Corneal neovascularization: Difference between revisions
CSV import |
CSV import |
||
| Line 1: | Line 1: | ||
{{SI}} | |||
{{Infobox medical condition | |||
| name = Corneal neovascularization | |||
| image = [[File:Corneaneo.jpg|left|thumb|Corneal neovascularization]] | |||
| caption = Corneal neovascularization visible in the eye | |||
| field = [[Ophthalmology]] | |||
| symptoms = [[Red eye]], [[decreased vision]], [[photophobia]] | |||
| complications = [[Corneal scarring]], [[vision loss]] | |||
| onset = Gradual | |||
| duration = Chronic | |||
| causes = [[Contact lens overwear]], [[corneal infection]], [[trauma]], [[hypoxia]] | |||
| risks = [[Contact lens use]], [[eye surgery]], [[chemical injury]] | |||
| diagnosis = [[Slit lamp examination]], [[fluorescein angiography]] | |||
| differential = [[Conjunctivitis]], [[keratitis]], [[pterygium]] | |||
| prevention = Proper [[contact lens hygiene]], avoiding [[eye trauma]] | |||
| treatment = [[Topical corticosteroids]], [[anti-VEGF therapy]], [[surgical intervention]] | |||
| prognosis = Variable, depending on severity and treatment | |||
| frequency = Common in contact lens users | |||
}} | |||
'''Corneal Neovascularization''' is a pathological condition characterized by the growth of new blood vessels into the [[cornea]], which is normally avascular. This condition can significantly compromise visual acuity and ocular health, leading to a range of visual impairments. The cornea's transparency is crucial for the refraction of light onto the [[retina]], and the invasion of blood vessels disrupts this clarity, potentially resulting in visual disturbances or blindness. | '''Corneal Neovascularization''' is a pathological condition characterized by the growth of new blood vessels into the [[cornea]], which is normally avascular. This condition can significantly compromise visual acuity and ocular health, leading to a range of visual impairments. The cornea's transparency is crucial for the refraction of light onto the [[retina]], and the invasion of blood vessels disrupts this clarity, potentially resulting in visual disturbances or blindness. | ||
==Causes== | ==Causes== | ||
Corneal neovascularization can be triggered by a variety of factors, including but not limited to: | Corneal neovascularization can be triggered by a variety of factors, including but not limited to: | ||
| Line 10: | Line 28: | ||
* [[Dry eye syndrome]] | * [[Dry eye syndrome]] | ||
* [[Corneal graft rejection]] | * [[Corneal graft rejection]] | ||
==Symptoms== | ==Symptoms== | ||
Symptoms of corneal neovascularization may include: | Symptoms of corneal neovascularization may include: | ||
| Line 18: | Line 35: | ||
* Pain or discomfort in the eye | * Pain or discomfort in the eye | ||
* The feeling of a foreign body in the eye | * The feeling of a foreign body in the eye | ||
==Diagnosis== | ==Diagnosis== | ||
Diagnosis of corneal neovascularization involves a comprehensive eye examination, including: | Diagnosis of corneal neovascularization involves a comprehensive eye examination, including: | ||
| Line 25: | Line 41: | ||
* [[Corneal topography]] or [[OCT (Optical Coherence Tomography)]] scans to assess the cornea's shape and thickness | * [[Corneal topography]] or [[OCT (Optical Coherence Tomography)]] scans to assess the cornea's shape and thickness | ||
* Fluorescein angiography to highlight the blood vessels | * Fluorescein angiography to highlight the blood vessels | ||
==Treatment== | ==Treatment== | ||
Treatment aims to reduce the risk factors, control the underlying cause, and inhibit the growth of new blood vessels. Options include: | Treatment aims to reduce the risk factors, control the underlying cause, and inhibit the growth of new blood vessels. Options include: | ||
| Line 33: | Line 48: | ||
* [[Photodynamic therapy]] with verteporfin | * [[Photodynamic therapy]] with verteporfin | ||
* Surgical options, such as fine needle diathermy or corneal transplantation in severe cases | * Surgical options, such as fine needle diathermy or corneal transplantation in severe cases | ||
==Prevention== | ==Prevention== | ||
Preventive measures focus on minimizing the risk factors associated with corneal neovascularization: | Preventive measures focus on minimizing the risk factors associated with corneal neovascularization: | ||
| Line 40: | Line 54: | ||
* Protecting eyes from chemical exposures and UV light | * Protecting eyes from chemical exposures and UV light | ||
* Managing dry eye syndrome and other ocular surface diseases | * Managing dry eye syndrome and other ocular surface diseases | ||
==Prognosis== | ==Prognosis== | ||
