Chronic paroxysmal hemicrania: Difference between revisions
CSV import |
CSV import Tags: mobile edit mobile web edit |
||
| Line 1: | Line 1: | ||
== Chronic Paroxysmal Hemicrania == | {{SI}} {{Infobox medical condition | ||
| name = Chronic paroxysmal hemicrania | |||
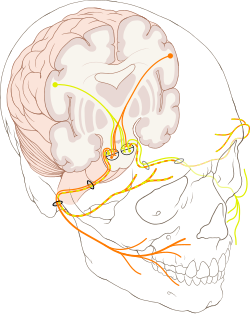
[[File:Cranial_nerve_VII.svg|thumb| | | image = [[File:Cranial_nerve_VII.svg|250px]] | ||
| caption = Diagram of the [[facial nerve]], which may be involved in the pathophysiology of chronic paroxysmal hemicrania. | |||
| field = [[Neurology]] | |||
| symptoms = Severe unilateral [[headache]], [[lacrimation]], [[rhinorrhea]], [[ptosis]], [[miosis]] | |||
| onset = Typically in [[adulthood]] | |||
| duration = 2 to 30 minutes per attack | |||
| frequency = More than 5 attacks per day | |||
| causes = Unknown, possibly related to [[trigeminal autonomic cephalalgias]] | |||
| risks = More common in [[females]] | |||
| diagnosis = Clinical evaluation, response to [[indomethacin]] | |||
| differential = [[Cluster headache]], [[migraine]], [[SUNCT syndrome]] | |||
| treatment = [[Indomethacin]] | |||
| medication = Indomethacin | |||
| prognosis = Good with treatment | |||
| frequency = Rare | |||
| deaths = None directly attributed | |||
}} | |||
[[Chronic paroxysmal hemicrania]] (CPH) is a rare type of [[headache]] disorder that is characterized by frequent, short-lasting attacks of severe unilateral pain. It is classified under [[trigeminal autonomic cephalalgias]], a group of primary headache disorders. The condition is notable for its excellent response to the non-steroidal anti-inflammatory drug [[indomethacin]]. | |||
The [[pathophysiology]] of CPH is not fully understood, but it is believed to involve the [[trigeminal nerve]] and autonomic nervous system. The [[facial nerve]] may also play a role, as depicted in the image provided. Diagnosis is primarily clinical, based on the characteristic symptoms and the patient's response to indomethacin. Differential diagnosis includes other headache disorders such as [[cluster headache]] and [[migraine]]. | |||
CPH is more common in [[females]] and typically begins in [[adulthood]]. The prognosis is generally good with appropriate treatment, and the condition is considered rare.== Chronic Paroxysmal Hemicrania == | |||
[[File:Cranial_nerve_VII.svg|thumb|left|Diagram of the cranial nerves, including the facial nerve (VII) which may be involved in headache disorders.]] | |||
'''Chronic Paroxysmal Hemicrania''' (CPH) is a rare primary headache disorder characterized by frequent, short-lasting, and severe unilateral headaches. It is classified under the group of [[trigeminal autonomic cephalalgias]] (TACs), which also includes [[cluster headache]]s and [[SUNCT syndrome]]. | '''Chronic Paroxysmal Hemicrania''' (CPH) is a rare primary headache disorder characterized by frequent, short-lasting, and severe unilateral headaches. It is classified under the group of [[trigeminal autonomic cephalalgias]] (TACs), which also includes [[cluster headache]]s and [[SUNCT syndrome]]. | ||
=== Clinical Features === | === Clinical Features === | ||
CPH is marked by attacks of severe pain that are strictly one-sided, typically around the eye, temple, or forehead. These attacks last from 2 to 30 minutes and can occur more than five times a day. The pain is often accompanied by autonomic symptoms such as conjunctival injection, lacrimation, nasal congestion, or rhinorrhea on the affected side. | CPH is marked by attacks of severe pain that are strictly one-sided, typically around the eye, temple, or forehead. These attacks last from 2 to 30 minutes and can occur more than five times a day. The pain is often accompanied by autonomic symptoms such as conjunctival injection, lacrimation, nasal congestion, or rhinorrhea on the affected side. | ||
=== Pathophysiology === | === Pathophysiology === | ||
The exact pathophysiology of CPH is not fully understood, but it is believed to involve dysfunction of the [[hypothalamus]] and the [[trigeminal nerve]] system. The involvement of the [[facial nerve]] (cranial nerve VII) is also considered due to the autonomic symptoms observed during attacks. | The exact pathophysiology of CPH is not fully understood, but it is believed to involve dysfunction of the [[hypothalamus]] and the [[trigeminal nerve]] system. The involvement of the [[facial nerve]] (cranial nerve VII) is also considered due to the autonomic symptoms observed during attacks. | ||
=== Diagnosis === | === Diagnosis === | ||
Diagnosis of CPH is primarily clinical, based on the characteristic pattern of headache attacks and response to treatment. It is important to differentiate CPH from other TACs and secondary causes of headache. Neuroimaging may be performed to rule out structural lesions. | Diagnosis of CPH is primarily clinical, based on the characteristic pattern of headache attacks and response to treatment. It is important to differentiate CPH from other TACs and secondary causes of headache. Neuroimaging may be performed to rule out structural lesions. | ||
=== Treatment === | === Treatment === | ||
