Post-vagotomy diarrhea: Difference between revisions
CSV import |
CSV import Tags: mobile edit mobile web edit |
||
| Line 1: | Line 1: | ||
== Post-vagotomy diarrhea == | |||
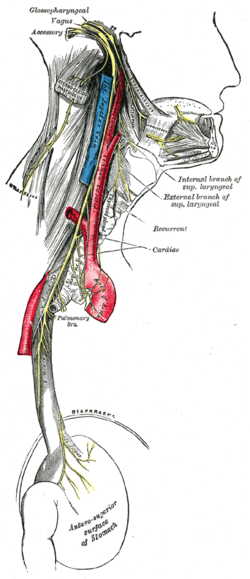
[[File:Gray793.png|thumb|right|200px|Diagram of the stomach and vagus nerve.]] | |||
'''Post-vagotomy diarrhea''' is a condition that can occur after a [[vagotomy]], a surgical procedure where the [[vagus nerve]] is cut to reduce acid secretion in the treatment of [[peptic ulcer disease]]. This condition is characterized by frequent, watery bowel movements and can significantly affect the quality of life of patients who have undergone this surgery. | |||
== | == Pathophysiology == | ||
The [[vagus nerve]] plays a crucial role in the regulation of [[gastric motility]] and [[gastric acid secretion]]. When the vagus nerve is severed, there is a disruption in the normal coordination of the [[gastrointestinal tract]], leading to rapid gastric emptying and increased intestinal motility. This can result in diarrhea as the intestines do not have sufficient time to absorb water from the chyme. | |||
== Clinical features == | |||
Patients with post-vagotomy diarrhea typically present with: | |||
* Frequent, watery stools | |||
* Abdominal cramping | |||
* Urgency to defecate | |||
* Possible [[dehydration]] if diarrhea is severe | |||
The symptoms can vary in intensity and may be influenced by dietary factors and the extent of the vagotomy. | |||
== Management == | |||
Management of post-vagotomy diarrhea involves both dietary modifications and pharmacological interventions. Patients are often advised to: | |||
* Eat smaller, more frequent meals | |||
* Avoid foods that exacerbate symptoms, such as high-fat or spicy foods | |||
* Increase dietary fiber intake to help solidify stools | |||
Pharmacological treatments may include: | |||
* [[Antidiarrheal agents]] such as loperamide | |||
* [[Bile acid sequestrants]] if bile acid malabsorption is suspected | |||
== Prognosis == | |||
The prognosis for post-vagotomy diarrhea varies. Some patients experience a reduction in symptoms over time as the body adapts to the changes in gastrointestinal function. However, others may continue to experience symptoms long-term and require ongoing management. | |||
== Related pages == | |||
* [[Vagotomy]] | |||
* [[Peptic ulcer disease]] | |||
* [[Gastrointestinal tract]] | |||
* [[Gastric motility]] | |||
[[Category:Gastroenterology]] | |||
Revision as of 11:36, 15 February 2025
Post-vagotomy diarrhea
Post-vagotomy diarrhea is a condition that can occur after a vagotomy, a surgical procedure where the vagus nerve is cut to reduce acid secretion in the treatment of peptic ulcer disease. This condition is characterized by frequent, watery bowel movements and can significantly affect the quality of life of patients who have undergone this surgery.
Pathophysiology
The vagus nerve plays a crucial role in the regulation of gastric motility and gastric acid secretion. When the vagus nerve is severed, there is a disruption in the normal coordination of the gastrointestinal tract, leading to rapid gastric emptying and increased intestinal motility. This can result in diarrhea as the intestines do not have sufficient time to absorb water from the chyme.
Clinical features
Patients with post-vagotomy diarrhea typically present with:
- Frequent, watery stools
- Abdominal cramping
- Urgency to defecate
- Possible dehydration if diarrhea is severe
The symptoms can vary in intensity and may be influenced by dietary factors and the extent of the vagotomy.
Management
Management of post-vagotomy diarrhea involves both dietary modifications and pharmacological interventions. Patients are often advised to:
- Eat smaller, more frequent meals
- Avoid foods that exacerbate symptoms, such as high-fat or spicy foods
- Increase dietary fiber intake to help solidify stools
Pharmacological treatments may include:
- Antidiarrheal agents such as loperamide
- Bile acid sequestrants if bile acid malabsorption is suspected
Prognosis
The prognosis for post-vagotomy diarrhea varies. Some patients experience a reduction in symptoms over time as the body adapts to the changes in gastrointestinal function. However, others may continue to experience symptoms long-term and require ongoing management.