In-Chief: Prab R Tumpati, MD
Obesity, Sleep & Internal medicine
Founder, WikiMD Wellnesspedia &
W8MD medical weight loss NYC and sleep center NYC
| Pseudohypoaldosteronism | |
|---|---|
| |
| Synonyms | N/A |
| Pronounce | N/A |
| Specialty | N/A |
| Symptoms | Hyponatremia, hyperkalemia, metabolic acidosis, hypotension |
| Complications | Dehydration, failure to thrive |
| Onset | Neonatal |
| Duration | Chronic |
| Types | Type 1 (systemic and renal), Type 2 |
| Causes | Genetic mutations in mineralocorticoid receptor or sodium channels |
| Risks | Family history of the condition |
| Diagnosis | Blood tests, urine tests, genetic testing |
| Differential diagnosis | Congenital adrenal hyperplasia, Addison's disease, Bartter syndrome |
| Prevention | N/A |
| Treatment | Sodium supplementation, potassium restriction, fludrocortisone |
| Medication | Fludrocortisone |
| Prognosis | Generally good with treatment |
| Frequency | Rare |
| Deaths | N/A |
Pseudohypoaldosteronism (PHA) is a medical condition that involves the kidneys and the aldosterone hormone. It is characterized by an apparent state of aldosterone deficiency, despite having normal or elevated levels of the hormone in the body. There are two types of PHA: Type 1 and Type 2.
Type 1 Pseudohypoaldosteronism[edit]
Type 1 PHA is further divided into two subtypes: autosomal dominant and autosomal recessive. The autosomal dominant form is also known as PHA1A or renal PHA1, and the autosomal recessive form is known as PHA1B or systemic PHA1.
PHA1A[edit]
PHA1A is caused by mutations in the mineralocorticoid receptor gene (NR3C2). It is characterized by salt-wasting, hyperkalemia, and metabolic acidosis. Symptoms usually appear in the neonatal period and improve with age.
PHA1B[edit]
PHA1B is caused by mutations in the genes encoding the epithelial sodium channel (ENaC). It is characterized by severe salt-wasting, failure to thrive, and recurrent pneumonia. Unlike PHA1A, symptoms do not improve with age.
Type 2 Pseudohypoaldosteronism[edit]
Type 2 PHA, also known as Gordon's syndrome, is caused by mutations in the WNK1, WNK4, CUL3, or KLHL3 genes. It is characterized by hypertension, hyperkalemia, and metabolic acidosis.
Diagnosis[edit]
Diagnosis of PHA is based on clinical symptoms, laboratory findings, and genetic testing. Laboratory findings typically show low levels of sodium and high levels of potassium in the blood. Genetic testing can confirm the diagnosis and identify the specific type of PHA.
Treatment[edit]
Treatment of PHA involves managing the symptoms and preventing complications. This may include a low-potassium diet, medications to lower potassium levels, and in some cases, hormone replacement therapy.


