Andersen–Tawil syndrome: Difference between revisions
CSV import |
No edit summary |
||
| Line 25: | Line 25: | ||
| alt = | | alt = | ||
}} | }} | ||
'''Andersen–Tawil syndrome''' ('''ATS'''), also known as '''Andersen syndrome''' or '''long QT syndrome 7''', is a rare [[genetic disorder]] that affects multiple systems in the body, including the [[cardiovascular system]], [[musculoskeletal system]], and [[nervous system]]. It is characterized by three main features: | |||
* Abnormal [[cardiac conduction]] leading to an extended [[QT interval]] and a predisposition to [[ventricular arrhythmias]]. | |||
* Periodic episodes of [[muscle weakness]], known as [[hypokalemic periodic paralysis]]. | |||
* Distinctive physical abnormalities affecting the [[face]], [[limbs]], and [[spine]]. | |||
This condition follows an [[autosomal dominant]] pattern of inheritance and is most commonly associated with mutations in the '''[[KCNJ2]]''' gene, which encodes a [[potassium ion channel]] essential for cardiac and muscle function. Management of Andersen–Tawil syndrome primarily focuses on controlling [[arrhythmias]], preventing sudden cardiac death, and managing periodic paralysis episodes. | |||
Andersen–Tawil syndrome | == Clinical Features == | ||
Andersen–Tawil syndrome presents with a characteristic triad of: | |||
# '''Cardiac Abnormalities''' – Prolongation of the [[QT interval]], [[ventricular tachycardia]], and increased risk of [[sudden cardiac events]]. | |||
# '''Neuromuscular Manifestations''' – Recurrent episodes of [[muscle weakness]], often triggered by [[hypokalemia]]. | |||
# '''Dysmorphic Features''' – Distinctive [[craniofacial]], [[skeletal]], and [[limb]] anomalies. | |||
== | === Cardiac Abnormalities === | ||
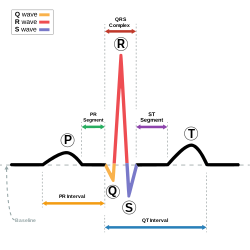
The [[electrocardiogram]] (ECG) of an individual with Andersen–Tawil syndrome typically shows: | |||
[[ | * '''Prolonged QT interval''', increasing the risk of [[ventricular arrhythmias]]. | ||
* '''Frequent premature ventricular contractions (PVCs)''', which may progress to [[ventricular tachycardia]]. | |||
* '''Bidirectional ventricular tachycardia''', a characteristic arrhythmia associated with ATS. | |||
* '''Palpitations, dizziness, and syncope''', especially during [[exercise]] or [[emotional stress]]. | |||
While ATS is associated with [[long QT syndrome]], the risk of sudden cardiac death is lower compared to other forms of [[congenital long QT syndromes]]. | |||
== | === Neuromuscular Manifestations === | ||
* Recurrent episodes of [[muscle weakness]], lasting from minutes to hours. | |||
* Weakness is typically '''triggered by low potassium levels''' ([[hypokalemia]]). | |||
* Episodes may be provoked by '''exercise, stress, fasting, or certain medications'''. | |||
* Some patients experience '''persistent muscle weakness''' between episodes. | |||
=== Physical Abnormalities === | |||
The '''skeletal and craniofacial abnormalities''' seen in Andersen–Tawil syndrome include: | |||
* '''Low-set ears''' and '''widely spaced eyes''' ([[hypertelorism]]). | |||
* '''Micrognathia''' – A small lower jaw. | |||
* '''Clinodactyly''' – Abnormal curvature of the '''fifth finger'''. | |||
* '''Syndactyly''' – Fusion of two or more fingers or toes. | |||
* '''Scoliosis''' – Abnormal curvature of the '''spine'''. | |||
* '''Short stature''' and '''high-arched palate'''. | |||
== Genetics and Pathophysiology == | |||
Andersen–Tawil syndrome is caused by mutations in the '''[[KCNJ2]]''' gene, which encodes the '''Kir2.1 potassium channel'''. This ion channel plays a crucial role in regulating: | |||
* '''Cardiac repolarization''', ensuring proper electrical conduction in the heart. | |||
* '''Muscle membrane potential''', preventing abnormal muscle contractions and weakness. | |||
=== Genetic Inheritance === | |||
* ATS follows an '''autosomal dominant''' inheritance pattern. | |||
* Some cases result from '''de novo mutations''', meaning they occur spontaneously without a family history. | |||
* '''Type 1 ATS''' (60% of cases) results from mutations in '''KCNJ2'''. | |||