The prognosis for individuals with corneal neovascularization varies depending on the cause, extent, and response to treatment. Early detection and treatment are crucial for preserving vision and preventing permanent damage to the cornea. | The prognosis for individuals with corneal neovascularization varies depending on the cause, extent, and response to treatment. Early detection and treatment are crucial for preserving vision and preventing permanent damage to the cornea. | ||
==Gallery== | |||
<gallery> | <gallery> | ||
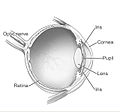
File:Human_eye_diagram-sagittal_view-NEI.jpg|Sagittal view of the human eye | File:Human_eye_diagram-sagittal_view-NEI.jpg|Sagittal view of the human eye | ||
File:Normal_Cornea_(Fig_1).tif|Normal cornea | File:Normal_Cornea_(Fig_1).tif|Normal cornea | ||
</gallery> | </gallery> | ||
[[Category:Eye diseases]] | |||
[[Category:Corneal disorders]] | |||
{{medicine-stub}} | |||
Latest revision as of 13:36, 5 April 2025

Editor-In-Chief: Prab R Tumpati, MD
Obesity, Sleep & Internal medicine
Founder, WikiMD Wellnesspedia &
W8MD medical weight loss NYC and sleep center NYC
| Corneal neovascularization | |
|---|---|
 | |
| Synonyms | N/A |
| Pronounce | N/A |
| Specialty | N/A |
| Symptoms | Red eye, decreased vision, photophobia |
| Complications | Corneal scarring, vision loss |
| Onset | Gradual |
| Duration | Chronic |
| Types | N/A |
| Causes | Contact lens overwear, corneal infection, trauma, hypoxia |
| Risks | Contact lens use, eye surgery, chemical injury |
| Diagnosis | Slit lamp examination, fluorescein angiography |
| Differential diagnosis | Conjunctivitis, keratitis, pterygium |
| Prevention | Proper contact lens hygiene, avoiding eye trauma |
| Treatment | Topical corticosteroids, anti-VEGF therapy, surgical intervention |
| Medication | N/A |
| Prognosis | Variable, depending on severity and treatment |
| Frequency | Common in contact lens users |
| Deaths | N/A |
Corneal Neovascularization is a pathological condition characterized by the growth of new blood vessels into the cornea, which is normally avascular. This condition can significantly compromise visual acuity and ocular health, leading to a range of visual impairments. The cornea's transparency is crucial for the refraction of light onto the retina, and the invasion of blood vessels disrupts this clarity, potentially resulting in visual disturbances or blindness.
Causes[edit]
Corneal neovascularization can be triggered by a variety of factors, including but not limited to:
- Ocular surface disease and inflammation
- Contact lens overwear or misuse
- Chemical burns to the eye
- Infectious keratitis, involving bacterial, viral, fungal, or parasitic infections
- Corneal hypoxia, or reduced oxygen supply to the cornea
- Dry eye syndrome
- Corneal graft rejection
Symptoms[edit]
Symptoms of corneal neovascularization may include:
- Redness of the eye
- Sensitivity to light (Photophobia)
- Blurred vision
- Pain or discomfort in the eye
- The feeling of a foreign body in the eye
Diagnosis[edit]
Diagnosis of corneal neovascularization involves a comprehensive eye examination, including:
- Visual acuity test
- Slit lamp examination to observe the extent and pattern of neovascularization
- Corneal topography or OCT (Optical Coherence Tomography) scans to assess the cornea's shape and thickness
- Fluorescein angiography to highlight the blood vessels
Treatment[edit]
Treatment aims to reduce the risk factors, control the underlying cause, and inhibit the growth of new blood vessels. Options include:
- Anti-VEGF therapy (Vascular Endothelial Growth Factor inhibitors), such as bevacizumab or ranibizumab, to directly target the growth of new blood vessels
- Corticosteroids to reduce inflammation
- Laser photocoagulation to cauterize and close off the vessels
- Photodynamic therapy with verteporfin
- Surgical options, such as fine needle diathermy or corneal transplantation in severe cases
Prevention[edit]
Preventive measures focus on minimizing the risk factors associated with corneal neovascularization:
- Proper use and care of contact lenses
- Timely treatment of corneal infections and injuries
- Protecting eyes from chemical exposures and UV light
- Managing dry eye syndrome and other ocular surface diseases
Prognosis[edit]
The prognosis for individuals with corneal neovascularization varies depending on the cause, extent, and response to treatment. Early detection and treatment are crucial for preserving vision and preventing permanent damage to the cornea.
Gallery[edit]
-
Sagittal view of the human eye
-
Normal cornea