Primary sclerosing cholangitis: Difference between revisions
No edit summary |
CSV import |
||
| Line 1: | Line 1: | ||
{{SI}} | |||
{{Infobox medical condition | |||
| name = Primary sclerosing cholangitis | |||
| image = [[File:Cholangiogram_of_primary_sclerosing_cholangitis.jpg|250px]] | |||
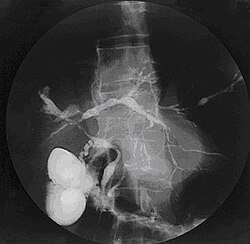
| caption = Cholangiogram showing primary sclerosing cholangitis | |||
| field = [[Gastroenterology]] | |||
| synonyms = PSC | |||
| symptoms = [[Jaundice]], [[itching]], [[fatigue]], [[abdominal pain]] | |||
| complications = [[Cholangiocarcinoma]], [[liver failure]], [[portal hypertension]] | |||
| onset = Typically between ages 30 and 40 | |||
| duration = Chronic | |||
| causes = Unknown, possibly [[autoimmune disease]] | |||
| risks = [[Inflammatory bowel disease]], particularly [[ulcerative colitis]] | |||
| diagnosis = [[Magnetic resonance cholangiopancreatography|MRCP]], [[liver biopsy]] | |||
| differential = [[Primary biliary cholangitis]], [[bile duct cancer]], [[choledocholithiasis]] | |||
| treatment = [[Ursodeoxycholic acid]], [[endoscopic retrograde cholangiopancreatography|ERCP]], [[liver transplantation]] | |||
| medication = [[Ursodeoxycholic acid]], [[immunosuppressants]] | |||
| prognosis = Variable, often progressive | |||
| frequency = 1 in 10,000 people | |||
| deaths = Related to complications such as liver failure and cholangiocarcinoma | |||
}} | |||
Primary sclerosing cholangitis (PSC) is a long-term progressive disease of the liver and gallbladder characterized by inflammation and scarring of the bile ducts which normally allow bile to drain from the gallbladder. This can lead to liver damage and eventually, liver failure. | Primary sclerosing cholangitis (PSC) is a long-term progressive disease of the liver and gallbladder characterized by inflammation and scarring of the bile ducts which normally allow bile to drain from the gallbladder. This can lead to liver damage and eventually, liver failure. | ||
==Introduction== | ==Introduction== | ||
PSC is a chronic disease characterized by a progressive course of cholestasis with inflammation and fibrosis of the intrahepatic and extrahepatic bile ducts. The disease affects both adults and children, but is more common in males. The pathogenesis of PSC remains unclear, but it is often associated with inflammatory bowel disease (IBD), particularly ulcerative colitis.<ref>[[Chapman, R.]], Fevery, J., Kalloo, A., Nagorney, D. M., Boberg, K. M., Shneider, B., & Gores, G. J. (2010). Diagnosis and management of primary sclerosing cholangitis. Hepatology, 51(2), 660-678.</ref> | PSC is a chronic disease characterized by a progressive course of cholestasis with inflammation and fibrosis of the intrahepatic and extrahepatic bile ducts. The disease affects both adults and children, but is more common in males. The pathogenesis of PSC remains unclear, but it is often associated with inflammatory bowel disease (IBD), particularly ulcerative colitis.<ref>[[Chapman, R.]], Fevery, J., Kalloo, A., Nagorney, D. M., Boberg, K. M., Shneider, B., & Gores, G. J. (2010). Diagnosis and management of primary sclerosing cholangitis. Hepatology, 51(2), 660-678.</ref> | ||
==Causes== | ==Causes== | ||
The exact cause of PSC is unknown, but it's thought to be related to a combination of genetic and environmental factors. The strong association between PSC and IBD suggests an autoimmune component to the disease.<ref>[[Boonstra, K.]], Weersma, R. K., & van Erpecum, K. J. (2013). Epidemiology of primary sclerosing cholangitis and primary biliary cirrhosis: a systematic review. Journal of hepatology, 58(5), 958-967.</ref> | The exact cause of PSC is unknown, but it's thought to be related to a combination of genetic and environmental factors. The strong association between PSC and IBD suggests an autoimmune component to the disease.<ref>[[Boonstra, K.]], Weersma, R. K., & van Erpecum, K. J. (2013). Epidemiology of primary sclerosing cholangitis and primary biliary cirrhosis: a systematic review. Journal of hepatology, 58(5), 958-967.</ref> | ||