* '''Type 2 ATS''' (40% of cases) is genetically undefined but may involve mutations in '''[[KCNJ5]]'''. | |||
=== Mechanisms of Disease === | |||
* '''Reduced Kir2.1 channel function''' results in abnormal '''potassium ion transport'''. | |||
* '''Increased cardiac excitability''' leads to '''prolonged repolarization''' and susceptibility to arrhythmias. | |||
* '''Muscle hyperexcitability and depolarization''' cause episodes of periodic paralysis. | |||
== Diagnosis == | |||
A diagnosis of Andersen–Tawil syndrome is based on a combination of: | |||
* '''Clinical criteria''' (triad of cardiac, neuromuscular, and skeletal features). | |||
* '''Electrocardiogram (ECG)''' findings (QT prolongation, bidirectional VT). | |||
* '''Genetic testing''' to identify mutations in '''KCNJ2''' or related genes. | |||
== | === Diagnostic Criteria === | ||
A diagnosis is likely if two of the following are present: | |||
1. '''Periodic paralysis''' with episodes of muscle weakness. | |||
2. '''Prolonged QT interval''' and ventricular arrhythmias. | |||
3. '''Distinctive physical features''' such as '''clinodactyly, low-set ears, and scoliosis'''. | |||
4. '''A family history of Andersen–Tawil syndrome'''. | |||
=== Differential Diagnosis === | |||
[[ | Conditions that may mimic Andersen–Tawil syndrome include: | ||
* '''[[Long QT syndrome]] (types 1–6)''' – Prolonged QT interval without skeletal abnormalities. | |||
* '''[[Catecholaminergic polymorphic ventricular tachycardia]] (CPVT)''' – Exercise-induced ventricular arrhythmias. | |||
* '''[[Familial periodic paralysis]] (hyperkalemic or hypokalemic forms)''' – Muscle weakness without cardiac abnormalities. | |||
== Treatment and Management == | |||
As a '''genetic disorder''', Andersen–Tawil syndrome has no cure. However, treatment focuses on: | |||
* '''Preventing life-threatening arrhythmias'''. | |||
* '''Managing periodic paralysis episodes'''. | |||
* '''Monitoring and treating skeletal abnormalities'''. | |||
=== Cardiac Management === | |||
* '''Beta-blockers''' (e.g., '''propranolol''') help prevent arrhythmias by reducing heart excitability. | |||
* '''Flecainide and verapamil''' may be used for arrhythmia suppression. | |||
* '''Implantable cardioverter-defibrillators (ICDs)''' are considered for high-risk patients who have experienced life-threatening arrhythmias. | |||
== | === Managing Periodic Paralysis === | ||
* '''Potassium supplementation''' during episodes can help '''restore muscle function'''. | |||
* '''Acetazolamide (a carbonic anhydrase inhibitor)''' may reduce the frequency of attacks. | |||
* '''Avoiding triggers''' such as fasting, stress, and excessive exercise is recommended. | |||
=== Lifestyle Considerations === | |||
* '''Avoid medications that prolong the QT interval''', such as '''amiodarone''' and '''sotalol'''. | |||
* '''Mild to moderate exercise''' is encouraged, but '''competitive sports''' should be avoided due to arrhythmia risks. | |||
* '''Regular monitoring with ECG and Holter monitoring''' is essential to track arrhythmia burden. | |||
== | == Prognosis == | ||
The | The '''prognosis of Andersen–Tawil syndrome''' varies depending on the severity of symptoms: | ||
* '''Most individuals lead normal lives''' with appropriate treatment. | |||
* '''Severe arrhythmias may increase the risk of sudden cardiac events''', requiring close monitoring. | |||
* '''Skeletal abnormalities''' can impact mobility and may require orthopedic interventions. | |||
== Epidemiology == | == Epidemiology == | ||
Andersen–Tawil syndrome is | Andersen–Tawil syndrome is an '''extremely rare condition''', affecting '''approximately 1 in 1,000,000 individuals worldwide'''. Due to its rarity, many cases remain '''undiagnosed or misdiagnosed'''. | ||
== History == | == History == | ||
The condition was first described in '''1971''' by '''Dr. Ellen Damgaard Andersen''', who documented the triad of symptoms. Further contributions were made by '''Dr. Rabi Tawil''' in 1994, leading to the modern understanding of the disorder. | |||
* '' | == See Also == | ||
