Pancreatic serous cystadenoma: Difference between revisions
CSV import Tags: mobile edit mobile web edit |
CSV import |
||
| Line 29: | Line 29: | ||
{{Medicine-stub}} | {{Medicine-stub}} | ||
== Pancreatic serous cystadenoma == | |||
<gallery> | |||
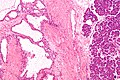
File:Pancreatic_serous_cystadenoma_-_intermed_mag.jpg|Pancreatic serous cystadenoma - intermediate magnification | |||
File:Serous_cystadenoma_of_the_pancreatic_head..jpg|Serous cystadenoma of the pancreatic head | |||
File:Pancreatic_serous_cystadenoma_-_intermed_mag.jpg|Pancreatic serous cystadenoma - intermediate magnification | |||
File:Pancreatic_serous_cystadenoma_-_high_mag.jpg|Pancreatic serous cystadenoma - high magnification | |||
File:Pancreatic_serous_cystadenoma_-_very_high_mag.jpg|Pancreatic serous cystadenoma - very high magnification | |||
File:Pancreatic_serous_cystadenoma_(1).jpg|Pancreatic serous cystadenoma | |||
File:Pancreatic_serous_cystic_tumor_(3).jpg|Pancreatic serous cystic tumor | |||
File:Relative_incidence_of_pancreatic_neoplasms.png|Relative incidence of pancreatic neoplasms | |||
</gallery> | |||
Revision as of 11:56, 18 February 2025
Pancreatic serous cystadenoma (PSC), also known as serous cystic neoplasm of the pancreas, is a benign tumor of the pancreas. It is a type of pancreatic cyst that is typically non-cancerous and is most commonly found in the body or tail of the pancreas. PSCs account for about 1-2% of all pancreatic tumors and are more frequently diagnosed in women, particularly in the sixth and seventh decades of life.
Etiology and Pathogenesis
The exact cause of pancreatic serous cystadenoma is not well understood. These tumors are thought to originate from the centroacinar cells, which are part of the pancreatic ducts. Genetic mutations have been identified in some cases, but the significance of these mutations is still under investigation.
Clinical Presentation
Patients with pancreatic serous cystadenoma often present with non-specific symptoms or are asymptomatic. When symptoms do occur, they may include abdominal pain, nausea, and vomiting. The growth of the tumor can lead to the compression of adjacent organs, causing additional symptoms such as jaundice.
Diagnosis
Diagnosis of pancreatic serous cystadenoma typically involves a combination of imaging studies and histological examination. Computed tomography (CT) scans and magnetic resonance imaging (MRI) are commonly used to visualize the cystic nature of the tumor and its location within the pancreas. Endoscopic ultrasound (EUS) with fine-needle aspiration (FNA) may be employed to obtain tissue samples for histological analysis.
Treatment
The treatment approach for pancreatic serous cystadenoma depends on the size of the tumor, its location, and the presence of symptoms. Asymptomatic small tumors may be managed with regular monitoring and follow-up imaging studies. Surgical resection is recommended for symptomatic tumors, tumors that are increasing in size, or when malignancy cannot be ruled out. The most common surgical procedures are the distal pancreatectomy and enucleation.
Prognosis
The prognosis for patients with pancreatic serous cystadenoma is generally excellent, as these tumors are benign and have a low potential for malignancy. Surgical removal of the tumor is usually curative, and recurrence is rare.
Epidemiology
Pancreatic serous cystadenomas are more common in women than in men and are typically diagnosed in individuals over the age of 60. The incidence of these tumors is relatively low, making up about 1-2% of all pancreatic neoplasms.
See Also
Pancreatic serous cystadenoma
-
Pancreatic serous cystadenoma - intermediate magnification
-
Serous cystadenoma of the pancreatic head
-
Pancreatic serous cystadenoma - intermediate magnification
-
Pancreatic serous cystadenoma - high magnification
-
Pancreatic serous cystadenoma - very high magnification
-
Pancreatic serous cystadenoma
-
Pancreatic serous cystic tumor
-
Relative incidence of pancreatic neoplasms