==Symptoms== | ==Symptoms== | ||
Many people with PSC have no symptoms at all. When symptoms do occur, they may include fatigue, itching, abdominal pain, fever, and jaundice. Over time, as the liver's function decreases, symptoms of cirrhosis can develop, including fluid buildup, bleeding from enlarged veins, and confusion.<ref>[[Chapman, R. W.]] (2015). Risk factors for biliary neoplasia in primary sclerosing cholangitis. Journal of hepatology, 62(5), 1065-1067.</ref> | Many people with PSC have no symptoms at all. When symptoms do occur, they may include fatigue, itching, abdominal pain, fever, and jaundice. Over time, as the liver's function decreases, symptoms of cirrhosis can develop, including fluid buildup, bleeding from enlarged veins, and confusion.<ref>[[Chapman, R. W.]] (2015). Risk factors for biliary neoplasia in primary sclerosing cholangitis. Journal of hepatology, 62(5), 1065-1067.</ref> | ||
==Diagnosis== | ==Diagnosis== | ||
Diagnosis is often made through a combination of liver function tests, imaging studies such as MRCP or ERCP, and sometimes liver biopsy. The hallmark of PSC on imaging is a pattern of strictures and dilations of the bile ducts, often described as a 'beaded' appearance.<ref>[[Lazaridis, K. N.]], & LaRusso, N. F. (2016). Primary Sclerosing Cholangitis. New England Journal of Medicine, 375(12), 1161-1170.</ref> | Diagnosis is often made through a combination of liver function tests, imaging studies such as MRCP or ERCP, and sometimes liver biopsy. The hallmark of PSC on imaging is a pattern of strictures and dilations of the bile ducts, often described as a 'beaded' appearance.<ref>[[Lazaridis, K. N.]], & LaRusso, N. F. (2016). Primary Sclerosing Cholangitis. New England Journal of Medicine, 375(12), 1161-1170.</ref> | ||
==Treatment== | ==Treatment== | ||
There's currently no known cure for PSC, and treatment is mainly supportive. This can include medication to relieve itching and antibiotics for infections. In severe cases, a liver transplant may be necessary.<ref>[[Karlsen, T. H.]], Folseraas, T., Thorburn, D., & Vesterhus, M. (2014). Primary sclerosing cholangitis – a comprehensive review. Journal of hepatology, 59(5), 1069-1079.</ref> | There's currently no known cure for PSC, and treatment is mainly supportive. This can include medication to relieve itching and antibiotics for infections. In severe cases, a liver transplant may be necessary.<ref>[[Karlsen, T. H.]], Folseraas, T., Thorburn, D., & Vesterhus, M. (2014). Primary sclerosing cholangitis – a comprehensive review. Journal of hepatology, 59(5), 1069-1079.</ref> | ||
==Prognosis== | ==Prognosis== | ||
The course of PSC is highly variable, ranging from a relatively indolent course to rapid progression to cirrhosis and its complications. PSC is a serious condition that can lead to other health problems, such as liver cirrhosis, bile duct infection, liver failure, and liver cancer. | The course of PSC is highly variable, ranging from a relatively indolent course to rapid progression to cirrhosis and its complications. PSC is a serious condition that can lead to other health problems, such as liver cirrhosis, bile duct infection, liver failure, and liver cancer. | ||
==See Also== | ==See Also== | ||
* [[Liver Disease]] | * [[Liver Disease]] | ||
| Line 25: | Line 39: | ||
* [[Inflammatory bowel disease]] | * [[Inflammatory bowel disease]] | ||
* [[Ulcerative colitis]] | * [[Ulcerative colitis]] | ||
==References== | ==References== | ||
<references /> | <references /> | ||
Latest revision as of 15:31, 8 April 2025

Editor-In-Chief: Prab R Tumpati, MD
Obesity, Sleep & Internal medicine
Founder, WikiMD Wellnesspedia &