* '''[[Long QT syndrome]]''' | |||
* '''[[Periodic paralysis]]''' | |||
* '''[[Arrhythmogenic disorders]]''' | |||
* '''[[Ion channel disorders]]''' | |||
== External | == External Links == | ||
{{Medical resources | {{Medical resources | ||
| | | DiseasesDB = 700 | ||
| | | ICD10 = {{ICD10|I|45|8|i|45}} | ||
| | | ICD9 = {{ICD9|426.82}}, {{ICD9|794.31}} | ||
| | | OMIM = 170390 | ||
| MedlinePlus = | |||
| | | GeneReviewsNBK = NBK1264 | ||
| GeneReviewsName = Andersen-Tawil syndrome | |||
| Orphanet = 37553 | |||
| | |||
| | |||
| | |||
}} | }} | ||
{{syndromes}} | |||
{{ | [[Category:Cardiac arrhythmias]] | ||
[[Category:Cardiac | |||
[[Category:Channelopathies]] | [[Category:Channelopathies]] | ||
[[Category:Rare | [[Category:Rare diseases]] | ||
[[Category: | [[Category:Neuromuscular disorders]] | ||
[[Category: | [[Category:Genetic syndromes]] | ||
[[Category:Skeletal disorders]] | |||
[[Category:Long QT syndrome]] | |||
Latest revision as of 05:05, 19 March 2025
Rare autosomal dominant genetic disorder
| Andersen–Tawil syndrome | |
|---|---|
| |
| Synonyms | Cardiodysrhythmic potassium-sensitive periodic paralysis, long QT syndrome type 7 |
| Pronounce | |
| Field | Cardiology |
| Symptoms | Abnormal heart rhythms, periodic paralysis, characteristic physical features |
| Complications | Sudden death |
| Onset | Birth |
| Duration | Lifelong |
| Types | Type 1 (KCNQ2 mutation positive), Type 2 (genetic mutation not identified) |
| Causes | Genetic |
| Risks | |
| Diagnosis | Clinical, genetic testing |
| Differential diagnosis | Romano-Ward syndrome, Jervell and Lange-Nielsen syndrome, Timothy syndrome |
| Prevention | |
| Treatment | Medication, implantable cardioverter-defibrillator |
| Medication | Flecainide, beta-blockers, acetazolamide |
| Prognosis | |
| Frequency | 1:1,000,000 |
| Deaths | |
Andersen–Tawil syndrome (ATS), also known as Andersen syndrome or long QT syndrome 7, is a rare genetic disorder that affects multiple systems in the body, including the cardiovascular system, musculoskeletal system, and nervous system. It is characterized by three main features:
- Abnormal cardiac conduction leading to an extended QT interval and a predisposition to ventricular arrhythmias.
- Periodic episodes of muscle weakness, known as hypokalemic periodic paralysis.
- Distinctive physical abnormalities affecting the face, limbs, and spine.
This condition follows an autosomal dominant pattern of inheritance and is most commonly associated with mutations in the KCNJ2 gene, which encodes a potassium ion channel essential for cardiac and muscle function. Management of Andersen–Tawil syndrome primarily focuses on controlling arrhythmias, preventing sudden cardiac death, and managing periodic paralysis episodes.
Clinical Features[edit]
Andersen–Tawil syndrome presents with a characteristic triad of:
- Cardiac Abnormalities – Prolongation of the QT interval, ventricular tachycardia, and increased risk of sudden cardiac events.
- Neuromuscular Manifestations – Recurrent episodes of muscle weakness, often triggered by hypokalemia.
- Dysmorphic Features – Distinctive craniofacial, skeletal, and limb anomalies.
Cardiac Abnormalities[edit]
The electrocardiogram (ECG) of an individual with Andersen–Tawil syndrome typically shows:
- Prolonged QT interval, increasing the risk of ventricular arrhythmias.
- Frequent premature ventricular contractions (PVCs), which may progress to ventricular tachycardia.
- Bidirectional ventricular tachycardia, a characteristic arrhythmia associated with ATS.
- Palpitations, dizziness, and syncope, especially during exercise or emotional stress.
While ATS is associated with long QT syndrome, the risk of sudden cardiac death is lower compared to other forms of congenital long QT syndromes.
Neuromuscular Manifestations[edit]
- Recurrent episodes of muscle weakness, lasting from minutes to hours.
- Weakness is typically triggered by low potassium levels (hypokalemia).
- Episodes may be provoked by exercise, stress, fasting, or certain medications.
- Some patients experience persistent muscle weakness between episodes.
