Acute intermittent porphyria: Difference between revisions
No edit summary Tag: visualeditor-wikitext |
CSV import |
||
| Line 1: | Line 1: | ||
'''Other Names:''' AIP; Porphobilinogen deaminase deficiency; PBGD deficiency; Uroporphyrinogen synthase deficiency; UPS deficiency; Porphyria, Swedish type; Hydroxymethylbilane synthase deficiency; HMBS deficiency | |||
{{Infobox medical condition | |||
| name = Acute intermittent porphyria | |||
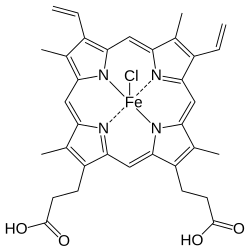
| image =[[File:Porphobilinogen.png|thumb|Porphobilinogen, a key compound in porphyria]] | |||
| caption = Porphobilinogen, a key compound in porphyria | |||
| synonyms = AIP | |||
| pronounce = | |||
| specialty = [[Hematology]], [[Genetics]] | |||
| symptoms = Abdominal pain, vomiting, neuropathy, constipation, confusion | |||
| onset = Typically after puberty | |||
| duration = Episodic | |||
| causes = [[Genetic mutation]] in the [[HMBS]] gene | |||
| risks = [[Hormonal changes]], [[medications]], [[alcohol]], [[fasting]] | |||
| diagnosis = [[Urine test]] for porphobilinogen | |||
| differential = [[Lead poisoning]], [[Guillain–Barré syndrome]], [[appendicitis]] | |||
| treatment = [[Intravenous glucose]], [[heme arginate]] | |||
| medication = [[Hemin]] | |||
| prognosis = Variable, can be life-threatening if untreated | |||
| frequency = 5-10 per 100,000 people | |||
| deaths = Rare with treatment | |||
}} | |||
'''Other Names:''' AIP; Porphobilinogen deaminase deficiency; PBGD deficiency; Uroporphyrinogen synthase deficiency; UPS deficiency; Porphyria, Swedish type; Hydroxymethylbilane synthase deficiency; HMBS deficiency | |||
Acute intermittent porphyria (AIP) is one of the liver (hepatic) [[porphyrias]]. AIP is caused by low levels of [[porphobilinogen deaminase]] (PBGD), an enzyme also often called [[hydroxymethylbilane synthase]]. The low levels of PBGD are generally not sufficient to cause symptoms; however, activating factors such as hormones, drugs, and dietary changes may trigger symptoms. Although most individuals with AIP never develop symptoms, symptomatic individuals typically present with abdominal pain with [[nausea]]. | Acute intermittent porphyria (AIP) is one of the liver (hepatic) [[porphyrias]]. AIP is caused by low levels of [[porphobilinogen deaminase]] (PBGD), an enzyme also often called [[hydroxymethylbilane synthase]]. The low levels of PBGD are generally not sufficient to cause symptoms; however, activating factors such as hormones, drugs, and dietary changes may trigger symptoms. Although most individuals with AIP never develop symptoms, symptomatic individuals typically present with abdominal pain with [[nausea]]. | ||
| Line 15: | Line 36: | ||
=='''Cause '''== | =='''Cause '''== | ||
AIP is caused by the deficiency of an [[enzyme]] | AIP is caused by the deficiency of an [[enzyme]]  called [[porphobilinogen deaminase]] (PBGD), also known as hydroxymethylbilane synthase (HMBS) and formerly known as [[uroporphyrinogen I-synthase]]. The deficiency of PBGD is caused by a [[mutation]] in the [[''HMBS'']]gene . The ''HMBS'' gene is the only gene known to be associated with AIP. However, the deficiency of PBGD alone is not enough to cause AIP. Other activating factors (e.g.,[[harmones]], drugs, dietary changes) must also be present. | ||
=='''Inheritance'''== | =='''Inheritance'''== | ||
[[File:Autosomal dominant - en.svg|thumb|right|[[Autosomal dominant]] pattern, a 50/50 chance.]] | [[File:Autosomal dominant - en.svg|thumb|right|[[Autosomal dominant]] pattern, a 50/50 chance.]] | ||
AIP is [[inherited]] | AIP is [[inherited]] in an [[autosomal dominant]] fashion, which means only one of the two [[''HMBS'']][[genes]] needs to have a disease-causing [[mutation]]  to decrease [[enzyme]] activity and cause symptoms. | ||
<br /> | <br /> | ||
=='''Diagnosis'''== | =='''Diagnosis'''== | ||
Diagnosis of AIP is suspected in individuals with otherwise unexplained severe, acute abdominal pain without physical signs. The finding of increased levels of [[delta-aminolevulinic acid]] (ALA) and [[porphobilinogen]] (PBG) in urine establishes that one of the acute porphyrias is present. If PBGD is deficient in normal red blod cells, the diagnosis of AIP is established. | Diagnosis of AIP is suspected in individuals with otherwise unexplained severe, acute abdominal pain without physical signs. The finding of increased levels of [[delta-aminolevulinic acid]] (ALA) and [[porphobilinogen]] (PBG) in urine establishes that one of the acute porphyrias is present. If PBGD is deficient in normal red blod cells, the diagnosis of AIP is established. | ||
