Creatine transporter defect: Difference between revisions
CSV import |
CSV import Tags: mobile edit mobile web edit |
||
| Line 1: | Line 1: | ||
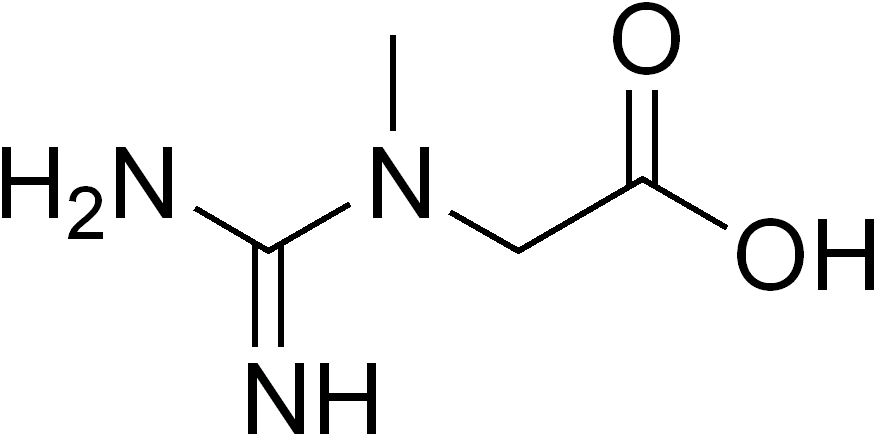
[[File:Creatine_neutral.png|Creatine neutral|thumb]] '''Creatine Transporter Defect''' (CTD) is a rare [[genetic disorder]] that affects the body's ability to transport [[creatine]], a key molecule in energy storage and supply, into cells. This condition primarily impacts the [[brain]], where creatine plays a crucial role in energy metabolism, leading to various neurological and developmental issues. CTD is classified under the broader category of [[creatine deficiency syndromes]], which also includes [[arginine:glycine amidinotransferase deficiency]] and [[guanidinoacetate methyltransferase deficiency]]. | {{SI}} | ||
{{Infobox medical condition | |||
| name = Creatine transporter defect | |||
| image = [[File:Creatine_neutral.png|alt=Creatine molecule]] | |||
| caption = Structure of the creatine molecule | |||
| synonyms = X-linked creatine deficiency | |||
| pronounce = | |||
| specialty = [[Medical genetics]] | |||
| symptoms = [[Intellectual disability]], [[speech delay]], [[seizures]], [[autism spectrum disorder]] | |||
| onset = [[Infancy]] or [[early childhood]] | |||
| duration = [[Lifelong]] | |||
| causes = Mutations in the [[SLC6A8]] gene | |||
| risks = | |||
| diagnosis = [[Genetic testing]], [[magnetic resonance spectroscopy]] | |||
| differential = [[Cerebral palsy]], [[autism]], other [[metabolic disorders]] | |||
| treatment = [[Creatine supplementation]] (ineffective), [[symptomatic treatment]] | |||
| medication = [[Anticonvulsants]], [[behavioral therapy]] | |||
| prognosis = Variable, often involves lifelong management | |||
| frequency = Estimated 1 in 100,000 to 1 in 250,000 males | |||
| deaths = | |||
}} | |||
[[File:Creatine_neutral.png|Creatine neutral|left|thumb]] '''Creatine Transporter Defect''' (CTD) is a rare [[genetic disorder]] that affects the body's ability to transport [[creatine]], a key molecule in energy storage and supply, into cells. This condition primarily impacts the [[brain]], where creatine plays a crucial role in energy metabolism, leading to various neurological and developmental issues. CTD is classified under the broader category of [[creatine deficiency syndromes]], which also includes [[arginine:glycine amidinotransferase deficiency]] and [[guanidinoacetate methyltransferase deficiency]]. | |||
== Causes == | == Causes == | ||
CTD is caused by mutations in the SLC6A8 gene, which encodes the creatine transporter protein. This protein is responsible for the uptake of creatine into cells, especially in the brain and muscle tissues. Mutations in the SLC6A8 gene lead to dysfunctional or absent creatine transporter proteins, resulting in reduced creatine uptake and subsequent energy deficits in cells. | CTD is caused by mutations in the SLC6A8 gene, which encodes the creatine transporter protein. This protein is responsible for the uptake of creatine into cells, especially in the brain and muscle tissues. Mutations in the SLC6A8 gene lead to dysfunctional or absent creatine transporter proteins, resulting in reduced creatine uptake and subsequent energy deficits in cells. | ||
== Symptoms == | == Symptoms == | ||
The symptoms of Creatine Transporter Defect can vary widely among affected individuals but commonly include: | The symptoms of Creatine Transporter Defect can vary widely among affected individuals but commonly include: | ||
| Line 12: | Line 31: | ||
* [[Motor skills|Motor skill]] delays | * [[Motor skills|Motor skill]] delays | ||
* Muscle weakness | * Muscle weakness | ||
== Diagnosis == | == Diagnosis == | ||
Diagnosis of CTD involves a combination of clinical evaluation, biochemical tests, and genetic testing. Biochemical tests may show abnormal levels of creatine or its metabolites in bodily fluids. However, definitive diagnosis is achieved through genetic testing, which can identify mutations in the SLC6A8 gene. | Diagnosis of CTD involves a combination of clinical evaluation, biochemical tests, and genetic testing. Biochemical tests may show abnormal levels of creatine or its metabolites in bodily fluids. However, definitive diagnosis is achieved through genetic testing, which can identify mutations in the SLC6A8 gene. | ||
== Treatment == | == Treatment == | ||
Currently, there is no cure for Creatine Transporter Defect, and treatment focuses on managing symptoms and improving quality of life. Therapeutic strategies may include: | Currently, there is no cure for Creatine Transporter Defect, and treatment focuses on managing symptoms and improving quality of life. Therapeutic strategies may include: | ||
| Line 22: | Line 39: | ||
* Behavioral therapy for managing autism spectrum disorder or ADHD | * Behavioral therapy for managing autism spectrum disorder or ADHD | ||
* Medications to control seizures | * Medications to control seizures | ||
== Prognosis == | == Prognosis == | ||