Physical Abnormalities[edit]
The skeletal and craniofacial abnormalities seen in Andersen–Tawil syndrome include:
- Low-set ears and widely spaced eyes (hypertelorism).
- Micrognathia – A small lower jaw.
- Clinodactyly – Abnormal curvature of the fifth finger.
- Syndactyly – Fusion of two or more fingers or toes.
- Scoliosis – Abnormal curvature of the spine.
- Short stature and high-arched palate.
Genetics and Pathophysiology[edit]
Andersen–Tawil syndrome is caused by mutations in the KCNJ2 gene, which encodes the Kir2.1 potassium channel. This ion channel plays a crucial role in regulating:
- Cardiac repolarization, ensuring proper electrical conduction in the heart.
- Muscle membrane potential, preventing abnormal muscle contractions and weakness.
Genetic Inheritance[edit]
- ATS follows an autosomal dominant inheritance pattern.
- Some cases result from de novo mutations, meaning they occur spontaneously without a family history.
- Type 1 ATS (60% of cases) results from mutations in KCNJ2.
- Type 2 ATS (40% of cases) is genetically undefined but may involve mutations in KCNJ5.
Mechanisms of Disease[edit]
- Reduced Kir2.1 channel function results in abnormal potassium ion transport.
- Increased cardiac excitability leads to prolonged repolarization and susceptibility to arrhythmias.
- Muscle hyperexcitability and depolarization cause episodes of periodic paralysis.
Diagnosis[edit]
A diagnosis of Andersen–Tawil syndrome is based on a combination of:
- Clinical criteria (triad of cardiac, neuromuscular, and skeletal features).
- Electrocardiogram (ECG) findings (QT prolongation, bidirectional VT).
- Genetic testing to identify mutations in KCNJ2 or related genes.
Diagnostic Criteria[edit]
A diagnosis is likely if two of the following are present: 1. Periodic paralysis with episodes of muscle weakness. 2. Prolonged QT interval and ventricular arrhythmias. 3. Distinctive physical features such as clinodactyly, low-set ears, and scoliosis. 4. A family history of Andersen–Tawil syndrome.
Differential Diagnosis[edit]
Conditions that may mimic Andersen–Tawil syndrome include:
- Long QT syndrome (types 1–6) – Prolonged QT interval without skeletal abnormalities.
- Catecholaminergic polymorphic ventricular tachycardia (CPVT) – Exercise-induced ventricular arrhythmias.
- Familial periodic paralysis (hyperkalemic or hypokalemic forms) – Muscle weakness without cardiac abnormalities.
Treatment and Management[edit]
As a genetic disorder, Andersen–Tawil syndrome has no cure. However, treatment focuses on:
- Preventing life-threatening arrhythmias.
- Managing periodic paralysis episodes.
- Monitoring and treating skeletal abnormalities.
Cardiac Management[edit]
- Beta-blockers (e.g., propranolol) help prevent arrhythmias by reducing heart excitability.
- Flecainide and verapamil may be used for arrhythmia suppression.
- Implantable cardioverter-defibrillators (ICDs) are considered for high-risk patients who have experienced life-threatening arrhythmias.
Managing Periodic Paralysis[edit]
- Potassium supplementation during episodes can help restore muscle function.
- Acetazolamide (a carbonic anhydrase inhibitor) may reduce the frequency of attacks.
- Avoiding triggers such as fasting, stress, and excessive exercise is recommended.
Lifestyle Considerations[edit]
- Avoid medications that prolong the QT interval, such as amiodarone and sotalol.
- Mild to moderate exercise is encouraged, but competitive sports should be avoided due to arrhythmia risks.
- Regular monitoring with ECG and Holter monitoring is essential to track arrhythmia burden.
Prognosis[edit]
The prognosis of Andersen–Tawil syndrome varies depending on the severity of symptoms:
- Most individuals lead normal lives with appropriate treatment.
- Severe arrhythmias may increase the risk of sudden cardiac events, requiring close monitoring.
- Skeletal abnormalities can impact mobility and may require orthopedic interventions.
Epidemiology[edit]
Andersen–Tawil syndrome is an extremely rare condition, affecting approximately 1 in 1,000,000 individuals worldwide. Due to its rarity, many cases remain undiagnosed or misdiagnosed.
History[edit]
The condition was first described in 1971 by Dr. Ellen Damgaard Andersen, who documented the triad of symptoms. Further contributions were made by Dr. Rabi Tawil in 1994, leading to the modern understanding of the disorder.
See Also[edit]
External Links[edit]
| Syndromes | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
This syndrome related article is a stub.
|