W8MD medical weight loss NYC and sleep center NYC
| Primary sclerosing cholangitis | |
|---|---|
| |
| Synonyms | PSC |
| Pronounce | N/A |
| Specialty | N/A |
| Symptoms | Jaundice, itching, fatigue, abdominal pain |
| Complications | Cholangiocarcinoma, liver failure, portal hypertension |
| Onset | Typically between ages 30 and 40 |
| Duration | Chronic |
| Types | N/A |
| Causes | Unknown, possibly autoimmune disease |
| Risks | Inflammatory bowel disease, particularly ulcerative colitis |
| Diagnosis | MRCP, liver biopsy |
| Differential diagnosis | Primary biliary cholangitis, bile duct cancer, choledocholithiasis |
| Prevention | N/A |
| Treatment | Ursodeoxycholic acid, ERCP, liver transplantation |
| Medication | Ursodeoxycholic acid, immunosuppressants |
| Prognosis | Variable, often progressive |
| Frequency | 1 in 10,000 people |
| Deaths | Related to complications such as liver failure and cholangiocarcinoma |
Primary sclerosing cholangitis (PSC) is a long-term progressive disease of the liver and gallbladder characterized by inflammation and scarring of the bile ducts which normally allow bile to drain from the gallbladder. This can lead to liver damage and eventually, liver failure.
Introduction[edit]
PSC is a chronic disease characterized by a progressive course of cholestasis with inflammation and fibrosis of the intrahepatic and extrahepatic bile ducts. The disease affects both adults and children, but is more common in males. The pathogenesis of PSC remains unclear, but it is often associated with inflammatory bowel disease (IBD), particularly ulcerative colitis.<ref>Chapman, R., Fevery, J., Kalloo, A., Nagorney, D. M., Boberg, K. M., Shneider, B., & Gores, G. J. (2010). Diagnosis and management of primary sclerosing cholangitis. Hepatology, 51(2), 660-678.</ref>
Causes[edit]
The exact cause of PSC is unknown, but it's thought to be related to a combination of genetic and environmental factors. The strong association between PSC and IBD suggests an autoimmune component to the disease.<ref>Boonstra, K., Weersma, R. K., & van Erpecum, K. J. (2013). Epidemiology of primary sclerosing cholangitis and primary biliary cirrhosis: a systematic review. Journal of hepatology, 58(5), 958-967.</ref>
Symptoms[edit]
Many people with PSC have no symptoms at all. When symptoms do occur, they may include fatigue, itching, abdominal pain, fever, and jaundice. Over time, as the liver's function decreases, symptoms of cirrhosis can develop, including fluid buildup, bleeding from enlarged veins, and confusion.<ref>Chapman, R. W. (2015). Risk factors for biliary neoplasia in primary sclerosing cholangitis. Journal of hepatology, 62(5), 1065-1067.</ref>
Diagnosis[edit]
Diagnosis is often made through a combination of liver function tests, imaging studies such as MRCP or ERCP, and sometimes liver biopsy. The hallmark of PSC on imaging is a pattern of strictures and dilations of the bile ducts, often described as a 'beaded' appearance.<ref>Lazaridis, K. N., & LaRusso, N. F. (2016). Primary Sclerosing Cholangitis. New England Journal of Medicine, 375(12), 1161-1170.</ref>
Treatment[edit]
There's currently no known cure for PSC, and treatment is mainly supportive. This can include medication to relieve itching and antibiotics for infections. In severe cases, a liver transplant may be necessary.<ref>Karlsen, T. H., Folseraas, T., Thorburn, D., & Vesterhus, M. (2014). Primary sclerosing cholangitis – a comprehensive review. Journal of hepatology, 59(5), 1069-1079.</ref>
Prognosis[edit]
The course of PSC is highly variable, ranging from a relatively indolent course to rapid progression to cirrhosis and its complications. PSC is a serious condition that can lead to other health problems, such as liver cirrhosis, bile duct infection, liver failure, and liver cancer.
See Also[edit]
References[edit]
<references />