The prognosis for individuals with Creatine Transporter Defect varies depending on the severity of symptoms and the effectiveness of management strategies. Early intervention and supportive therapies can improve developmental outcomes and quality of life. | The prognosis for individuals with Creatine Transporter Defect varies depending on the severity of symptoms and the effectiveness of management strategies. Early intervention and supportive therapies can improve developmental outcomes and quality of life. | ||
== Research == | == Research == | ||
Research on CTD is ongoing, with studies focusing on understanding the molecular mechanisms of the disease, exploring potential treatments, and developing more effective diagnostic methods. Gene therapy and other novel therapeutic approaches are areas of interest in the quest to find a cure or more effective treatments for CTD. | Research on CTD is ongoing, with studies focusing on understanding the molecular mechanisms of the disease, exploring potential treatments, and developing more effective diagnostic methods. Gene therapy and other novel therapeutic approaches are areas of interest in the quest to find a cure or more effective treatments for CTD. | ||
[[Category:Genetic disorders]] | [[Category:Genetic disorders]] | ||
[[Category:Neurological disorders]] | [[Category:Neurological disorders]] | ||
[[Category:Metabolic disorders]] | [[Category:Metabolic disorders]] | ||
{{medicine-stub}} | {{medicine-stub}} | ||
Latest revision as of 13:35, 5 April 2025

Editor-In-Chief: Prab R Tumpati, MD
Obesity, Sleep & Internal medicine
Founder, WikiMD Wellnesspedia &
W8MD's medical weight loss NYC, sleep center NYC
Philadelphia medical weight loss and Philadelphia sleep clinics
| Creatine transporter defect | |
|---|---|
| |
| Synonyms | X-linked creatine deficiency |
| Pronounce | |
| Specialty | Medical genetics |
| Symptoms | Intellectual disability, speech delay, seizures, autism spectrum disorder |
| Complications | N/A |
| Onset | Infancy or early childhood |
| Duration | Lifelong |
| Types | N/A |
| Causes | Mutations in the SLC6A8 gene |
| Risks | |
| Diagnosis | Genetic testing, magnetic resonance spectroscopy |
| Differential diagnosis | Cerebral palsy, autism, other metabolic disorders |
| Prevention | N/A |
| Treatment | Creatine supplementation (ineffective), symptomatic treatment |
| Medication | Anticonvulsants, behavioral therapy |
| Prognosis | Variable, often involves lifelong management |
| Frequency | Estimated 1 in 100,000 to 1 in 250,000 males |
| Deaths | |

Creatine Transporter Defect (CTD) is a rare genetic disorder that affects the body's ability to transport creatine, a key molecule in energy storage and supply, into cells. This condition primarily impacts the brain, where creatine plays a crucial role in energy metabolism, leading to various neurological and developmental issues. CTD is classified under the broader category of creatine deficiency syndromes, which also includes arginine:glycine amidinotransferase deficiency and guanidinoacetate methyltransferase deficiency.
Causes[edit]
CTD is caused by mutations in the SLC6A8 gene, which encodes the creatine transporter protein. This protein is responsible for the uptake of creatine into cells, especially in the brain and muscle tissues. Mutations in the SLC6A8 gene lead to dysfunctional or absent creatine transporter proteins, resulting in reduced creatine uptake and subsequent energy deficits in cells.
Symptoms[edit]
The symptoms of Creatine Transporter Defect can vary widely among affected individuals but commonly include:
- Intellectual disability
- Speech delay and other language impairments
- Behavioral disorders such as autism spectrum disorder and ADHD
- Seizures
- Motor skill delays
- Muscle weakness
Diagnosis[edit]
Diagnosis of CTD involves a combination of clinical evaluation, biochemical tests, and genetic testing. Biochemical tests may show abnormal levels of creatine or its metabolites in bodily fluids. However, definitive diagnosis is achieved through genetic testing, which can identify mutations in the SLC6A8 gene.
Treatment[edit]
Currently, there is no cure for Creatine Transporter Defect, and treatment focuses on managing symptoms and improving quality of life. Therapeutic strategies may include:
- Speech therapy for language impairments
- Physical therapy and occupational therapy for motor skill development
- Behavioral therapy for managing autism spectrum disorder or ADHD
- Medications to control seizures
Prognosis[edit]
The prognosis for individuals with Creatine Transporter Defect varies depending on the severity of symptoms and the effectiveness of management strategies. Early intervention and supportive therapies can improve developmental outcomes and quality of life.
Research[edit]
Research on CTD is ongoing, with studies focusing on understanding the molecular mechanisms of the disease, exploring potential treatments, and developing more effective diagnostic methods. Gene therapy and other novel therapeutic approaches are areas of interest in the quest to find a cure or more effective treatments for CTD.
