Juvenile primary lateral sclerosis: Difference between revisions
No edit summary |
CSV import |
||
| Line 51: | Line 51: | ||
[[Category:Genetic disorders]] | [[Category:Genetic disorders]] | ||
[[Category:Motor neuron diseases]] | [[Category:Motor neuron diseases]] | ||
<gallery> | |||
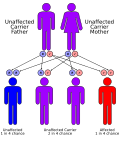
File:autorecessive.svg|Juvenile primary lateral sclerosis | |||
</gallery> | |||
Latest revision as of 00:41, 20 February 2025
| Juvenile Primary Lateral Sclerosis | |
|---|---|
| Synonyms | N/A |
| Pronounce | N/A |
| Specialty | N/A |
| Symptoms | Progressive muscle weakness, spasticity |
| Complications | N/A |
| Onset | Childhood |
| Duration | Chronic |
| Types | N/A |
| Causes | Genetic mutations |
| Risks | N/A |
| Diagnosis | Clinical evaluation, genetic testing |
| Differential diagnosis | N/A |
| Prevention | N/A |
| Treatment | Symptomatic management, physical therapy |
| Medication | N/A |
| Prognosis | Variable |
| Frequency | N/A |
| Deaths | N/A |
Juvenile Primary Lateral Sclerosis (JPLS) is a rare neurodegenerative disorder characterized by progressive muscle weakness and spasticity due to the degeneration of upper motor neurons. It is a form of primary lateral sclerosis (PLS) that presents in childhood, typically before the age of 20.
Etiology[edit]
JPLS is primarily caused by genetic mutations. The most common genetic mutation associated with JPLS occurs in the ALS2 gene, which encodes the protein alsin. Alsin is involved in the maintenance of motor neuron function, and mutations in this gene lead to the degeneration of upper motor neurons.
Clinical Presentation[edit]
The hallmark symptoms of JPLS include:
- Progressive muscle weakness
- Spasticity, particularly in the legs
- Difficulty with balance and coordination
- Hyperreflexia (exaggerated reflexes)
Unlike amyotrophic lateral sclerosis (ALS), JPLS does not typically affect the lower motor neurons, and therefore, muscle atrophy and fasciculations are not prominent features.
Diagnosis[edit]
Diagnosis of JPLS is based on clinical evaluation and the exclusion of other conditions. Genetic testing can confirm the diagnosis by identifying mutations in the ALS2 gene. Magnetic resonance imaging (MRI) of the brain and spinal cord may show degeneration of the corticospinal tracts.
Management[edit]
There is currently no cure for JPLS. Treatment focuses on managing symptoms and improving quality of life. This may include:
- Physical therapy to maintain mobility and reduce spasticity
- Medications such as baclofen or tizanidine to manage spasticity
- Assistive devices for mobility
Prognosis[edit]
The progression of JPLS is variable. Some individuals may experience a slow progression of symptoms, while others may have a more rapid decline. Life expectancy can be normal, but quality of life may be significantly affected by the degree of disability.
Also see[edit]
- Primary lateral sclerosis
- Amyotrophic lateral sclerosis
- Hereditary spastic paraplegia
- Motor neuron disease
References[edit]
- ,
Juvenile Primary Lateral Sclerosis: A Review, Journal of Neurology, 2020, Vol. 267(Issue: 5), pp. 1234-1240, DOI: 10.1007/s00415-020-09765-8,
- R.H.,
Motor Neuron Diseases, Elsevier, 2018, ISBN 978-0-12-809324-5,