The diagnosis is confirmed in individuals with a disease-causing mutation in the ''HMBS''gene , the only gene known to be associated with AIP, which encodes the [[erythrocyte]] | The diagnosis is confirmed in individuals with a disease-causing mutation in the ''HMBS''gene , the only gene known to be associated with AIP, which encodes the [[erythrocyte]] hydroxymethylbilane synthase . | ||
[[Molecular genetic testing]] of the ''HMBS'' gene detects more than 98% of affected individuals and is available in clinical laboratories. | [[Molecular genetic testing]] of the ''HMBS'' gene detects more than 98% of affected individuals and is available in clinical laboratories. | ||
Latest revision as of 02:54, 4 April 2025
| Acute intermittent porphyria | |
|---|---|
 | |
| Synonyms | AIP |
| Pronounce | |
| Specialty | Hematology, Genetics |
| Symptoms | Abdominal pain, vomiting, neuropathy, constipation, confusion |
| Complications | N/A |
| Onset | Typically after puberty |
| Duration | Episodic |
| Types | N/A |
| Causes | Genetic mutation in the HMBS gene |
| Risks | Hormonal changes, medications, alcohol, fasting |
| Diagnosis | Urine test for porphobilinogen |
| Differential diagnosis | Lead poisoning, Guillain–Barré syndrome, appendicitis |
| Prevention | N/A |
| Treatment | Intravenous glucose, heme arginate |
| Medication | Hemin |
| Prognosis | Variable, can be life-threatening if untreated |
| Frequency | 5-10 per 100,000 people |
| Deaths | Rare with treatment |
Other Names: AIP; Porphobilinogen deaminase deficiency; PBGD deficiency; Uroporphyrinogen synthase deficiency; UPS deficiency; Porphyria, Swedish type; Hydroxymethylbilane synthase deficiency; HMBS deficiency
Acute intermittent porphyria (AIP) is one of the liver (hepatic) porphyrias. AIP is caused by low levels of porphobilinogen deaminase (PBGD), an enzyme also often called hydroxymethylbilane synthase. The low levels of PBGD are generally not sufficient to cause symptoms; however, activating factors such as hormones, drugs, and dietary changes may trigger symptoms. Although most individuals with AIP never develop symptoms, symptomatic individuals typically present with abdominal pain with nausea.
Cause [edit]
AIP is caused by the deficiency of an enzyme  called porphobilinogen deaminase (PBGD), also known as hydroxymethylbilane synthase (HMBS) and formerly known as uroporphyrinogen I-synthase. The deficiency of PBGD is caused by a mutation in the ''HMBS''gene . The HMBS gene is the only gene known to be associated with AIP. However, the deficiency of PBGD alone is not enough to cause AIP. Other activating factors (e.g.,harmones, drugs, dietary changes) must also be present.
Inheritance[edit]

AIP is inherited in an autosomal dominant fashion, which means only one of the two ''HMBS''genes needs to have a disease-causing mutation  to decrease enzyme activity and cause symptoms.
Diagnosis[edit]
Diagnosis of AIP is suspected in individuals with otherwise unexplained severe, acute abdominal pain without physical signs. The finding of increased levels of delta-aminolevulinic acid (ALA) and porphobilinogen (PBG) in urine establishes that one of the acute porphyrias is present. If PBGD is deficient in normal red blod cells, the diagnosis of AIP is established. The diagnosis is confirmed in individuals with a disease-causing mutation in the HMBSgene , the only gene known to be associated with AIP, which encodes the erythrocyte hydroxymethylbilane synthase .
Molecular genetic testing of the HMBS gene detects more than 98% of affected individuals and is available in clinical laboratories.
Treatment[edit]
Treatment of AIP may vary based on the trigger of the attack and the symptoms present. Treatment may include stopping medications that cause or worsen the symptoms, treating any infections which may be present, administration of pain medication, monitoring fluid balance and/or correcting electrolyte disturbances, monitoring neurologic status and administering respiratory support. Mild attacks can be manged with increased caloric intake and fluid replacement. Recurrent acute attacks should be managed by a porphyria specialist. Hospitalization is often necessary.
Panhematin, an intravenous medication used to correct heme deficiency, may also be prescribed.
The medication(s) listed below have been approved by the Food and Drug Administration (FDA) as orphan products for treatment of this condition.
- Hemin (Brand name: Panhematin)
External links[edit]
|
|
|
| Heme metabolism disorders | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
NIH genetic and rare disease info[edit]
Acute intermittent porphyria is a rare disease.
| Rare and genetic diseases | ||||||
|---|---|---|---|---|---|---|
|
Rare diseases - Acute intermittent porphyria
|