CPH is uniquely responsive to [[indomethacin]], a nonsteroidal anti-inflammatory drug (NSAID). Indomethacin provides complete relief of symptoms in most patients, which is a key diagnostic criterion. Other treatments, such as [[verapamil]] or [[topiramate]], are generally ineffective. | CPH is uniquely responsive to [[indomethacin]], a nonsteroidal anti-inflammatory drug (NSAID). Indomethacin provides complete relief of symptoms in most patients, which is a key diagnostic criterion. Other treatments, such as [[verapamil]] or [[topiramate]], are generally ineffective. | ||
=== Prognosis === | === Prognosis === | ||
With appropriate treatment, the prognosis for individuals with CPH is excellent. Indomethacin effectively controls the attacks, allowing patients to lead normal lives. However, long-term use of indomethacin may be associated with gastrointestinal side effects, necessitating regular monitoring. | With appropriate treatment, the prognosis for individuals with CPH is excellent. Indomethacin effectively controls the attacks, allowing patients to lead normal lives. However, long-term use of indomethacin may be associated with gastrointestinal side effects, necessitating regular monitoring. | ||
== See Also == | |||
== | |||
* [[Cluster headache]] | * [[Cluster headache]] | ||
* [[Trigeminal neuralgia]] | * [[Trigeminal neuralgia]] | ||
* [[SUNCT syndrome]] | * [[SUNCT syndrome]] | ||
* [[Indomethacin]] | * [[Indomethacin]] | ||
{{Trigeminal autonomic cephalalgias}} | {{Trigeminal autonomic cephalalgias}} | ||
[[Category:Headaches]] | [[Category:Headaches]] | ||
[[Category:Neurology]] | [[Category:Neurology]] | ||
Latest revision as of 00:35, 6 April 2025

Editor-In-Chief: Prab R Tumpati, MD
Obesity, Sleep & Internal medicine
Founder, WikiMD Wellnesspedia &
W8MD medical weight loss NYC and sleep center NYC
| Chronic paroxysmal hemicrania | |
|---|---|
| |
| Synonyms | N/A |
| Pronounce | N/A |
| Specialty | N/A |
| Symptoms | Severe unilateral headache, lacrimation, rhinorrhea, ptosis, miosis |
| Complications | N/A |
| Onset | Typically in adulthood |
| Duration | 2 to 30 minutes per attack |
| Types | N/A |
| Causes | Unknown, possibly related to trigeminal autonomic cephalalgias |
| Risks | More common in females |
| Diagnosis | Clinical evaluation, response to indomethacin |
| Differential diagnosis | Cluster headache, migraine, SUNCT syndrome |
| Prevention | N/A |
| Treatment | Indomethacin |
| Medication | Indomethacin |
| Prognosis | Good with treatment |
| Frequency | Rare |
| Deaths | None directly attributed |
Chronic paroxysmal hemicrania (CPH) is a rare type of headache disorder that is characterized by frequent, short-lasting attacks of severe unilateral pain. It is classified under trigeminal autonomic cephalalgias, a group of primary headache disorders. The condition is notable for its excellent response to the non-steroidal anti-inflammatory drug indomethacin.
The pathophysiology of CPH is not fully understood, but it is believed to involve the trigeminal nerve and autonomic nervous system. The facial nerve may also play a role, as depicted in the image provided. Diagnosis is primarily clinical, based on the characteristic symptoms and the patient's response to indomethacin. Differential diagnosis includes other headache disorders such as cluster headache and migraine.
CPH is more common in females and typically begins in adulthood. The prognosis is generally good with appropriate treatment, and the condition is considered rare.== Chronic Paroxysmal Hemicrania ==

Chronic Paroxysmal Hemicrania (CPH) is a rare primary headache disorder characterized by frequent, short-lasting, and severe unilateral headaches. It is classified under the group of trigeminal autonomic cephalalgias (TACs), which also includes cluster headaches and SUNCT syndrome.
Clinical Features[edit]
CPH is marked by attacks of severe pain that are strictly one-sided, typically around the eye, temple, or forehead. These attacks last from 2 to 30 minutes and can occur more than five times a day. The pain is often accompanied by autonomic symptoms such as conjunctival injection, lacrimation, nasal congestion, or rhinorrhea on the affected side.
Pathophysiology[edit]
The exact pathophysiology of CPH is not fully understood, but it is believed to involve dysfunction of the hypothalamus and the trigeminal nerve system. The involvement of the facial nerve (cranial nerve VII) is also considered due to the autonomic symptoms observed during attacks.
Diagnosis[edit]
Diagnosis of CPH is primarily clinical, based on the characteristic pattern of headache attacks and response to treatment. It is important to differentiate CPH from other TACs and secondary causes of headache. Neuroimaging may be performed to rule out structural lesions.
Treatment[edit]
CPH is uniquely responsive to indomethacin, a nonsteroidal anti-inflammatory drug (NSAID). Indomethacin provides complete relief of symptoms in most patients, which is a key diagnostic criterion. Other treatments, such as verapamil or topiramate, are generally ineffective.
Prognosis[edit]
With appropriate treatment, the prognosis for individuals with CPH is excellent. Indomethacin effectively controls the attacks, allowing patients to lead normal lives. However, long-term use of indomethacin may be associated with gastrointestinal side effects, necessitating regular monitoring.